
Spontaneous resolution of myopic retinoschisis
Introduction
Myopic retinoschisis is the splitting of the posterior retinal layers in highly myopic patients that can lead to vision loss. The mechanisms underlying myopic retinoschisis remain unclear. It is generally believed that progressive axial elongation in high myopic eyes can lead to chorioretinal stretching and deprives retinal nutrients. In this context, the retina becomes oxygen starved and increases retinal vascular endothelial growth factor (VEGF) expression, contributing to ocular angiogenesis. The pathological neovascularity can leak fluid under or into the retina, causing macular oedema, retinal detachment and visual impairment (1). Because most of these eyes have already undergone structural changes, spontaneous resolution of myopic retinoschisis is a highly unusual event (2). Only a few dozen cases of non-surgical resolution of retinoschisis have been reported in the literature (2).
Case presentation
A 50-year-old highly myopic woman presented to our chiropractic clinic complaining of exacerbated neck pain and upper extremity numbness for a duration of 2 weeks. The patient was monocular OD, with a history of head contusion complicated by recurrent retinal detachment, chronic pain and glaucoma. The left eye had thus been enucleated 30 years prior. The right eye had long-standing myopic maculopathy, and undergone prophylactic laser therapy, cataract extraction and yttrium-aluminum-garnet (YAG) capsulotomy in the past few decades. Her vision impairment was depicted in ophthalmic studies, including visual field defects and features characteristic of myopic retinoschisis (Figures 1,2).

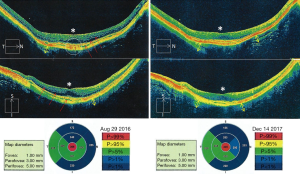
At presentation to our clinic, the patient had a guarded neck posture. The neck pain, rated to be 7/10 on verbal Numeric Pain Scale (NPS), was exacerbated with positions of flexion, extension and lateral bending. X-ray findings were consistent with degenerative cervical spondylolisthesis. Chiropractic approach was focused on correcting cervical instability and releasing nerve compression. The patient was treated with 3 sessions of cervical adjustment per week. As expected, the pain and numbness were reduced, and cervical range of motion (ROM) was increased 1 week after starting the manipulation. Throughout the 12 treatment sessions, the patient reported experiencing subjectively clearer and brighter vision in her right eye and the improvement had been ongoing during the 12 treatment sessions. Follow-up examinations confirmed an improvement in visual field status and almost complete resolution of her macular retinoschisis (Figures 1,2).
Discussion
The high-oxygen demand of the retina and the relatively sparse nature of the retinal vasculature make the retina vulnerable to ischaemia and hypoxia. Nevertheless, there are some survival factors in retinal ischaemia. In the normal eye, the choroidal circulation nurtures the outer retina, whereas the central retinal artery and its end branches feed the inner retina and mid-retina. Due to the connection between these two systems (3,4), the bipartite vascularization ensures minimum supply for retinal hemodynamics (5). Animal models have shown that the choroid supply of oxygen to the inner retina may be sufficient to maintain ganglion cell viability even when the retinal vessels have been completely obliterated (4).
Experimental data has suggested that preconditioning events (prior episodes of ischaemia) may induce “ischaemic tolerance” in the retina and result in reduced anatomical and functional damage (6,7). In this context, some retinal cells survive at an ischaemic level subthreshold for causing overt cell death, and hibernate in a poorly functioning mode. Upon improvement in blood supply and oxygenation of the surviving tissue, certain visual functions can be reactivated and restored (8-10). It is observed that if there is even minimal retinal circulation (8) or are islands of surviving tissue (9) after retinal damage, it is possible to obtain a considerable recovery of vision in these eyes. Spontaneous resolution of myopic retinoschisis may be a multifactorial cause, with changes in the scleral shape potentially playing a role (2). From a pathophysiologic point of view, restoration of retinal hemodynamics is a possible explanation for claims of visual improvement from many advocated therapies (11), including the possible efficacy of chiropractic adjustment (10).
