A unique surgical emergency: ileosigmoid knotting
Introduction
Ileosigmoid knot (ISK) is a rare but potentially lethal condition with a mean mortality rate of 35.5%. Mortality may be related to duration of symptoms, presence of gangrenous bowel, and septic shock (1). Unfamiliarity with the disease and atypical radiographic findings make preoperative diagnosis rare. However, prompt diagnosis and early surgical intervention significantly improve outcomes.
Surgical repair is aimed at reducing the knot if possible, and resecting any ischemic/gangrenous bowel. If the small bowl is viable, resection is not indicated; however, if the sigmoid colon is viable, resection should still be performed due to increased risk of recurrence. When either small bowel or sigmoid colon resections are performed, literature supports primary anastomosis as a safe repair (1).
Case presentation
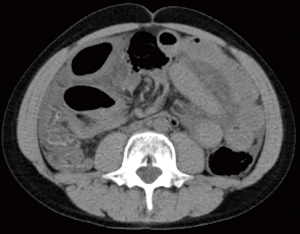
A 14-year-old male with a past medical history of constipation was brought to the emergency department complaining of sharp, post defecation abdominal pain for two hours. On physical exam, he was mildly distended, and exhibited diffuse tenderness. Laboratory abnormalities included a white blood cell count of 25.7 K/µL, and a lactic acid of 3.5 mmol/L. Initial imaging included an abdominal radiograph which demonstrated dilated loops of bowel (Figure 1), and a CT scan which confirmed dilated bowel around what the radiologist described as either a midgut volvulus or internal hernia (Figure 2).
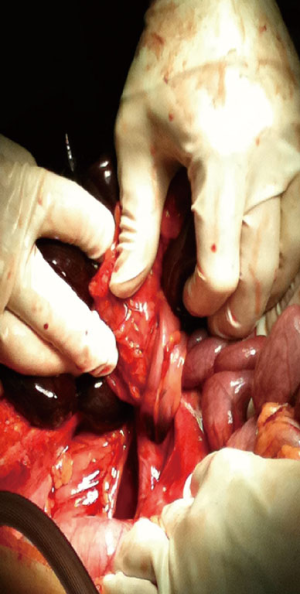
With these findings, the patient was taken to the operating theatre. Therein, a 360° volvulus was encountered (Figure 3), with several loops of necrotic small bowel wrapped around a necrosed sigmoid colon. The volvulus was detorsed, the necrotic bowel was resected (Figure 4), and two separate primary anastomoses were performed.
Discussion
ISK is a rare but potentially lethal condition in which a portion of ileum and sigmoid colon wrap around each other, forming a closed loop obstruction. ISK most commonly affects adult males in their 40s, in Asia, Africa and the Middle East (1-3). Our case of ISK in a pediatric patient makes for a rare diagnosis.
ISK has been classified into four subtypes, however, the exact mechanism for developing the knot remains unclear. Type I (53.9–57.5%) is the most common, where the ileum (active component) wraps itself around the sigmoid colon (passive component). Type II (18.9–20.6%) is the opposite, where the sigmoid colon acts as the active component. Type III (1.5%) is where the ileocecal segment acts as the active component. And type IV is an undetermined type (1,2,4). It has been postulated that anatomic and physiologic features serve as predisposing factors. These include a hypermobile small intestine with an elongated mesentery, a redundant sigmoid colon with a long mesocolon and a short attachment, and ingestion of a high bulk diet with an empty small bowel (1-4).
Predominant symptoms include abdominal pain/tenderness (100%), distension (94–100%), nausea and vomiting (87–100%), and rebound tenderness (69%) (1,5). Plain abdominal radiography may show a double closed-loop obstruction (1). CT scan may demonstrate the classic whirl sign, medial deviation of the distal descending colon with a pointed appearance in its medial border, or radial distribution of the intestine/mesenteric vasculature (1,2). The whirl seen with an ISK is visible on more contiguous slices that that seen with sigmoid volvulus, which it is often confused with. It is important to differentiate between the two because ISK is a surgical emergency in which endoscopic reduction is contraindicated (1-3).
Preoperative diagnosis of ISK is uncommon, and it is often confused as sigmoid volvulus or small bowel obstruction (1-3). When ISK develops, rapid progression to gangrenous bowel can occur, making prompt diagnosis and early intervention imperative (1-3,5).
Initial management includes aggressive resuscitation, hemodynamic stabilization, and early surgical exploration. At surgery, prolonged attempts at untwisting the knot are not recommended (1). When the bowel is gangrenous, it may be difficult to untie the knot, increasing potential for spillage of toxic bowel contents. In these instances, the bowel should be clamped before dissection or resection (2).
When the remaining bowel is healthy, well vascularized, and nondistended, primary anastomosis is preferred for both the small bowel and sigmoid colon. However, if the terminal ileum is gangrenous within 10cm of the ileocecal valve, diversion is preferred (1,2).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Machado NO. Ileosigmoid knot: a case report and literature review of 280 cases. Ann Saudi Med 2009;29:402-6. [Crossref] [PubMed]
- Baheti AD, Patel D, Hira P, et al. Ileosigmoid knot: A case report. Indian J Radiol Imaging 2011;21:147-9. [Crossref] [PubMed]
- Lee SH, Park YH, Won YS. The ileosigmoid knot: CT findings. AJR Am J Roentgenol 2000;174:685-7. [Crossref] [PubMed]
- Mallick IH, Winslet MC. Ileosigmoid knotting. Colorectal Dis 2004;6:220-5. [Crossref] [PubMed]
- Selçuk Atamanalp S. Treatment for ileosigmoid knotting: a single-center experience of 74 patients. Tech Coloproctol 2014;18:233-7. [Crossref] [PubMed]
Cite this article as: Bain K, Lelchuk A, Nicoara M, Meytes V. A unique surgical emergency: ileosigmoid knotting. AME Case Rep 2018;2:29.