Huge brachial plexus schwannoma, masking as a cystic neck mass
Introduction
Schwannomas are benign encapsulated tumors, originating from the Schwann cells of cranial, peripheral or autonomic nerve sheaths. Verocay first described schwannoma as a pathological entity in 1908, and coined the term neurinoma in 1910 followed by Stout whom used the term neurilemmoma in 1935 (1). It is reported that 25–45% of schwannomas present in the head and neck region, however primary tumors of the brachial plexus are rare (2). A more common differential for a painless lateral cystic neck mass is lymphangiomatous malformations which histological subtypes include cavernous lymphangioma, capillary lymphangioma and cystic hygroma. It is rare to find a branchial plexus schwannoma, and also uncommon for it to present as a cystic neck mass. Reported is a case of a 56-year-old man with a lateral supraclavicular cystic mass arising from the brachial plexus, histologically proven to be a schwannoma.
Case presentation
A 56-year-old Chinese gentleman presented with a painless cystic right neck swelling, progressively increasing in size over a 4-year period. He had no upper limb weakness nor pain, but complained of tingling sensation over the radial aspect of his right forearm, numbness over the tip of right thumb and index finger as the lesion progressively expanded. He was dominant right-handed worker which interfered with his employment as a designer in the advertisement department.
The mass extended from the lower one third of the right sternocleidomastoid muscle and laterally into the right supraclavicular fossa. It measured 8 cm × 8 cm, was soft, fluctuant, non-pulsatile and mobile. The overlying skin was smooth, not attached and not erythematous. There was no tenderness on palpation, no bruit on auscultation. There were no palpable neck nodes and no significant findings in the flexible scope of the nasopharynx and larynx.
A magnetic resonance imaging scan showed a multiseptated enhancing cystic lesion at the right supraclavicular region measuring 7.9 cm × 7.9 cm × 7.7 cm, with normal exiting nerves (Figure 1). A fine needle aspiration showed spindle cell neoplasm consistent with schwannoma.
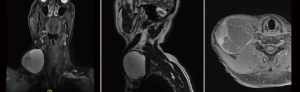
The patient was advised that surgical excision of the tumour was the most appropriate treatment to which he consented. A curvilinear incision was placed over the mass, the overlying soft tissue was separated and the surface of the lesion was carefully dissected from its attachment to the nerve sheath. The tumor measured 8 cm × 8 cm, was solid-cystic in nature with brownish fluid content. It was compressing the brachial plexus and there was thinning of the lower main trunk. The division and associated nerves were anatomically in continuity and no evidence of any defects was observed (Figure 2).

Post operatively, the patient had an uncomplicated recovery with no signs of weakness of the right upper limb. Over the following 3–5 days, the patient reported return of sensation over his right thumb and index finger, and the tingling sensation over his forearm had disappeared.
Discussion
Brachial plexus tumors are rare entities that comprise <5% of all tumors of upper extremities (3). The most common benign peripheral nerve sheath tumor (PNST) arising from the brachial plexus is neurofibromas, which are usually associated with neurofibromatosis type I (4). Schwannomas, are the second commonest PNST, of which, only 5% arise from the brachial plexus (5).
Schwannomas are slow growing, benign, encapsulated masses arising from Schwann cells. Their indolent nature typical presentation is as a painless, symptomless, solitary mass. Patients may present with nerve compression symptoms, less commonly with radiating pain and sensory or motor deficit (6). In contrast to neurofibromas, schwannomas may demonstrate cystic areas of degeneration and hemorrhagic necrosis (1,7). Grossly, they may be round, oval or plexiform in shape and may have a yellow or gray colour (7). Histologically, areas of dense spindle cells (Antoni A) and loosely arranged cells (Antoni B) may be seen (8).
The recommended approach to investigating a large cystic neck mass, is to initially proceed with a contrasted computed tomographic (CT) scan to differentiate between a vascular and nonvascular tumour (1). Once the mass is confirmed to be nonvascular in origin, it is advised to proceed to perform a fine needle aspiration cytology (FNAC) to distinguish between malignant and benign neoplasms. A magnetic resonant imaging (MRI) will further assist to delineate the features of the mass, help distinguish neurologic or non-neurological tissue and act as a road map during surgery.
