
A rare case of mycosis fungoides with porokeratosis-like lesions: a case report and review of previous literature
Highlight box
Key findings
• This case illustrates a rare presentation of mycosis fungoides (MF) mimicking porokeratosis, with lesions isolated to the feet.
• The report adds to the sparse literature on porokeratosis-like MF, providing valuable clinical insights.
• Clinical and histopathological examination, along with immunohistochemical profiling, are critical in distinguishing MF from similar dermatological conditions.
What is known and what is new?
• Mycosis fungoides presents with diverse clinical manifestations and mimics other dermatoses.
• This case highlights a rare porokeratosis-like presentation of mycosis fungoides, expanding the spectrum of its variants.
What is the implication, and what should change now?
• Dermatologists should maintain a high index of suspicion for MF in cases presenting with atypical porokeratosis-like lesions.
• Increased awareness and documentation of such rare presentations can aid in the timely diagnosis and treatment of MF.
Introduction
Cutaneous T-cell lymphomas (CTCLs) are the second most prevalent group of extranodal lymphomas second to B-cell lymphomas (1). Among them, mycosis fungoides (MF) stands as the most frequently diagnosed cutaneous lymphoma and it represents a neoplasia of malignant monoclonal T lymphocytes that primarily invade the skin, leading to various cutaneous manifestations. These manifestations can range from erythematous scaly patches and plaques in the early stages to tumors or erythroderma in advanced stages, often with lymph nodes or visceral involvement (2,3). MF is also characterized by its diverse clinical manifestations, which may include hypopigmented, hyperpigmented, hyperkeratotic, pigmented-purpuric, verrucous, and pityriasis lichenoides-like lesions (4-9). Histologically, MF presents as an epidermotropic infiltrate of small to medium-sized CD4+ T lymphocytes with cerebriform nuclei. The classic immunophenotype of MF is CD3+/CD4+/CD45RO+ memory T cells (2,3). The diagnosis of CTCL is frequently postponed due to its ability to resemble both common and uncommon dermatological conditions (1). The occurrence of MF with features resembling porokeratosis is notably rare, with only four instances documented in the medical literature (10-12). This report introduces a rare case involving a 44-year-old male diagnosed with MF, who exhibited lesions akin to porokeratosis. We present this case in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-24-210/rc).
Case presentation
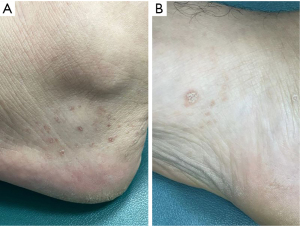
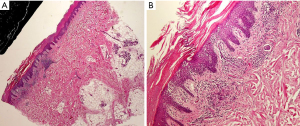
A 44-year-old male presented at the outpatient clinic with a seven-month history of lesions on both feet. Initially, the lesions appeared suddenly as a few skin-colored spots, which subsequently increased in number, darkened, and developed a peripheral scale, although they were not itchy. The patient reported no similar lesions elsewhere on the body and denied any oral symptoms. He had no chronic illnesses in his medical history and no family history of similar conditions, and has never been treated previously for a similar condition. Upon examination, multiple brownish papules with a collarette of scale, clinically resembling porokeratosis, were observed symmetrically distributed over the medial and lateral aspects of the dorsum of both feet, with additional similar lesions on the plantar aspects (Figure 1). A skin biopsy from the foot was obtained and revealed an acanthotic epidermis with a band-like infiltrate of lymphocytes in the papillary dermis and some papillary dermal fibrosis (Figure 2). Many lymphocytes within the epidermis exhibited a perinuclear halo; others showed mild nuclear enlargement and hyperchromasia (Figure 3). Immunohistochemical analysis showed diffuse positivity for CD3 and CD8 in both the epidermis and dermis. CD4 was mainly positive in dermal lymphocytes, while CD7 was predominantly absent in the epidermal lymphocytes (Figure 4). CD30 was negative. Although histology does not exhibit a cornoid lamella, the clinicopathologic correlation and immunohistochemistry confirmed the diagnosis of porokeratosis-like MF. The patient was prescribed daily applications of Clobetasol propionate 0.05% ointment and scheduled for follow-up (biweekly for 3 months). Two weeks after initiating the treatment plan, the patient reports adherence to topical therapy and improving skin lesions (partial improvement). The patient reports absence of recurrence during this period, with no associated adverse effects to therapy. No changes in treatment plan were done. Case timeline of events are provided in (Figure 5). All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.


