Metastasis to the thyroid gland from a tonsil squamous cell carcinoma
Introduction
Tonsil squamous cell carcinoma is the most common type of tonsillar cancer and at the same time it represents 70% of all malignant oropharyngeal cancers. Tonsillar squamous cell carcinoma often metastasizes to cervical lymph nodes and it can invade the surrounding deep tissues. Metastasis to the thyroid gland from a squamous cell carcinoma is extremely rare (1).
Thyroid gland is amongst the least frequent sites for metastasis and only 1% of thyroid cancers are metastatic in origin (2). The common primary tumors that metastasize to the thyroid gland are renal cell and colorectal carcinoma, while sarcoma is amongst the least common primary origins for thyroid metastasis. The time interval between the original diagnosis of the primary cancer and the metastasis to the thyroid gland is variable and ranges between few months to years (3).
Case presentation
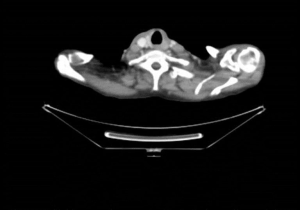
A 69-year-old male patient with a past medical history of tonsil squamous cell carcinoma, stage T3N0, for which he had complex surgery in 2015. He underwent trans-oral robotic bilateral neck dissection, followed by re-exploration and radial forearm free flap (RFFF). He had partial loss of the RFFF pharyngeopalatal reconstruction, so he needed to undergo right hemi palate reconstruction with buccinators flap. Eighteen months following his operation, he had left retropharyngeal recurrence which was treated with radiotherapy. His thyroid function tests were normal. As part of the screening process for his tonsil squamous cell carcinoma he underwent whole body PET scan in date which showed an enlarging markedly FDG avid nodule posteriorly within the left lobe of thyroid which was not present in December 2016 (Figure 1). The patient was referred to the Endocrine Surgical clinic for further investigation of the thyroid nodule. He reported dysphagia and voice hoarseness while denied any neck pain and hypo- or hyperthyroid symptoms. On examination, he had a palpable left sided thyroid nodule.
An US of the neck showed a hypoechoic nodule in the left lobe of the thyroid measuring 14 mm × 15 mm which demonstrated peripheral and internal vascularity. No other discrete thyroid nodules or enlarged or morphologically suspicious lymph nodes were visualized in the neck. A free-hand FNAC of the thyroid nodule was reported as highly suspicious for squamous cell carcinoma.
Discussion
Despite the rich blood supply of the thyroid gland, it has a low incidence of metastasis. Metastasis to the thyroid gland was described as early as 1871 from a primary testicular tumor. The low incidence of metastasis may be attributed to the fast arterial blood flow, as well as, the high levels of oxygen and iodine. These factors may prevent dislodging of the secondary tumor cells and their secondary growth (1).
Patients with metastatic thyroid cancer usually present with symptoms similar to primary thyroid cancer, mainly a palpable neck mass. Dysphagia or dysphonia may develop later if the metastatic cancer is advanced. Thyroid function is usually normal (4,5). That’s why detailed and thorough past medical and surgical history is very important, and metastatic thyroid cancer should be considered in any patient presenting with thyroid nodule especially if the patient has history of previous malignancy, regardless the time elapsed between the diagnosis of the primary malignancy. In addition, the recurrence of the primary disease should be considered. Detailed clinical history may also reveal occult primary malignancy, for example if the patient is complaining of hematuria or hemoptysis; this may indicate underlying renal or lung cancer.
Diagnostic approach is the same as any thyroid nodule (history and examination, imaging, biopsy). The advancement in technology has helped significantly in diagnosis via using high resolution ultrasound, CT and PET scan; however, these scans are sometimes unreliable in differentiating between primary and secondary lesions. FNAC can usually be of great assistance (6).
Treatment options depend on the general condition of the patient and the extent of the tumor. If there are no signs of extra glandular extension, total or hemi-thyroidectomy is a good option (7), and that was the management plan for our patient. Each patient needs to be discussed in the MDT meeting before the final decision. If there is no sign of recurrence at the primary site, thyroidectomy should be considered.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Lee DJ, Kwon MJ, Nam ES, et al. Histopathologic predictors of lymph node metastasis and prognosis in tonsillar squamous cell carcinoma. Korean J Pathol 2013;47:203-10. [Crossref] [PubMed]
- Willis RA. Metastatic Tumours in the Thyreoid Gland. Am J Pathol 1931;7:187-208.3.
- Chung AY, Tran TB, Brumund KT, et al. Metastases to the thyroid: a review of the literature from the last decade. Thyroid 2012;22:258-68. [Crossref] [PubMed]
- Papi G, Fadda G, Corsello SM, et al. Metastases to the thyroid gland: prevalence, clinicopathological aspects and prognosis: a 10-year experience. Clin Endocrinol (Oxf) 2007;66:565-71. [PubMed]
- Shimaoka K. Thyrotoxicosis due to metastatic involvement of the thyroid. Arch Intern Med 1980;140:284-5. [Crossref] [PubMed]
- Cozzolino I, Malapelle U, Carlomagno C, et al. Metastasis of colon cancer to the thyroid gland: a case diagnosed on fine-needle aspirate by a combined cytological, immunocytochemical, and molecular approach. Diagn Cytopathol 2010;38:932-5. [Crossref] [PubMed]
- Czech JM, Lichtor TR, Carney JA, et al. Neoplasms metastatic to the thyroid gland. Surg Gynecol Obstet 1982;155:503-5. [PubMed]
Cite this article as: Gumaa D, Christakis I, Mihai R. Metastasis to the thyroid gland from a tonsil squamous cell carcinoma. AME Case Rep 2018;2:7.