Surgical excision, is recommended as the first choice of treatment, for tumors causing neurological deficit, discomfort, progressively increasing in size with a suspicion of malignancy and to prevent or minimize neural damage (7,9). Complete resection of the tumor with preservation of the nerve is the ideal goal. As schwannomas are well encapsulated, it is almost always possible to enucleate and separate the tumor from the nerve sheath (10). Courvoisier reported the first surgical excision of a brachial plexus schwannoma in 1886, which was complicated post operatively with paralysis of the deltoid and biceps muscle (11). Complications reported in most case series are temporary sensory and motor deficit (12).
Schwannomas are reported to be radio resistant, and the potential for malignant change is extremely rare. Where the tumor is inoperable, radiotherapy may be considered as a palliative treatment (13).
Conclusions
Brachial plexus schwannomas are infrequently seen, and may present as a huge cystic neck mass. Aside from a palpable lesion, they are usually symptomless and slow growing. When faced with a fluctuant lateral neck mass, a branchial plexus schwannoma should be considered first on the differential diagnosis. Pathologically they are well encapsulated, which allows for complete excision. Total surgical removal is the recommended treatment, with preservation of the nerve trunk.
Acknowledgements
The authors would like to thank the Department of Otolaryngology, University Malaya Medical Centre for its continuous support.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Prasad R, Kumar V, Manohar SR. Extracranial Schwannomas of Head and Neck. J Otol Online 2014;4.
- Chang SC, Schi YM. Neurilemmoma of the vagus nerve. A case report and brief literature review. Laryngoscope 1984;94:946-9. [Crossref] [PubMed]
- Donner TR, Voorhies RM, Kline DG. Neural sheath tumors of major nerves. J Neurosurg 1994;81:362-73. [Crossref] [PubMed]
- Binder DK, Smith JS, Barbaro NM. Primary brachial plexus tumors: imaging, surgical, and pathological findings in 25 patients. Neurosurg Focus 2004;16. [Crossref] [PubMed]
- Ahn KM, Lee HK, Lee KD, et al. A case of neurilemmoma of the brachial plexus. J Korean Otolaryngol 2002;8:733-5.
- Go MH, Kim SH, Cho KH. Brachial plexus tumors in a consecutive series of twenty one patients. J Korean Neurosurg Soc 2012;52:138-43. [Crossref] [PubMed]
- Huang JH, Zaghloul K, Zager EL. Surgical management of brachial plexus region tumors. Surg Neurol 2004;61:372-8. [Crossref] [PubMed]
- Kumar A, Akhtar S. Schwannoma of brachial plexus. Indian J Surg 2011;73:80-1. [Crossref] [PubMed]
- Chen F, Miyahara R, Matsunaga Y, et al. Schwannoma of the brachial plexus presenting as an enlarging cystic mass: report of a case. Ann Thorac Cardiovasc Surg 2008;14:311-3. [PubMed]
- Horowitz J, Kline DG, Keller SM. Schwannoma of the brachial plexus mimicking an apical lung tumor. Ann Thorac Surg 1991;52:555-6. [Crossref] [PubMed]
- Lee HJ, Kim JH, Rhee SH, et al. Is surgery for brachial plexus schwannomas safe and effective?. Clin Orthop Relat Res 2014;472:1893-8. [Crossref] [PubMed]
- Ahmadi A, Hirbod H, Cheraghipoor M, et al. Schwannoma of the Brachial Plexus Presented as a Neck Mass: A Case Report and Review of the Literature. International Journal of Otolaryngology and Head & Neck Surgery 2015;4:104-7. [Crossref]
- Calcaterra TC, Rich JR, Ward PW. Neurilemoma of the sphenoid sinus. Arch Otolaryngol 1974;100:383-5. [Crossref] [PubMed]
Cite this article as: Kho JP, Prepageran N. Huge brachial plexus schwannoma, masking as a cystic neck mass. AME Case Rep 2018;2:41.


