Primary Hodgkin’s lymphoma of liver in HIV—a case report and review of literature
Introduction
Primary hepatic lymphoma is a very rare entity accounting for less than 0.4% of all extranodal lymphomas (1) and usually occurs in immunocompromised states. Non-Hodgkin’s lymphoma especially the B-cell varieties are more common than Hodgkin’s lymphoma. The clinical presentation is variable and radiological features are non-specific sometimes mimicking other liver tumours like hepatocellular carcinoma, metastases or cholangiocarcinoma. We report a case of Hodgkin’s lymphoma presenting as primary hepatic lymphoma with radiological features mimicking a fibrolamellar HCC.
Case presentation
A 55-year-old HIV positive male was admitted with complaints of vague dull aching pain in the right hypochondrium for 4 weeks with loss of appetite. However, he had no bowel symptoms or jaundice or fever or chills or night sweats. He was HIV positive for 11 years and on antiretroviral therapy. On examination, he did not have any generalized lymphadenopathy, pallor or icterus. Abdominal examination revealed mild hepatomegaly.
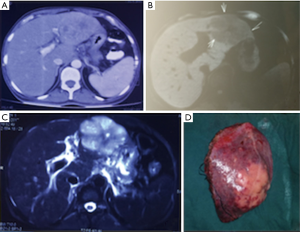
Blood investigations revealed normal liver and renal function tests, a total leukocyte count of 3.7×103/L and CD4 count of 329 cells/L. Both OGD and colonoscopies were normal. Serum AFP was 2.3 U/mL. A CECT abdomen showed a 6.9 cm × 6.2 cm well-defined heterodense mass lesion in left lobe of liver showing early arterial enhancement and rapid washout in venous phase suggestive of HCC (Figure 1A). MRI abdomen showed a T1 hypointense and T2 hyperintense lesion with a central scar in the lesion suggestive of fibrolamellar HCC (Figure 1B,C). The patient underwent a left lateral sectionectomy by a rooftop incision (Figure 1D). Postoperatively, he had an uneventful recovery.
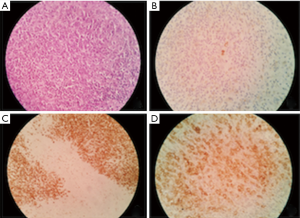
The histopathology of the specimen revealed large round to polyhedral neoplastic cells arranged in sheets having scant to moderate eosinophilic cytoplasm with large nuclei some showing prominent eosinophilic nucleoli and binucleate forms. Immunohistochemistry revealed focal positivity for CD15 and CD30 positivity in binucleate and mononuclear cells and negative for CK7 and CK20 suggestive of Hodgkin’s lymphoma (Figure 2). Bone marrow biopsy was negative for any lymphomatous infiltration. The patient was started on chemotherapy—Adriamycin, bleomycin, vinblastine and dacarbazine (ABVD regimen) along with HAART.
Literature review
Primary hepatic lymphoma (PHL) is a lymphoma limited to the liver or having major liver involvement at presentation without evidence of extrahepatic involvement within 6 months (1). PHL most commonly affects men during their fifth decade of life.
Although gastrointestinal tract is the most common site of primary extra nodal lymphoma, liver as a primary site of involvement is uncommon and accounts for less than 0.4% of extranodal NHLs and 0.016% of all NHLs (1). This is because host factors make the liver a poor environment for the development of malignant lymphoma in spite of the presence of lymphoid tissue in liver. But impaired immunity associated with HIV infection, immunosuppressive therapy post-transplant, liver cirrhosis, systemic lupus erythematosis and viral infections such as HBV, HCV, Epstein-Barr virus and human T-lymphotropic virus might play an important role in development of PHL (2).
Morphologically PHL can be uninodular, multinodular or diffuse types based on the pattern of liver infiltration. Histologically, non-Hodgkin’s lymphoma is more likely than Hodgkin’s lymphoma to have hepatic involvement and they are most commonly of B-cell variety especially diffuse large B cell type. Other less common varieties include Burkitt’s lymphoma, follicular lymphoma, T cell lymphoma and NHL-NOS (3).
