Redo transanal total mesorectal excision (Re-TaTME) after initial TaTME; is it possible?
Background
Colorectal cancer is the 3rd commonest cancer in the world as well as the 4th commonest cause of cancer death, one third of these cancers is located in the rectum (1).
Laparoscopy has been increasingly in use in the treatment of colorectal cancer (2). More recently transanal total mesorectal excision (TaTME) evolved to solve the problem of dissecting in narrow pelvis especially in male and obese patients (3).
However, anastomotic complications are still among the most feared and difficult problems facing colorectal surgeons in their practice, as the results of a failed anastomosis can be devastating to both the patient and the surgeon. Prolonged hospitalization, permanent stoma affecting life quality and multiple operations are the most critical outcomes. Complications can be divided into early (as bleeding and leak) and delayed as strictures; fortunately most of them could be managed with non-operative approaches (4).
The optimal surgical treatment of persistent stricture is unsettled. Many approaches do exist; usually stepwise management is applied with the open abdominal approach as the gold standard (5).
Herein, to our knowledge, we report the first case of combined transanal and transabdominal resection with re-anastomosis of an anastomotic stricture after a previous TaTME operation for rectal cancer.
Case presentation
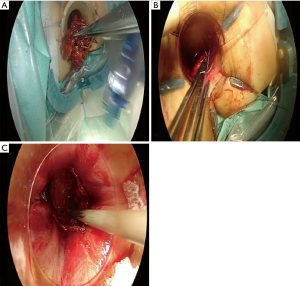
A male patient aged 70 years old with BMI 23.7 presented to the outpatient surgical clinic for closure of ileostomy. On dorsal rectal examination anastomotic stricture was felt at about 8 cm from anal verge for which flexible colonoscopy was done revealing impassable stricture with no detected malignancy in biopsy (Figure 1). The patient had a history of TaTME (without previous therapy) at August 2016 for radiological (by MRI and CT scan) node negative rectal cancer about 10 cm from the anal verge in CHUAC hospital, with the postoperative pathology grade II adenocarcinoma pT3N1bM0, with covering loop ileostomy by two teams. In the same admission a collection was detected presacrally by computed tomography done a week after the operation, probably suggesting a minor leak, which was treated by radiologic guided drainage and antibiotics. After which a course of adjuvant concurrent chemoradiotherapy was given. Follow up CT thorax, abdomen and pelvis after 6 months and one year was irrelevant. Three trials of endoscopic dilatation of the stenosis failed, as the guide wire could not pass the stricture, instead a faulty passage in a nearby recess occurred. The multidisciplinary decision was to resect the stenosed segment, a combined hybrid natural orifice transluminal endoscopic surgery (NOTES) technique was suggested, as it is easier to identify the segment transanally, in addition the laparoscopy is needed for adhesiolysis. The two teams work through multiport laparoscopy (5 ports) and transanal minimally invasive surgery (TAMIS) using GELPOINT path transanal access platform (Applied Medical, CA, USA). Operation started by adhesiolysis and closure of sigmoid lumen by tape, then the transanal step was initiated concomitantly by applying lone star retractor, taking a purse string suture one cm below the stenosed part (Figure 2) then dissection through the TME plane till the two teams meet (Figure 3). The specimen was extracted transanally after cutting the proximal colon (Figure 4A), then through a mini-Pfannenstiel incision (as the colon was deemed short for exteriorization) the anvil of the stapler was inserted into the colon and secured with a purse string. Another purse string suture was fixed transanally all around the rectal stump (Figure 4B) then tightened around the long anvil rod. Anastomosis was done by a hemorroidal EEA stapler 31 and checked transanally (Figure 4C). The postoperative course was smooth and the patient is planned for closure of ileostomy 6 weeks later.

Discussion
Since 2009 the indications of TAMIS have been expanded and the spectrum of pathology which can be treated with it has increased from simple excision of small rectal lesions/Tis-1 rectal cancer to total mesorectal excision (TaTME) (6), and recently for trans-stomal excision of tumours (7).
