
Multi-modal approach with dye laser and CO2 laser for the resolution of vascularized acne scars: a case series
Highlight box
Key findings
• This study highlights the efficacy and the safety of the combined use of different laser devices as therapeutic alternative approach for vascularized acne scars treatment.
• This study emphasises the role of CO2 laser in skin remodelling and the efficacy of dye laser to reduce the inflammation and vascularization, especially for patients who do not respond to or cannot tolerate other therapies.
What is known and what is new?
• Literature demonstrated that dye laser is efficient in the treatment of keloids and hypertrophic scars. Similarly, the fractional CO2 laser has been widely used in atrophic scar remodelling with excellent results.
• As few published research are available on the combination of these two laser techniques, this study assesses the efficacy of combining dye and fractional CO2 lasers for acne resolution.
What is the implication, and what should change now?
• Our data confirmed the combination of dye and CO2 lasers is a winning strategy for the treatment of vascularized acne scars in young subjects. It is essential to create a clinical strategy designed for the patient, since everyone represents a unique case. This way, the patient’s perception of improvement after the laser sessions was very high as demonstrated by the Global Aesthetic Improvement Scale (GAIS) findings.
Introduction
As a prevalent condition of the pilosebaceous unit, acne vulgaris affects approximately 85% of people between the ages of 12 and 25 years (1,2). In 12–14% of cases with psychological, social, and emotional deficits, it frequently lasts into adulthood (3). Among the patients, 47% of them report having acne scars (4). These scars have an important vascular component. Trauma and inflammation are necessary to generate a scar. Normally, coagulation and inflammatory reactions occur immediately following trauma, followed by the release of several inflammatory factors, angiogenesis, and the activation of granulation and tissue repair processes (5). If this process steadily persists, hyperplasia will continue, and the scar will become hypertrophic (6).
The granulation tissue is composed of proliferating migrating fibroblasts and macrophages, newly formed blood vessels, embedded collagen matrix, and hyaluronic acid. The cells progressively shrink as a result of the remodeling process, and a scar finally appears (6).
Finding quick, efficient, and alternative treatments with fewer side effects is essential since acne vulgaris is linked to long-term medication use that often results in undesired side effects and germ resistance. Indeed, numerous treatment modalities for facial acne are available including topical and systemic drugs, hormonal treatment, physical therapy, and lasers (7). Due to its efficacy and safety, laser therapy has been a popular treatment option for acne vulgaris in recent years (3,4). Many lasers are used for acne including potassium titanyl phosphate (KTP), pulsed dye lasers (PDL), diode, erbium glass, neodymium-doped yttrium aluminum garnet (Nd: YAG) and CO2 lasers (10,600 nm) (8,9).
Another valuable technology is the flash-lamp pulsed dye laser (FPDL). It can emit at a wavelength of 595 nm, which is quite close to the maximal absorption of haemoglobin and oxyhaemoglobin, by pumping a rhodamine dye dissolved in a solvent with a flashlight (10). The fundamental idea of FPDL is selective photothermolysis, which targets specific skin structures for destruction while sparing adjacent tissue. Pulses of visible light with a wavelength of 585 or 595 nm are released by FPDL. To reduce the danger of scarring, the FPDL selectively photothermolyzes cutaneous blood vessels without harming the surrounding tissue (11,12).
Considering the characteristics of the dye laser, perfect for treating superficial vascular lesions, and vascularized acne scars, we believe that this device can be a feasible solution for treating these facial skin imperfections. Specifically, in this study, we suggest the combination of the 595 nm wavelength with a fractional CO2 laser to also ensure skin resurfacing and the best possible result. We present this case series in accordance with the AME Case Series reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-24-130/rc).
Case presentation
For this prospective case series study, 31 patients predominantly presenting vascularized acne scars with some active acne lesions were considered.