Discussion
This case contributes to the rare but expanding body of knowledge on porokeratosis-like MF. MF is the most prevalent type of CTCL. It commonly affects older adults, exhibiting a male-to-female incidence ratio of approximately (1.6–2.0:1), although it can also occur in children and adolescents. Clinically, MF presents as an indolent eruption of erythematous scaly patches or plaques, which can resemble common dermatological conditions such as atopic dermatitis or psoriasis. Initially, lesions typically manifest in sun-protected areas, but they can eventually involve any skin site (13). A myriad of clinical variants of MF have been documented. Histopathologically, MF is characterized by variable features, commonly including a superficial band-like lymphocytic infiltrate and atypical lymphocytes exhibiting epidermotropism (14). These epidermal lymphocytes often appear larger and more atypical than those in the dermis and are frequently surrounded by a halo that delineates the lymphocyte nuclei from adjacent keratinocytes (15). In the dermis, papillary dermal fibrosis is typically observed (16). The findings in our case we presented align with these characteristics of MF. The immunophenotype of MF generally features epidermotropic peripheral T lymphocytes, typically expressing CD2+, CD3+, CD4+, CD5+, CD8−, CD45RO+, CD20−, and CD30−. Occurrences of CD4− or CD8+, double positive or double negative cases are infrequent (17,18). A loss of CD7 expression is often noted even in the early stages of the disease (18). The biopsy from our patient corresponded with this expected immunophenotype of MF, exhibiting CD7 loss and double positivity for CD4 and CD8.
MF presenting with porokeratosis-like lesions have been seldom reported. The first two cases were described by Hsu et al. in 1992, involving two black patients with widespread, sharply demarcated, round hyperpigmented or hypopigmented macules that clinically resembled disseminated superficial actinic porokeratosis (10). In 1993, Breneman et al. reported a case of MF that mimicked porokeratosis of Mibelli (11). The most recent case was documented by Tawfiq et al. in 2014, involving a young male with generalized hyperpigmented macules similar to porokeratosis of Mibelli (12). Previous cases of porokeratosis-like MF, such as those reported by Hsu et al. and Breneman et al., had different lesion distributions and were not limited to the feet. This case differs by its localized foot involvement. The patient’s lesions, confined to the feet, represent an uncommon distribution for such MF variants.
Our patient presented with localized lesions on both feet, appearing as multiple scattered brownish papules, some with a collarette of scale, and including plantar involvement. The clinical differential diagnosis considered porokeratosis, secondary syphilis, and MF. Given the unusual presentation, a clinicopathologic correlation was essential to establish the diagnosis. The importance of recognizing such rare clinical variants lies in the implications for management and prognosis. The ability to differentiate MF from other dermatoses that it may mimic, such as porokeratosis, is critical in avoiding misdiagnosis and ensuring appropriate treatment. Moreover, this case contributes to the broader dermatological knowledge by documenting an additional instance of MF mimicking porokeratosis, expanding the spectrum of known clinical presentations of this lymphoma. It emphasizes the need for heightened suspicion and comprehensive diagnostic strategies, particularly in cases where the clinical presentation deviates from the more typical manifestations of MF. By continuing to document and study such rare presentations, clinicians can enhance their understanding and improve outcomes for patients with this complex and variable disease. This case expands the limited spectrum of porokeratosis-like MF presentations. Limitations include the lack of long-term follow-up data on treatment efficacy, the absence of T-cell receptor rearrangement analysis (which is increasingly used in MF diagnosis), as well as lack of dermoscopic findings, which could have provided additional diagnostic clarity. We recommend including dermoscopy in future cases of porokeratosis-like MF to enhance diagnostic precision. Moreover, this unique variant may require tailored therapeutic strategies, emphasizing the need for further research into its specific management needs.
