
Difficult insertion of a transesophageal echocardiography probe for cardiac surgery not only before but also immediately after thyroid goiter resection in a patient with chronic esophageal compression by the goiter: a case report
Highlight box
Key findings
• Dilatation of the chronically compressed esophagus could be inadequate at least immediately after thyroid surgery.
• When usual transesophageal echocardiography (TEE) probe placement is difficult, alternative methods for assessing the mitral valve should be considered.
What is known and what is new?
• Extrinsic compression of the esophagus is one of the causes of difficult TEE probe insertion.
• It would take long time to improve the esophageal stricture caused by external pressure from thyroid goiter.
What is the implication, and what should change now?
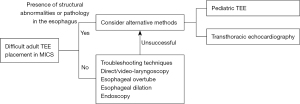
• Our proposed roadmap could provide recommended management strategy for the difficulties of TEE probe insertion for minimally invasive cardiac surgery in mitral valvuloplasty.
Introduction
Transesophageal echocardiography (TEE) is an essential tool during minimally invasive cardiac surgery (MICS), although inserting a TEE probe is sometimes challenging. We experienced a case of an esophageal stenosis resulting from extrinsic compression of the esophagus by goiter, which made insertion of an adult TEE probe impossible not only before but also immediately after goiter resection. This is a rare case of the difficult insertion of the TEE probe (1-3). We present this case in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-24-241/rc).
Case presentation
A 78-year-old man (170 cm, 68 kg), who had been followed up for benign thyroid goiter and mitral valve (MV) regurgitation for years, complained of dyspnea and was admitted to hospital with a diagnosis of congestive heart failure (CHF). Transthoracic echocardiography (TTE) revealed severe mitral regurgitation (MR) due to prolapse of the mid-portion of the posterior leaflet (P2) of the MV. After cardiologists had performed medical treatment for CHF and catheter ablation for atrial flutter, they referred the patient to cardiac surgeons because mitral valvuloplasty (MVP) and left atrial appendage closure (LAAC) were indicated. The patient selected MICS for MVP rather than conventional open-heart surgery. Preoperative computed tomography (CT) revealed a 45-mm tumor in the left thyroid lobe that was compressing the esophagus (Figure 1). The patient also had symptoms of dysphagia. Therefore, prior to TEE, gastroenterologists performed trans-nasal esophagogastroduodenoscopy using an endoscope with a shaft diameter of 5.9 mm (EG-6500N, Fujifilm, Tokyo, Japan), which revealed no internal structural abnormalities in the esophagus. However, in a subsequent preoperative TEE examination, experienced cardiologists could not advance an adult TEE probe with a maximum tip diameter of 15 mm (X8-2t, Philips Medical Systems, Cambridge, MA, USA) beyond the pharynx because of strong resistance. Instead, they had to use a pediatric probe with a maximum tip diameter of 10 mm (S7-3t, Philips Medical Systems), although the two-dimensional (2D) image was of poor quality. Considering the severity of symptomatic MR, surgeons decided to perform a simultaneous operation, in which left thyroid lobectomy would be performed first to allow the passage of an adult TEE probe, followed by MICS-MVP and LAAC, rather than a two-stage operation in which the heart surgery would be performed much later than the thyroid surgery.

After establishment of an arterial line, anesthesiologists induced general anesthesia with midazolam and fentanyl, and administrated rocuronium to facilitate tracheal intubation with a 37-F left-sided double-lumen tube (Shiley/Mallinckrodt, Medtronic Inc., Minneapolis, MN, USA) using video laryngoscopy (McGrath MAC, Aircraft Medical Ltd., Edinburgh, UK). They easily intubated the patient with the tube. They maintained general anesthesia with sevoflurane or propofol, remifentanil, and rocuronium. First, otolaryngologists completely resected the left thyroid lobe including the goiter. They confirmed there was no visible bleeding from the surgical field. Next, experienced anesthesiologists tried to place the adult TEE probe. However, due to strong resistance, they could not advance the probe beyond the pharynx, even using various troubleshooting maneuvers, including jaw-thrust, neck flexion, lateral neck pressure, anterior displacement of the cricoid cartilage, and the use of video laryngoscopy (McGrath MAC, Aircraft Medical Ltd.) to clearly visualize the esophageal inlet. Finally, anesthesiologists had to place the pediatric TEE probe. They found no laryngeal edema in the patient after several attempts at probe insertion. Thereafter, anesthesiologists placed a central venous catheter and venous cannula for cardiopulmonary bypass (CPB) in the superior vena cava via the right internal jugular vein. Surgeons placed another venous cannula in the right atrium via the right femoral vein and an arterial cannula in the right subclavian artery. After establishing CPB, surgeons performed MICS-MVP and LAAC via a right mini-thoracotomy without any problem. Cardiologists used 2D images, color Doppler images, and continuous wave Doppler to assess the repaired MV. Although image quality was poor, there was no residual MR. Durations of aortic cross-clamping, CPB, and surgery (including thyroid lobectomy) were 97, 150, and 412 min, respectively.