PHL presents most commonly with B symptoms like fever, loss of weight, night sweats and less commonly with jaundice and hepatomegaly and sometimes very rarely as acute liver failure especially in the diffuse variety. 10% are detected incidentally. The important differential diagnoses include hepatocellular carcinoma and metastatic tumours for nodular variety and intrahepatic cholangiocarcinoma for the diffuse variety (4).
PHLs are generally hypovascular lesions with minimal enhancement on all phases in a contrast enhanced CT and may have hypoattenuating centre suggestive of necrosis and haemorrhage. But there are reports of lesions showing arterial enhancement and delayed venous washout typical of HCC causing diagnostic dilemma like in our case (5). According to one study, MRI features of variable low T1 and high T2 signal intensities with minimal or no enhancement on dynamic post-gadolinium imaging were indicative of PHL. Tumour encasement of vessels was a distinctive finding. However, no MRI feature is specific for diagnosis of PHL (6).
Due to the rarity of the disease, variability in clinical presentation and nonspecific radiological features, a high index of suspicion and early liver biopsy along with ancillary tests remains the only way to make the diagnosis. The presence of elevated LDH in the presence of normal AFP can point towards the diagnosis of PHL when suspected. Still, many a times, the diagnosis is missed and is established only after histopathological examination of the resected specimen. Hence, even when radiological findings show a typical appearance of HCC, consideration of the other differential diagnoses is required, particularly when serum AFP is normal and a patient has no risk factors for HCC, and needle biopsy may be performed before surgical resection (5).
Once diagnosis is established, most patients are treated with chemotherapy regimen according to the type of lymphoma along with HAART in HIV positive patients. A large review of the literature has shown that in patients with localized disease treated with surgery followed by chemotherapy have better survival rates (7). Postoperative chemotherapy is found to be the only prognostic factor for survival and should be considered to prevent disease recurrence (8).
Conclusions
Hodgkin lymphoma very rarely presents as Primary hepatic lymphoma especially in the background of an immunocompromised state. The clinical presentation is variable and radiological features are not specific and can mimic hepatocellular carcinoma especially the fibrolamellar variant. However, it should be suspected in immunocompromised patients like HIV in the presence of normal AFP levels and enlarged regional lymph nodes. In such patients, even in the presence of typical radiological findings of HCC, a liver biopsy may be done to clinch the diagnosis and thereby avoid a major surgical resection. In fit patients, surgical resection followed by chemotherapy is also an equally effective alternative.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- El-Fattah MA. Non-Hodgkin Lymphoma of the Liver: A US population-based analysis. J Clin Transl Hepatol 2017;5:83-91. [PubMed]
- Park JI, Jung BH. Primary hepatic lymphoma treated with liver resection followed by chemotherapy: a case report. Ann Hepatobiliary Pancreat Surg 2017;21:163-7. [Crossref] [PubMed]
- Bai YF, Liu JM, Zhang XM, et al. Percutaneous liver biopsy: retrospective study of primary and secondary hepatic lymphoma in twenty-one patients. Hepatobiliary Pancreat Dis Int 2017;16:58-64. [Crossref] [PubMed]
- Forghani F, Masoodi M, Kadivar M. Primary hepatic lymphoma mimicking cholangiocarcinoma. Oman Med J 2017;32:335-8. [Crossref] [PubMed]
- Lee J, Park KS, Kang MH, et al. Primary hepatic peripheral T-cell lymphoma mimicking hepatocellular carcinoma: a case report. Ann Surg Treat Res 2017;93:110-4. [Crossref] [PubMed]
- Semelka RC, Nimojan N, Chandana S, et al. MRI features of primary rare malignancies of the liver: A report from four university centres. Eur Radiol 2018;28:1529-39. [Crossref] [PubMed]
- Ugurluer G, Miller RC, Li Y, et al. Primary hepatic lymphoma: a retrospective, multicenter rare cancer network study. Rare Tumors 2016;8:6502. [Crossref] [PubMed]
- Yang XW, Tan WF, Yu WL, et al. Diagnosis and surgical treatment of primary hepatic lymphoma. World J Gastroenterol 2010;16:6016-9. [PubMed]
Cite this article as: Muthukrishnan S, Amudhan A, Rajendran S. Primary Hodgkin’s lymphoma of liver in HIV—a case report and review of literature. AME Case Rep 2018;2:21.