Conclusions
Porokeratosis-like MF is a rare and uncommon instance. The distinctive morphology and distribution of such lesions poses significant diagnostic challenges. It is imperative to include MF in the differential diagnosis when encountering atypical presentations of porokeratosis. A thorough clinicopathologic correlation is crucial for accurate diagnosis.
Acknowledgments
None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-24-210/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-24-210/prf
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-24-210/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kim EJ, Hess S, Richardson SK, et al. Immunopathogenesis and therapy of cutaneous T cell lymphoma. J Clin Invest 2005;115:798-812. [Crossref] [PubMed]
- Kazakov DV, Burg G, Kempf W. Clinicopathological spectrum of mycosis fungoides. J Eur Acad Dermatol Venereol 2004;18:397-415. [Crossref] [PubMed]
- Hodak E, Amitay-Laish I. Mycosis fungoides: A great imitator. Clin Dermatol 2019;37:255-67. [Crossref] [PubMed]
- Stone ML, Styles AR, Cockerell CJ, et al. Hypopigmented mycosis fungoides: a report of 7 cases and review of the literature. Cutis 2001;67:133-8. [PubMed]
- Kikuchi A, Shimizu H, Nishikawa T. Mycosis fungoides with marked hyperpigmentation. Dermatology 1996;192:360-3. [Crossref] [PubMed]
- Hannah M, Jacyk WK. Palmoplantar hyperkeratotic plaques. Hyperkeratotic mycosis fungoides restricted to the palms and soles. Arch Dermatol 1998;134:1021, 1024.
- Georgala S, Katoulis AC, Symeonidou S, et al. Persistent pigmented purpuric eruption associated with mycosis fungoides: a case report and review of the literature. J Eur Acad Dermatol Venereol 2001;15:62-4. [Crossref] [PubMed]
- Wakelin SH, Stewart EJ, Emmerson RW. Poikilodermatous and verrucous mycosis fungoides. Clin Exp Dermatol 1996;21:205-8. [Crossref] [PubMed]
- Ko JW, Seong JY, Suh KS, et al. Pityriasis lichenoides-like mycosis fungoides in children. Br J Dermatol 2000;142:347-52. [Crossref] [PubMed]
- Hsu WT, Toporcer MB, Kantor GR, et al. Cutaneous T-cell lymphoma with porokeratosis-like lesions. J Am Acad Dermatol 1992;27:327-30. [Crossref] [PubMed]
- Breneman DL, Breneman JC. Cutaneous T-cell lymphoma mimicking porokeratosis of Mibelli. J Am Acad Dermatol 1993;29:1046-8. [Crossref] [PubMed]
- Tawfiq S, Aziz Z, Sultan A, et al. Cutaneous T-cell lymphoma with porokeratosis-like lesions: A case report and review of literature. Egyptian Dermatology Online Journal 2014;10:1-5. [Crossref]
- Zinzani PL, Ferreri AJ, Cerroni L. Mycosis fungoides. Crit Rev Oncol Hematol 2008;65:172-82. [Crossref] [PubMed]
- Smoller BR, Santucci M, Wood GS, et al. Histopathology and genetics of cutaneous T-cell lymphoma. Hematol Oncol Clin North Am 2003;17:1277-311. [Crossref] [PubMed]
- Smith NP. Histologic criteria for early diagnosis of cutaneous T-cell lymphoma. Dermatol Clin 1994;12:315-22. [Crossref] [PubMed]
- Shapiro PE, Pinto FJ. The histologic spectrum of MF/Sezary syndrome (cutaneous T-cell lymphoma). Am J Surg Pathol 1994;18:645-67. [Crossref] [PubMed]
- Pimpinelli N, Olsen EA, Santucci M, et al. Defining early mycosis fungoides. J Am Acad Dermatol 2005;53:1053-63. [Crossref] [PubMed]
- Robson A. Immunocytochemistry and the diagnosis of cutaneous lymphoma. Histopathology 2010;56:71-90. [Crossref] [PubMed]
Cite this article as: Alkeraye SS, Alsehli TN, Alhumidi A, Al-Husain K, Nagshabandi KN. A rare case of mycosis fungoides with porokeratosis-like lesions: a case report and review of previous literature. AME Case Rep 2025;9:67.