In a Cochrane review study, anastomotic strictures were observed in 5% of patients after stapled colorectal anastomosis (8). Anastomotic strictures have been conventionally treated by Hegar dilatation or endoscopic hydrostatic balloon dilatation, followed by transabdominal excision of the stenotic segment in case of persistent narrowing (5).
Many technical problems arose during redo pelvic surgery; one of them is the difficulty to achieve an adequate exposure. In addition, redo anastomotic surgery for patients with a pelvic abscess or leak after low/ultralow anterior resection or pouch dysfunction is usually hindered by adhesions, fibrosis and distorted anatomical planes. This may be an indication for bottom to up minimally invasive approach (9).
Some authors reported transanal endoscopic surgery (TES) for management of anastomotic stricture without abdominal assistance. In this method the stenotic anastomosis or scar is incised until restoration of the rectal lumen (>2 cm diameter), it is actually a strictureplasty. If the stenosis is larger, partial or complete resection of the stricture can be performed. The rectal wall defect is closed transversely when possible (5).
Borstlap in 2016 described the first series of patients of redo low rectal anastomosis and ileoanal pouches using combined laparoscopy and TAMIS, in fact a technique similar to TaTME but without the proximal vascular control which has been already done in the first surgery plus there is no need for node dissection in a non-oncologic surgery. In his series the two teams meet each other (successful rendezvous) in all patients (apart of two cases in whom they considered no need for abdominal approach) (9).
The long-term results of the combined transanal-transabdominal resection and redo of anastomosis for the management of colorectal surgery complications is still unclear. Moreover, doing a TaTME for managing complications after an original TaTME for cancer is an innovative approach.
Conclusions
Combined laparoscopic and transanal endoscopic approach (Re-TaTME) for managing of anastomotic stricture after TaTME is a feasible and reproducible technique.
Acknowledgements
None.
Footnote
Conflicts of Interest: JF Noguera reports personal fees from Medtronic, other from Johnson & Johnson, outside the submitted work. The other authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- GLOBOCAN 2012: Estimated cancer incidence, mortality and prevalence worldwide in 2012. Lyon, France: International Agency for Research on Cancer, 2012.
- Bonjer HJ, Deijen CL, Abis GA, et al. A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 2015;372:1324-32. [Crossref] [PubMed]
- Sylla P, Rattner DW, Delgado S, et al. NOTES transanal rectal cancer resection using transanal endoscopic microsurgery and laparoscopic assistance. Surg Endosc 2010;24:1205-10. [Crossref] [PubMed]
- Umanskiy K, Hyman N. Anastomotic Complications. In: Steele SR, Hull TL, Read TE, et al. editors. The ASCRS Textbook of Colon and Rectal Surgery. Springer, 2016:161-71.
- van Vledder MG, Doornebosch PG, de Graaf EJ. Transanal endoscopic surgery for complications of prior rectal surgery. Surg Endosc 2016;30:5356-63. [Crossref] [PubMed]
- Plummer JM, Leake PA, Albert MR. Recent advances in the management of rectal cancer: No surgery, minimal surgery or minimally invasive surgery. World J Gastrointest Surg 2017;9:139-48. [Crossref] [PubMed]
- Atallah S. Utilization of the TAMIS technique for trans-stomal excision of a colonic neoplasm: a video demonstration. Tech Coloproctol 2016;20:779-80. [Crossref] [PubMed]
- Neutzling CB, Lustosa SA, Proenca IM, et al. Stapled versus handsewn methods for colorectal anastomosis surgery. Cochrane Database Syst Rev 2012.CD003144. [PubMed]
- Borstlap WA, Harran N, Tanis PJ, et al. Feasibility of the TAMIS technique for redo pelvic surgery. Surg Endosc 2016;30:5364-71. [Crossref] [PubMed]
Cite this article as: Metwally IH, Romero JA, Coello PC, Noguera JF. Redo transanal total mesorectal excision (Re-TaTME) after initial TaTME; is it possible? AME Case Rep 2018;2:6.