Patients were enrolled in in the Medical Europe Center Clinic between January 2022 and June 2022. They ranged between 20 and 35 years old. They presented Fitzpatrick’s skin phototypes from I to III. Patient’s exclusion criteria were: strong hypersensitivity to light, pregnancy, presence of precancerous lesions, intake of anticoagulants, retinoids, photo-sensitizers.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Ethical approval is not necessary as both study devices are already CE marked since 14/04/2021 and 28/03/2013. Written informed consent was obtained from the patients for the publication of this case series and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
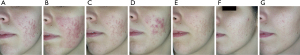
Two different wavelengths were used for the treatments. In Figure 1 the standard treatment timeline is shown. Depending on the characteristics of the clinical case, the treatment order or combination was modified. The therapeutical approach usually started with two dye laser treatments followed by two CO2 laser sessions. Depending on the clinical evaluation of the patient, the CO2 laser could be used during the whole treatment cycle while the dye laser can be extended until the 3rd session. In this study, the dye laser was mainly used for the resolution of skin inflammation and vascularization while CO2 was used for skin remodelling.

Specifically, a CO2 laser system (DuoGlide, DEKA M.E.L.A Srl, Florence, Italy) and a 595 nm pulse Dye Laser device (Synchro VasQ, DEKA, Florence, Italy) were used. The parameters for the CO2 wavelength source were D-Pulse (DP), spacing between columns of thermal damage (DOTs) of 750 µm, stack 1–2, and dwell time 1,800 µs. One pass over the body area was done. The fractioned scanning unit (µScan DOT) with a maximum scanning area of 15 mm × 15 mm was utilised to perform treatments.
To guarantee the best and safest outcome, a skin contact sensor was included with the device.
Moreover, dye laser sessions at 595 nm wavelength emission with a spot size of 12 mm, fluence of 6–7 J/cm2, and pulse duration of 0.5 ms, was performed. Clinical pictures were taken during the whole process and at the end of laser therapy (4 months follow-up). Possible side effects such as posttreatment erythema, itching, blisters, crusting, oedema or hyper/hypo pigmentation, were monitored.
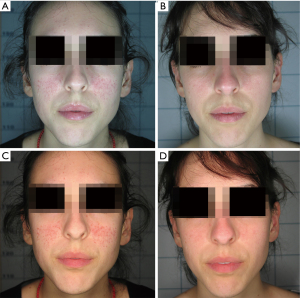
The progression of laser treatment was evaluated with a photographic assessment using a Canon digital camera and a polarized flash (Anthology system, DEKA-M.E.L.A., Calenzano, Italy). The images were standardized using the same camera, shooting settings, flash, ambient light and chin support, to ensure the same distance and to carefully monitor the outcomes obtained. Figures 2,3 document the progress of exemplificative cases of a young women presenting active acne vulgaris on the cheeks.
During the session, a jet of cool air (Zimmer Cryo6) was given to the treated area to minimise inflammation and oedema.
Using a 4-point Global Aesthetic Improvement Scale (GAIS) (none: 0, slight: 1, mild: 2, excellent: 3) (13) to assess the treatment outcomes, 77% of patients claimed it was “excellent”, 16% “mild” and 7% “slight”.
The healing process after treatment with dye involves standard consequences such as purpura for 7–10 days, while after treatment with the CO2 laser, a widespread redness lasting 4–5 days was present. Moreover, pharmacological therapy pre-treatment with antivirals and post-treatment with a mousse-like solution to hydrate the skin was provided.
Discussion
Propionibacterium acnes is the main cause of acne vulgaris, one of the most frequent chronic skin diseases. It colonises hair follicles and affects pilosebaceous units on the face, neck, chest, and back, causing increased sebum production, altered keratinization, and inflammation.
Atrophic and hypertrophic scars are the two main forms of scars, which differ in the amount of collagen gained or lost. Atrophic scars, or scars associated with a loss of collagen, constitute eighty to ninety percent of acne scarring patients; hypertrophic scars and keloids are found in a smaller percentage of cases. The prevalence of atrophic acne scars is 3:1 greater than that of keloids and hypertrophic scars. They’ve been categorized into rolling, boxcar, and ice pick subtypes (14).
With these premises, there is a great need to develop new therapeutic options, especially for patients who are not well-responders to conventional treatments for acne vulgaris. Moreover, some patients develop antibiotic resistance, and others are not suitable candidates for pharmacotherapy.
