
Pilomatricoma of the breast similar to breast cancer on ultrasound and elastography: a case report
Highlight box
Key findings
• We report a case of pilomatricoma of the breast with similar characteristics to breast cancer on ultrasound and elastography.
What is known and what is new?
• Pilomatricomas occurring on the breast may present clinically and ultrasonographically similar to breast cancer.
• Pilomatricomas and breast cancer have different origin layers that can be observed on ultrasound.
What is the implication, and what should change now?
• Pilomatricomas and breast cancer have different origin layers, necessitating a focus on distinguishing between the two entities based on layer-derived differentiation on ultrasound and elastography.
Introduction
Pilomatricoma, also known as calcifying epithelioma of Malherbe, is a benign tumor originating from human hair follicle stem cells and commonly observed in adolescents (though it can occur at any age). Pilomatricomas can arise in any region with hair follicles, typically presenting as solitary lesions, predominantly affecting the facial region. Clinically, they manifest as firm, painless nodules, with both pathological and ultrasonographic findings often revealing calcifications, which may be coarse or punctate (1). Reports on pilomatricoma located in the breast are scarcer, thus our understanding of its ultrasound and elastography characteristics is even more limited. The lack of specific imaging features poses a challenge to preoperative diagnosis. Herein, we report a case of pilomatricoma located on the breast, characterized by multiple punctate hyperechoic foci internally, presenting as a firm, non-tender mass on palpation and elastography. Additionally, the rapid enlargement of the mass within a short period raised clinical suspicion of breast cancer, leading to surgical excision, which subsequently confirmed pilomatricoma through histopathological examination. We present this case in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-24-103/rc).
Case presentation
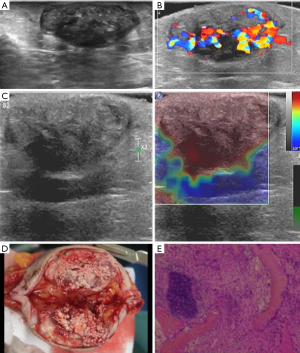
A 47-year-old female discovered a pea-sized lump in her left breast a year ago, which was firm, non-tender, and mobile. Without seeking treatment, she experienced pain in the lump two weeks before presentation. After applying an unspecified anti-inflammatory ointment, the lump markedly increased to the size of a pigeon egg, prompting her hospital visit. On examination, the lump was firm, non-tender, and mobile, with normal overlying skin. Breast ultrasound examination was performed using a high-frequency linear array transducer (el18-4). Breast ultrasonography revealed a well-defined hypoechoic solid mass with multiple punctate hyperechoic foci internally and abundant vascularity. Strain elastography reveals that the lesion has a hard texture. According to the American College of Radiology Breast Imaging-Reporting and Data System (ACR BI-RADS) classification, the lesion was classified into category 4A. The differential diagnosis included pilomatricoma and breast cancer. However, the ultrasound indicated that the lesion was situated between the dermis and subcutaneous fat layers, without invading the posterior breast glandular tissue, suggesting pilomatricoma originating from the skin. Despite clinical suspicion of breast cancer due to the firm texture and rapid enlargement of the mass, along with multiple punctate hyperechoic foci on ultrasonography, surgical excision was performed after obtaining informed consent from the patient, confirming pilomatricoma on histopathology (Figure 1). All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Publication of this case report and accompanying images was exempt from patient consent according to The Affiliated First Hospital of Ningbo University ethics committee (approval number 2024-120RS).
Discussion
Pilomatricoma, initially described by Malherbe in 1880 and named calcifying epithelioma, is a benign tumor derived from human hair follicle stem cells. It slightly predominates in females, with a ratio of approximately 1.1:1 compared to males (1).
The exact pathogenesis underpinning pilomatrixoma is still unclear. Some studies have shown that b-catenin is involved in the development of pilomatricoma (2,3). BCL2 also plays an important role in the occurrence of pilomatricoma (4).
