
Chorioretinal involvement in a patient with paracoccidioidomycosis: a case report
Highlight box
Key findings
• This case report presents a rare instance of ocular paracoccidioidomycosis in a 58-year-old male with systemic fungal infection.
• The patient exhibited chorioretinal lesions and palpebral involvement without visual acuity loss.
What is known, and what is new?
• Ocular manifestations of paracoccidioidomycosis are extremely rare but can lead to serious complications if not diagnosed early.
• This report highlights the importance of routine ophthalmologic evaluations in patients with systemic fungal infections, as early intervention can prevent vision loss.
What is the implication, and what should change now?
• When evaluating chorioretinal lesions, ophthalmologists should consider paracoccidioidomycosis as a differential diagnosis in endemic regions.
• Early diagnosis and appropriate systemic antifungal treatment can significantly improve ocular lesions and preserve vision.
Introduction
Paracoccidioidomycosis, caused by the dimorphic fungus Paracoccidioides spp., is a systemic mycosis endemic in Mexico, South, and Central America (1). It predominantly affects male rural workers and is typically acquired through the inhalation of conidia or oral mucosal inoculation (1). The lungs are the primary organs affected, with extrapulmonary manifestations including lesions on the facial skin, oral, laryngeal, and pharyngeal mucosa, as well as potential lymph node involvement (1). Ocular manifestations are rare, likely due to hematological dissemination, with only a few cases reported, primarily in Brazil (2-4). Eyelid and conjunctival involvement are more common than corneal or retinal involvement (2,5). This case is unique for documenting simultaneous palpebral associated with chorioretinal lesions without visual acuity loss, a rare presentation. It underscores the importance of ophthalmologic evaluation in systemic fungal infections to ensure early diagnosis and treatment, preventing severe outcomes. We presented this case in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-24-201/rc).
Case presentation
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
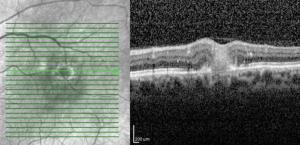
A 58-year-old male residing in Brazil with a histopathologic diagnosis of paracoccidioidomycosis had an ophthalmologic evaluation in our outpatient clinic due to palpebral lesions. The patient had a history of unintentional weight loss, chronic cough, and cutaneous lesions on the eyelid, nasal and maxillary regions for 8 months. Ophthalmic evaluation revealed nodular palpebral lesions in the right superior region with a medial infiltrative lesion, as well as medial superior and inferior madarosis with inferior displacement of the lacrimal duct. Visual acuity remained unaffected, 20/20 in both eyes (OU). Anterior biomicroscopy of right eye (OD) revealed mild keratitis. Fundoscopic examination of left eye (OS) showed an elevated white/yellowish lesion approximately 1/2 disc area superiorly temporal to the macula, accompanied by perilesional hard exudates and microhemorrhages (Figure 1). Optical coherence tomography (OCT) of OS revealed a chorioretinal lesion with disruption of retinal layers, suggesting fungal lesions (Figure 2). The diagnosis of paracoccidioidomycosis had been made one week prior to the ophthalmological consultation through a skin biopsy performed by the dermatology department of our hospital. Due to the history of consumptive syndrome, Tuberculosis was initially suspected, but tuberculin skin test and tuberculosis sputum culture were negative. In this context, the dermatology department performed a biopsy of the face cutaneous lesions to elucidate the diagnosis (Figure 3). Histopathological examination revealed a thick, birefringent fungal wall and the characteristic multiple budding of Paracoccidioides spp., elucidating the diagnosis of paracoccidioidomycosis. He had a history of tobacco use and alcoholism and was non-compliant with oral medication for the established infection. Due to previous oral medication non-compliance, the patient was hospitalized for a treatment with amphotericin B 3 mg/kg. Initial treatment with amphotericin B was discontinued after 15 days due to acute renal injury and was replaced with trimethoprim/sulfamethoxazole, planned for 12 months. Weekly evaluations showed progressive improvement of chorioretinal lesions, presumptively diagnosed as chorioretinitis secondary to systemic paracoccidioidomycosis infection. However, the patient was lost to follow-up after 3 months of treatment with trimethoprim/sulfamethoxazole, during which time the progressive improvement of the chorioretinal lesions was observed.


Discussion
Although ocular manifestations are rare in paracoccidioidomycosis, this case highlights the importance of ophthalmologic evaluation in patients with this diagnosis. Paracoccidioidomycosis should always be regarded as a systemic infection, as direct skin inoculation is rare (1). Even isolated eyelid lesions typically result from lymphatic extension or hematogenous dissemination of the fungus (1). The primary entry point for Paracoccidioides spp. is the lungs (1). Our case was compared to similar cases of ocular paracoccidioidomycosis, wherein the palpebral, conjunctival, and corneal regions were involved (2,4,6). The description of palpebral lesions revealed shallow ulcerated lesions with an infiltrated base and a vegetative bed with hemorrhagic petechiae. Histopathologic examination of the skin lesions demonstrated granulomatous inflammatory infiltrates with the presence of fungi. Despite the limited description of the palpebral lesion in our case, the formation of granulomas was a commonality, affecting either the superior, inferior, or both eyelids of the affected eye. Keratitis resulting from inferior exposure was identified as a shared characteristic across all cases, and one patient exhibited madarosis, mirroring the findings observed in our case (2,4,6).