In order to individualize acne care based on the possible advantages and dangers of therapy, the degree, location, and intensity of acne involvement, treatment costs, patient preferences, and other considerations, collaborative decision-making is crucial considering the variety of acne treatment options (15).
Dermabrasion, systemic antibiotics, hormonal agents, oral isotretinoin, physical modalities complementary and alternative medicine, dietary, chemical peels, punch techniques, tissue-augmenting agents, needling, subcision, fat transplantation, laser and light-based devices, silicone gel, intralesional steroid therapy, cryotherapy, and surgery or combinations of them represent the current clinical therapies for atrophic acne scars management (16).
However, icepick and rolling scars, require multiple peelings for a complete disappearance with the needed of additional homecare treatment using topical retinoids and alpha hydroxy acids (17,18).
Although oral antibiotics such as oral doxycycline or minocycline have been approved by the Food and Drug Administration (FDA) for the management of acne, tetracycline class antibiotics should be avoided in pregnant or breastfeeding patients for their potential risk of permanent tooth discoloration and inhibition of bone growth in the fetus or newborn (19).
Furthermore, following dermabrasion treatments individuals with darker skin tones may develop blotchiness or persistent skin discoloration (14).
Concerning the use of isotretinoin, literature demonstrate that it causes delayed reepithelialization and the development of hypertrophic scars (20).
Skin needling is another recently proposed procedure; however, it is not recommended if there has been previous use of anticoagulants, presence of active skin infections, collagen injections or other injectable fillers in the preceding six months, or a personal or family history of hypertrophic and keloid scars (21,22).
Local cryotherapy has long been reported to be useful in the treatment of acne vulgaris as it allows for faster involution of acne compared to topical medications. Nevertheless, a number of disadvantages, such as discomfort during the procedure, skin atrophy and hypo/hyperpigmentation have restricted its application (23).
Microvessel blockage has been discovered to accompany scar regression, highlighting the crucial roles that microvessels play in scar reduction. Pathological scarring is a sort of hyperactive vascular reactivity to trauma. As a result, treatments that focus on the vascular component, including PDL or vascular endothelial growth factor antibodies, have proven to be highly effective. Furthermore, treatments that target collagen, including collagenase and fractional CO2 laser, have shown promise results for the treatment of scars since current treatments typically fail to treat the collagen mass associated with the scar (24). Indeed, CO2 fractional laser systems have been on the market for a long time for acne management and there is proportionality between the energy supplied and the depth reached, which are consolidated over time. Deep scars need more ablation and thus more energy. Indeed, the most severe scars request laser action depths >1 mm, and this can be accomplished by raising the ablative power, which is connected to the energy provided by the system (25-28).
In this scenario, several laser and light-based devices have become popular for treating mild-to-severe acne because they are safe, effective, and convenient. While their efficacy and safety have been proven, the outcomes have been inconsistent. However, the benefits of light- and laser-based therapies include patient compliance, prevention of antibiotic resistance, and a shorter treatment duration. Serious long-term side effects are uncommon, and most adverse effects are mild and manageable. Nevertheless, as several treatment sessions are sometimes needed to observe a clinical improvement, some patients may find the cost of laser and light-based acne care techniques exorbitant. When treating acne, laser treatments—especially ablative ones—may exacerbate the condition. Even though these treatments are not approved in many states, more research and understanding of alternative laser and light-based approaches to acne therapy will lead to better recommendations on how to use them (29).
Our clinical experience and other reports allowed us to treat patients with lasers, even though intense PDL is a non-ablative technology that is typically used in vascular malformation therapy (10). Moreover, it was reported by Al-Mohamady Ael-S et al. [2016] that PDL is efficient in the treatment of keloids and hypertrophic scars with almost no difference compared to Nd:YAG lasers. This is due to its characteristic of selectively targeting haemoglobin and coagulating microvasculature in the papillary and reticular dermis and inhibiting nutrient supply to the scar (30). Similarly, the CO2 laser has been widely used in atrophic scar remodelling with excellent results (31).
Indeed, our data confirmed the combination of dye and CO2 lasers is a winning strategy for the treatment of vascularized acne scars in young subjects. We believe that it is crucial to build a clinical strategy designed for the patient since everyone represents a unique case. This way, the patient’s perception of improvement after the laser sessions was very high as demonstrated by the GAIS results.