After surgery, the patient was transferred to the intensive care unit and uneventfully extubated 4 hours later. Postoperative CT showed that the transverse diameter of the esophagus at the level of the thyroid gland increased from 2 mm preoperatively to 7 mm on postoperative day (POD) 4, but this was still smaller than that of the distal esophagus (16 mm). He was discharged in an ambulatory condition on POD 7. Although he complained of a mild sore throat, he did not have dysphagia upon discharge.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Extrinsic compression of the esophagus is one of the causes of difficult TEE probe insertion (1). The causes of its extrinsic compression include left atrium enlargement, aortic aneurysm, thoracic tumor, and thyroid tumor (2,3). In our case, the preoperative TEE examination was performed using a pediatric probe, because insertion of an adult TEE probe was unsuccessful due to esophageal compression by goiter. However, the images of the MV were of poor quality. Therefore, we scheduled a simultaneous operation, in which thyroid surgery would be performed first, followed by heart surgery, expecting that after removal of the tumor compressing the esophagus, we would be able to place an adult TEE probe for obtaining better intraoperative images of the MV. Contrary to our expectation, however, we could not advance the adult TEE probe beyond the pharynx due to strong resistance even after tumor resection. Consequently, we had to use a pediatric TEE probe again to assess the repaired MV.
In our case, a placement of the large adult TEE probe was unsuccessful not only before but also immediately after thyroid surgery, whereas placements of the small trans-nasal endoscope and pediatric TEE probe were successful even before thyroid surgery. Our experiences strongly suggested that dilatation of the esophagus, which had been chronically compressed by goiter, was not adequate enough to allow the passage of the large adult TEE probe immediately after thyroid surgery.
In patients with symptomatic benign goiter, Brinch et al. evaluated the size of the esophagus (measured with magnetic resonance imaging) and goiter-related swallowing difficulties prior to and 6 months after thyroid surgery (4). They reported that swallowing symptoms improved with increasing size of the esophagus in many patients at 6 months after surgery (4), whereas in some patients, swallowing symptoms and/or esophageal stenosis remained unchanged or even worsened at 6 months after surgery (4). They did not evaluate the size of the esophagus or swallowing symptoms immediately or shortly after surgery (4). However, in a systematic review analyzing the impact of goiter and thyroid surgery on esophageal dysfunction, Sorensen et al. concluded that goiter-related swallowing symptoms worsened in the early period after thyroid surgery, but improved after 6 months, as compared to baseline (5). Such reports seemed to support our assumption that dilatation of the chronically compressed esophagus could be inadequate at least immediately after thyroid surgery.
Intraoperative TEE is a class 1 indication for MVP and creating detailed three-dimensional (3D) images is sometimes required to evaluate the results of MVP (6-8). Meanwhile, when TEE probe insertion is difficult, it is important to consider alternative methods for acquiring images (1,9). In patients with narrowing of the oropharynx or esophagus, a pediatric probe is a useful alternative (1), although the use of a smaller probe is associated with reduced image quality (10). In our case, we had to use a pediatric 2D probe unable to create 3D images. However, recently developed pediatric mini 3D probes, such as GE 9VT-D (GE HealthCare, Chicago, IL, USA) and Philips X11-4t (Philips Medical Systems), would be helpful in obtaining more detailed images of the MV (11). As other alternatives, some case reports mention performing intraoperative esophageal dilation to facilitate TEE probe placement, but with a risk of esophageal injuries (12). In addition, an esophageal overtube and/or a gastroscope can be used as assistive devices for inserting adult TEE probes, although the cooperation of skilled gastroenterologists is required (13,14). Another alternative is TTE, although positive end-expiratory pressure interferes with its acoustic window in ventilated patients (15-17), and TTE is less informative than TEE to assess the MV adjacent to the esophagus (7,8). Unlike MICS, conventional sternotomy allows the surgeon to directly approach the heart, allowing the use of epicardial ultrasound (18). Intracardiac echocardiography (ICE) is a useful tool for observing the structure of the right-sided heart but is difficult to use for assessing the MV in the left-sided heart (19). Furthermore, venous cannulas for CPB would interfere with ICE. Based on the above-mentioned considerations, we propose a road map to cope with difficulties in inserting the TEE probe for MICS for MVP (Figure 2).
Our case report is limited to the presentation of a single patient, because of the rarity of the patient undergoing surgery requiring thyroid tumor resection and MVP.
Conclusions
We described here a patient with goiter undergoing MICS for MVP, in whom we could not place an adult TEE probe even after goiter resection. The cause of this difficulty seemed to be inadequate dilatation of the esophagus immediately after goiter resection probably because the esophagus had been chronically compressed by the goiter. However, we could evaluate the results of MICS-MVP using a pediatric TEE probe. When usual TEE probe placement is difficult, alternative methods for assessing the MV should be considered.