Retinal involvement in our case was a single chorioretinal lesion superiorly temporal to the macula on OS, with disruption of retinal layers and hard exudates with microhemorrhage (Figure 1). A case report published by Igami et al. described a younger patient with a similar background (rural worker) presenting with systemic paracoccidioidomycosis with ophthalmic findings limited to the choroid and retina (2). The patient’s vision acuity was compromised, <20/400 on the affected eye. An ophthalmic exam revealed corneal fine-pigmented keratotic precipitates inferiorly, +2 cells in the anterior chamber, and +2 vitreous cells in the slit-lamp. In addition, their report described a perimacular choroidal granuloma with multiple whitish spots and mid-periphery exudative retinal detachment of OS. Fluorescein angiography of the affected eye showed hyperfluorescence in the choroidal lesion area with late leakage. This description is considerably similar to our case, although our lesion was smaller and showed no signs of retinal detachment (Figure 4).
A case report by Finamor et al. detailed a 25-year-old pregnant woman with AIDS who presented with systemic paracoccidioidomycosis affecting both the central nervous system and the eye (3). The patient exhibited severe inflammation in the OD, involving the choroid, retina, and optic disk, which rapidly led to retinal detachment, iris neovascularization, and neovascular glaucoma. The OS was unaffected. Magnetic resonance imaging revealed a focal hypodense ring-enhancing lesion in the brain. Initial serological tests for Toxoplasma gondii were negative, but the parasite was detected in the vitreous sample through polymerase chain reaction. Despite partial response to specific treatment for toxoplasmosis, the patient progressed to a blind, painful eye, resulting in enucleation. Histopathological studies of the eye and oropharynx identified Paracoccidioides spp. Subsequent treatment with trimethoprim-sulfamethoxazole yielded a satisfactory outcome, including a reduction in the size of the brain lesion.
The case by Finamor et al. highlights the importance of considering ocular paracoccidioidomycosis in the differential diagnosis of ocular inflammation in patients with acquired immune deficiency syndrome (AIDS), especially when presenting with atypical features and negative serologies for more common pathogens (3). In all cases, autoimmune, neoplastic, and inflammatory conditions should be considered to rule out other possible causes of the ocular findings, including serologic tests for toxoplasmosis, human immunodeficiency virus (HIV), syphilis, hepatitis, tuberculosis, and cytomegalovirus. Recognizing that immunocompromised individuals face an elevated susceptibility to systemic disseminated fungal infections is crucial, as they are predisposed to experiencing more severe manifestations of ocular paracoccidioidomycosis.
Effective pharmacological treatment can be achieved with prolonged use (>3 months) itraconazole, trimethoprim-sulfamethoxazole, and voriconazole or a median of 15 days of amphotericin B. Prednisolone is sometimes used to aid in reducing inflammation (7,8).
This case report highlights the importance of considering Paracoccidioides spp. in the differential diagnosis of ocular lesions, particularly in patients with unexplained symptoms who reside in or have traveled to endemic regions (1,5). Diagnostic challenges in resource-limited settings emphasize the need for thorough clinical and epidemiological evaluation (1,5). Early recognition and treatment are especially critical for immunocompromised individuals, who face a higher risk of severe manifestations (1,5). Further research on the ocular manifestations of paracoccidioidomycosis is warranted to enhance diagnostic accuracy and optimize management strategies for these rare cases.
Conclusions
This case underscores the importance of including an ophthalmological evaluation in managing patients diagnosed with paracoccidioidomycosis, even when ocular manifestations are rare. Timely diagnosis and treatment of ocular involvement, as demonstrated by the chorioretinal lesions in this patient, can prevent significant visual impairment. Systemic antifungal therapy, including amphotericin B and sulfamethoxazole-trimethoprim, proved effective in controlling the disease’s ocular and systemic manifestations. Early intervention in such cases can result in favorable outcomes and improved prognosis.
Acknowledgments
None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-24-201/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-24-201/prf
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-24-201/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Cordova LA, Torres J. Paracoccidioidomycosis. StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2024, StatPearls Publishing LLC.; 2024.
- Igami TZ, Solano F, Preti RC, et al. Retinal involvement of Paracoccioidomycosis: A Case Report. Trop Med Health 2012;40:149-53. [Crossref] [PubMed]
- Finamor LP, Muccioli C, Martins MC, et al. Ocular and central nervous system paracoccidioidomycosis in a pregnant woman with acquired immunodeficiency syndrome. Am J Ophthalmol 2002;134:456-9. [Crossref] [PubMed]
- Gervini RL, Vettorato G, Lecompte SM, et al. Ocular paracoccidioidomycosis: report of two cases and review of literature. Anais Brasileiros de Dermatologia 2004;79:69-78. [Crossref]
- Taborda CP, Travassos LR, Benard G. Paracoccidioidomycosis. In: Zaragoza Ó, Casadevall A. editors. Encyclopedia of Mycology. Oxford: Elsevier; 2021:654-75.
- Bovo LB, Pierre-Filho Pde T, Carvalho Fdo C, et al. Disseminated paracoccidioidomycosis with chorioretinal involvement. Eye (Lond) 2005;19:1021-3. [Crossref] [PubMed]
- Shikanai-Yasuda MA, Mendes RP, Colombo AL, et al. Brazilian guidelines for the clinical management of paracoccidioidomycosis. Rev Soc Bras Med Trop 2017;50:715-40. [Crossref] [PubMed]
- Borges SR, Silva GM, Chambela Mda C, et al. Itraconazole vs. trimethoprim-sulfamethoxazole: A comparative cohort study of 200 patients with paracoccidioidomycosis. Med Mycol 2014;52:303-10. [Crossref] [PubMed]
Cite this article as: Faneli AC, Morello PC, Neto PFS, Oliveira RDC, Muccioli C. Chorioretinal involvement in a patient with paracoccidioidomycosis: a case report. AME Case Rep 2025;9:55.