Pilomatricomas can occur at any age, with a peak incidence in adolescents, possibly related to vigorous metabolism and development of hair cells and subcutaneous appendages during adolescence (5). Our case, occurring in an older age group, which is more prone to breast cancer and located on the breast, raised suspicion for breast cancer. Pilomatricomas can arise in any area with hair follicles, often as solitary lesions, commonly affecting the facial region, neck, and upper extremities, with breast involvement being rare. Clinically, they typically present as well-defined, firm, painless nodules, often adherent to the skin, with good mobility, and a normal or slightly erythematous or violaceous surface. Pathologically, the tumor appears subcutaneously with clear margins, mostly encapsulated, gray-white in color, and firm. On cut section, it reveals gray-white solid tissue with calcifications, imparting a gritty sensation upon sectioning. Microscopically, the tumor is located in the reticular dermis, often encapsulated by connective tissue, composed mainly of basaloid cells and shadow cells. The proportion of these cells indicates the tumor development stage (6). The stroma may show foreign body giant cell reactions, localized calcifications, and inflammatory cell infiltration. Complete excision of the mass usually results in a good prognosis, with rare occurrences of malignant transformation or distant metastasis.
Ultrasonographically, pilomatricomas typically appear as well-defined, solid masses located at the junction of the dermis and subcutaneous fat layers, with round or oval shapes, heterogeneous echogenicity, often accompanied by calcifications, either scattered or coarse (7). Peripheral fatty tissue around the lesion may show increased echogenicity due to calcifications stimulating foreign body giant cell reaction and inflammatory cell infiltration. Color Doppler flow imaging usually demonstrates abundant blood flow around and within the lesion. Pilomatricoma exhibits a hard texture in strain elastography (8). Preoperatively, pilomatricomas, especially those occurring in breast tissue, pose diagnostic challenges. In our case, the presence of scattered punctate hyperechoic foci, abundant blood flow, and firm texture on elastography, along with the patient’s older age, rapid recent growth of the mass, mimicking breast cancer, highlighted the importance of distinguishing between the two entities. The crucial distinguishing feature from breast cancer lies in delineating the origin layers: the lesion located between the dermis and subcutaneous fat layers, without invasion into the posterior breast glandular tissue, suggesting a non-breast glandular origin, necessitating consideration of a skin-derived pilomatricoma. Xue et al. (9) emphasized the significance of layer-derived differentiation in distinguishing benign and malignant breast masses, where masses located within the fatty layer with smooth margins are generally benign, consistent with our report of this case of breast pilomatricoma.
Conclusions
Pilomatricomas occurring on the breast may present clinically and ultrasonographically similar to breast cancer, necessitating a focus on distinguishing between the two entities based on layer-derived differentiation on ultrasound and elastography.
Acknowledgments
None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-24-103/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-24-103/prf
Funding: None.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-24-103/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Publication of this case report and accompanying images was exempt from patient consent according to The Affiliated First Hospital of Ningbo University ethics committee (approval number 2024-120RS).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hwang JY, Lee SW, Lee SM. The common ultrasonographic features of pilomatricoma. J Ultrasound Med 2005;24:1397-402. [Crossref] [PubMed]
- Park SW, Suh KS, Wang HY, et al. beta-Catenin expression in the transitional cell zone of pilomatricoma. Br J Dermatol 2001;145:624-9. [Crossref] [PubMed]
- Ha SJ, Kim JS, Seo EJ, et al. Low frequency of beta-catenin gene mutations in pilomatricoma. Acta Derm Venereol 2002;82:428-31. [Crossref] [PubMed]
- Farrier S, Morgan M. bcl-2 expression in pilomatricoma. Am J Dermatopathol 1997;19:254-7. [Crossref] [PubMed]
- Lan MY, Lan MC, Ho CY, et al. Pilomatricoma of the head and neck: a retrospective review of 179 cases. Arch Otolaryngol Head Neck Surg 2003;129:1327-30. [Crossref] [PubMed]
- Kaddu S, Soyer HP, Hödl S, et al. Morphological stages of pilomatricoma. Am J Dermatopathol 1996;18:333-8. [Crossref] [PubMed]
- Choo HJ, Lee SJ, Lee YH, et al. Pilomatricomas: the diagnostic value of ultrasound. Skeletal Radiol 2010;39:243-50. [Crossref] [PubMed]
- Marino MA, Ascenti G, Cardia R, et al. Pilomatrixoma of the right thigh: Sonographic-pathologic correlation in a young man. Radiol Case Rep 2020;15:230-3. [Crossref] [PubMed]
- Xue N, Zhang S. Analysis of the accuracy of ultrasound elastography and BI-RADS classification of breast masses located within the superficial fat layer of the glands. Gland Surg 2022;11:1722-9. [Crossref] [PubMed]
Cite this article as: Zhu S, Xue N. Pilomatricoma of the breast similar to breast cancer on ultrasound and elastography: a case report. AME Case Rep 2025;9:46.