Acknowledgments
The authors appreciate the patient and the Juntendo Hospital operating room staff.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-24-241/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-24-241/prf
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-24-241/coif). I.K. serves as an unpaid editorial board member of AME Case Reports from May 2023 to April 2025. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hillenbrand KD, Racine CL, McNeil JS, et al. Difficult TEE Probe Placement: The Evidence, Troubleshooting Techniques, and a Guide to Alternative Monitoring Options for Intraoperative Physicians. Semin Cardiothorac Vasc Anesth 2019;23:369-78. [Crossref] [PubMed]
- Massey SR, Pitsis A, Mehta D, et al. Oesophageal perforation following perioperative transoesophageal echocardiography. Br J Anaesth 2000;84:643-6. [Crossref] [PubMed]
- Norton BC, Papaefthymiou A, Aslam N, et al. The endoscopic management of oesophageal strictures. Best Pract Res Clin Gastroenterol 2024;69:101899. [Crossref] [PubMed]
- Brinch FA, Døssing H, Nguyen N, et al. The Impact of Esophageal Compression on Goiter Symptoms before and after Thyroid Surgery. Eur Thyroid J 2019;8:16-23. [Crossref] [PubMed]
- Sorensen JR, Bonnema SJ, Godballe C, et al. The Impact of Goiter and Thyroid Surgery on Goiter Related Esophageal Dysfunction. A Systematic Review. Front Endocrinol (Lausanne) 2018;9:679. [Crossref] [PubMed]
- Ender J, Sgouropoulou S. Value of transesophageal echocardiography (TEE) guidance in minimally invasive mitral valve surgery. Ann Cardiothorac Surg 2013;2:796-802. [PubMed]
- Akhter N, Zhao Q, Andrei AC, et al. Identification of prolapsing mitral valve scallops by a three-dimensional multiplanar reconstruction method. Echocardiography 2015;32:106-13. [Crossref] [PubMed]
- Mantegazza V, Gripari P, Tamborini G, et al. 3D echocardiography in mitral valve prolapse. Front Cardiovasc Med 2022;9:1050476. [Crossref] [PubMed]
- Sharma V, Alderton S, McNamara H, et al. A safety checklist for transoesophageal echocardiography from the British Society of Echocardiography and the Association of Cardiothoracic Anaesthetists. Echo Res Pract 2015;2:G25-7. [Crossref] [PubMed]
- Reynolds HR, Spevack DM, Shah A, et al. Comparison of image quality between a narrow caliber transesophageal echocardiographic probe and the standard size probe during intraoperative evaluation. J Am Soc Echocardiogr 2004;17:1050-2. [Crossref] [PubMed]
- Karsenty C, Hadeed K, Pyra P, et al. Advancing paediatric cardiac imaging: a comprehensive analysis of the feasibility and accuracy of a novel 3D paediatric transoesophageal probe. Front Cardiovasc Med 2023;10:1294109. [Crossref] [PubMed]
- Spence BC, Hartman GS, Gosselin BJ. Intraoperative esophageal dilation for TEE probe placement in a patient with an undiagnosed esophageal stricture. J Cardiothorac Vasc Anesth 2005;19:209-11. [Crossref] [PubMed]
- Tan CO, Fernandes J, Leaver A, et al. Endoscopically assisted transesophageal echocardiographic probe insertion. J Cardiothorac Vasc Anesth 2011;25:e26-9. [Crossref] [PubMed]
- Reuss CS, Triester SL, Lynch JJ, et al. Esophageal overtube facilitation of transesophageal echocardiography in patients with previously difficult esophageal intubation. J Am Soc Echocardiogr 2007;20:285-9. [Crossref] [PubMed]
- Si X, Ma J, Cao DY, et al. Transesophageal echocardiography instead or in addition to transthoracic echocardiography in evaluating haemodynamic problems in intubated critically ill patients. Ann Transl Med 2020;8:785. [Crossref] [PubMed]
- Canty DJ, Heiberg J, Tan JA, et al. Assessment of Image Quality of Repeated Limited Transthoracic Echocardiography After Cardiac Surgery. J Cardiothorac Vasc Anesth 2017;31:965-72. [Crossref] [PubMed]
- Vignon P, Mentec H, Terré S, et al. Diagnostic accuracy and therapeutic impact of transthoracic and transesophageal echocardiography in mechanically ventilated patients in the ICU. Chest 1994;106:1829-34. [Crossref] [PubMed]
- Frenk VE, Shernan SK, Eltzschig HK. Epicardial echocardiography: diagnostic utility for evaluating aortic valve disease during coronary surgery. J Clin Anesth 2003;15:271-4. [Crossref] [PubMed]
- Basman C, Parmar YJ, Kronzon I. Intracardiac Echocardiography for Structural Heart and Electrophysiological Interventions. Curr Cardiol Rep 2017;19:102. [Crossref] [PubMed]
Cite this article as: Fukuda M, Kochiyama T, Aono K, Yonemoto S, Hayashi M, Hayashida M, Kawagoe I. Difficult insertion of a transesophageal echocardiography probe for cardiac surgery not only before but also immediately after thyroid goiter resection in a patient with chronic esophageal compression by the goiter: a case report. AME Case Rep 2025;9:63.