The combination of dye and fractional CO2 laser showed good efficacy in the treatment of patients affected by vascularized acne scars with no severe complications and it can be recommended in clinical application.
The study’s main limitation was the lack of comparison between CO2 and dye laser treatments vs. dye and CO2 treatments alone in the same patient population.
Conclusions
In conclusion, early treatment of vascularized acne scars is crucial to prevent additional aggravation and chronicization of the condition. The combination of different laser devices can be a promising therapeutic alternative for acne resolution. Remodelling the skin with the CO2 laser wavelength and reducing the inflammation and vascularization with the dye laser could be particularly helpful, especially for patients who do not respond to or cannot tolerate other therapies. To confirm the effectiveness of this combined laser approach in treating acne, more research with a larger sample size may be helpful. This would permit comparisons between a combination therapy group, patients treated with a dye laser alone, and patients treated with CO2.
Acknowledgments
None.
Footnote
Reporting Checklist: The authors have completed the AME Case Series reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-24-130/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-24-130/prf
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-24-130/coif). B.M.P., I.F., and T.Z. are employed at El.En. Group. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for the publication of this case series and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lynn DD, Umari T, Dunnick CA, et al. The epidemiology of acne vulgaris in late adolescence. Adolesc Health Med Ther 2016;7:13-25. [Crossref] [PubMed]
- Moftah NH, Mansour AM, Ibrahim SMA. Clinical evaluation of efficacy of intralesional platelet-rich plasma injection versus 1064 nm long-pulsed Neodymium:YAG laser in the treatment of inflammatory acne vulgaris in adolescent and post-adolescent patients: a prospective randomized split-face comparative study. Lasers Med Sci 2022;37:2471-8. [Crossref] [PubMed]
- Becker M, Wild T, Zouboulis CC. Objective assessment of acne. Clin Dermatol 2017;35:147-55. [Crossref] [PubMed]
- Liu L, Xue Y, Chen Y, et al. Prevalence and risk factors of acne scars in patients with acne vulgaris. Skin Res Technol 2023;29:e13386. [Crossref] [PubMed]
- Greaves NS, Ashcroft KJ, Baguneid M, et al. Current understanding of molecular and cellular mechanisms in fibroplasia and angiogenesis during acute wound healing. J Dermatol Sci 2013;72:206-17. [Crossref] [PubMed]
- Shi C, Zhu J, Yang D. The pivotal role of inflammation in scar/keloid formation after acne. Dermatoendocrinol 2017;9:e1448327. [Crossref] [PubMed]
- Tan AU, Schlosser BJ, Paller AS. A review of diagnosis and treatment of acne in adult female patients. Int J Womens Dermatol 2018;4:56-71. [Crossref] [PubMed]
- Gold MH, Weiss E, Biron J. Novel laser hair removal in all skin types. J Cosmet Dermatol 2023;22:1261-5. [Crossref] [PubMed]
- Ibrahim AM, Omar GAB, Hamdino M. Long-pulsed Nd: YAG laser (1064 nm) versus intralesional botulinum toxin type (A) in acne vulgaris therapy: a split face study. Int J Dermatol 2023;62:822-30. [Crossref] [PubMed]
- Cannarozzo G, Sannino M, Tamburi F, et al. Flash-lamp pulsed-dye laser treatment of keloids: results of an observational study. Photomed Laser Surg 2015;33:274-7. [Crossref] [PubMed]
- Giovanni C, Marina PB, Tiziano Z. A retrospective 10 years- experience overview of dye laser treatments for vascular pathologies. Skin Res Technol 2023;29:e13427. [Crossref] [PubMed]
- Bennardo L, Fasano G, Tamburi F, et al. Sequential Use of CO(2) Laser Prior to Nd:YAG and Dye Laser in the Management of Non-Facial Warts: A Retrospective Study. Medicina (Kaunas) 2022;58:115. [Crossref] [PubMed]
- Piccolo D, Crisman G, Gallo G, et al. Long Pulsed 1064 nm Nd:YAG Laser Treatment for Skin Laxity and Wrinkle Reduction: Evaluation of New Handpiece and "in Motion" Setting Technique-A Case Series Study. Photobiomodul Photomed Laser Surg 2023;41:297-9. [Crossref] [PubMed]
- Fabbrocini G, Annunziata MC, D'Arco V, et al. Acne scars: pathogenesis, classification and treatment. Dermatol Res Pract 2010;2010:893080. [Crossref] [PubMed]
- Reynolds RV, Yeung H, Cheng CE, et al. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol 2024;90:1006.e1-1006.e30. [Crossref] [PubMed]
- Connolly D, Vu HL, Mariwalla K, et al. Acne Scarring-Pathogenesis, Evaluation, and Treatment Options. J Clin Aesthet Dermatol 2017;10:12-23. [PubMed]
- Goodman GJ. Management of post-acne scarring. What are the options for treatment?. Am J Clin Dermatol 2000;1:3-17. [Crossref] [PubMed]
- Goodman GJ. Postacne scarring: a review of its pathophysiology and treatment. Dermatol Surg 2000;26:857-71. [Crossref] [PubMed]
- Zaenglein AL, Pathy AL, Schlosser BJ, et al. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol 2016;74:945-73.e33. [Crossref] [PubMed]
- Guadanhim LR, Gonçalves RG, Bagatin E. Observational retrospective study evaluating the effects of oral isotretinoin in keloids and hypertrophic scars. Int J Dermatol 2016;55:1255-8. [Crossref] [PubMed]
- Fernandes D. Minimally invasive percutaneous collagen induction. Oral Maxillofac Surg Clin North Am 2005;17:51-63. vi. [Crossref] [PubMed]
- Fabbrocini G, Fardella N, Monfrecola A, et al. Acne scarring treatment using skin needling. Clin Exp Dermatol 2009;34:874-9. [Crossref] [PubMed]
- Rho NK. Revisiting the Role of Local Cryotherapy for Acne Treatment: A Review and Update. J Clin Med 2022;12:26. [Crossref] [PubMed]
- Yuan B, Upton Z, Leavesley D, et al. Vascular and Collagen Target: A Rational Approach to Hypertrophic Scar Management. Adv Wound Care (New Rochelle) 2023;12:38-55. [Crossref] [PubMed]
- Scarcella G, Pieri L, Fusco I. Skin Fractional Scar Treatment with a New Carbon Dioxide Scanner: Histological and Clinical Evaluation. Photobiomodul Photomed Laser Surg 2022;40:424-32. [Crossref] [PubMed]
- Sasaki GH, Travis HM, Tucker B. Fractional CO2 laser resurfacing of photoaged facial and non-facial skin: histologic and clinical results and side effects. J Cosmet Laser Ther 2009;11:190-201. [Crossref] [PubMed]
- Oni G, Robbins D, Bailey S, et al. An in vivo histopathological comparison of single and double pulsed modes of a fractionated CO(2) laser. Lasers Surg Med 2012;44:4-10. [Crossref] [PubMed]
- Waibel JS, Rudnick A, Shagalov DR, et al. Update of Ablative Fractionated Lasers to Enhance Cutaneous Topical Drug Delivery. Adv Ther 2017;34:1840-9. [Crossref] [PubMed]
- Li MK, Liu C, Hsu JTS. The Use of Lasers and Light Devices in Acne Management: An Update. Am J Clin Dermatol 2021;22:785-800. [Crossref] [PubMed]
- Al-Mohamady Ael-S. Ibrahim SM, Muhammad MM. Pulsed dye laser versus long-pulsed Nd:YAG laser in the treatment of hypertrophic scars and keloid: A comparative randomized split-scar trial. J Cosmet Laser Ther 2016;18:208-12. [Crossref] [PubMed]
- Gotkin RH, Sarnoff DS, Cannarozzo G, et al. Ablative skin resurfacing with a novel microablative CO2 laser. J Drugs Dermatol 2009;8:138-44. [PubMed]
Cite this article as: Cannarozzo G, Pennati BM, Fusco I, Campolmi P, Zingoni T. Multi-modal approach with dye laser and CO2 laser for the resolution of vascularized acne scars: a case series. AME Case Rep 2025;9:36.