Vision recovery has occasionally been reported after chiropractic manipulation in patients with various visual problems (12-14), however, none of the published reports has explained the reasons for the recovery in detail. In regard to our case, there was nearly full resolution of macular schisis, recovery of the retinal pigment epithelium, and altered choroidal thickness (Figure 2). Given that choroidal thickness is associated with ocular perfusion pressure (15), age (16) and myopic macular degeneration (17), it is possible that the morphological changes in OCT appearance reflect an improved choroidal circulation. The choroid is innervated by both divisions (the sympathetic and the parasympathetic vasodilators) of the autonomic nervous system (18). We speculate that cervical manipulation may have induced a shift in the sympathetic and parasympathetic interaction (19,20), and might further adjust the choroidal haemodynamics. Even a minimal improvement of blood supply may be of great importance for vulnerable end-organs.
The present study is limited by its retrospective nature and by its single-patient observation. The items of observation lack prospective designs. There is no vascular imaging to be confirm that neck manipulation alone can predictably lead to improvement in ocular blood flow. Overtimes, in repeat visual field examination, the second exam shows better results due to the learning effect. The change of the central scotoma of our patient (Figure 1) was considered as near full recovery of the macular schisis. Furthermore, the notable changes shown on OCT are supportive, reflecting a spontaneous resolution of myopic retinoschisis. This study could contribute to further understanding of the connection between retinal morphology and alteration of visual function.
Conclusions
We report a spontaneous anatomic and visual improvement, in a myopic eye with macular retinoschisis, following 12 cervical spinal adjustments. The exact mechanism of recovery remains unclear. Limited reports and obscure references make it not possible to generalize the efficacy of chiropractic manipulation for patients suffering from macular retinoschisis.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Meng B, Zhao L, Yin Y, et al. Internal limiting membrane peeling and gas tamponade for myopic foveoschisis: a systematic review and meta-analysis. BMC Ophthalmol 2017;17:166. [Crossref] [PubMed]
- Hoang QV, Chen CL, Garcia-Arumi J, et al. Radius of curvature changes in spontaneous improvement of foveoschisis in highly myopic eyes. Br J Ophthalmol 2016;100:222-6. [Crossref] [PubMed]
- Muthaian R, Minhas G, Anand A. Pathophysiology of stroke and stroke-induced retinal ischemia: emerging role of stem cells. J Cell Physiol 2012;227:1269-79. [Crossref] [PubMed]
- Patz A. Oxygen inhalation in retinal arterial occlusion. Am J Ophthalmol 1955;40:789-95. [Crossref] [PubMed]
- Berrones D, Salcedo-Villanueva G, Morales-Cantón V, et al. Changes in retinal and choroidal vascular blood flow after oral sildenafil: An optical coherence tomography angiography study. J Ophthalmol 2017;2017:7174540. [Crossref] [PubMed]
- Junk AK, Rosenbaum PS, Engel HM, et al. Visual recovery after central retinal artery occlusion (CRAO) - A new pathophysiologic approach to the clinical entity of partial CRAO. Invest Ophthalmol Vis Sci 2003;44:4055.
- Roth S, Dreixler JC. Ischemic pre- and post-conditioning in the retina. In: Gidday J, Perez-Pinzon M, Zhang J. Editors. Innate Tolerance in the CNS. Springer Series in Translational Stroke Research. New York: Springer, 2013:541-50.
- Watson PG. The treatment of acute retinal arterial occlusion. In: Cant JS. Editor. The Ocular Circulation in Health and Disease. London: Kimpton, 1969:234-5.
- Sabel BA, Henrich-Noack P, Fedorov A, et al. Vision restoration after brain and retina damage: the residual vision activation theory. Prog Brain Res 2011;192:199-262. [Crossref] [PubMed]
- Terrett AG. Cerebral dysfunction: a theory to explain some of the effects of chiropractic spinal manipulation. Chiropractic Technique 1993;5:168-73.
- Brown GC, Magargal LE, Simeone FA, et al. Arterial obstruction and ocular neovascularization. Ophthalmology 1982;89:139-46. [Crossref] [PubMed]
- Gorman RF. Monocular vision loss after closed head trauma: immediate resolution associated with spinal manipulation. J Manipulative Physiol Ther 1995;18:308-14. [PubMed]
- Wingfield BR, Gorman RF. Treatment of severe glaucomatous visual field deficit by chiropractic spinal manipulative therapy: a prospective case study and discussion. J Manipulative Physiol Ther 2000;23:428-34. [Crossref] [PubMed]
- Zhang CJ, Wang Y, Lu WQ, et al. Study on cervical visual disturbance and its manipulative treatment. J Tradit Chin Med 1984;4:205-10. [PubMed]
- Kim M, Kim SS, Kwon HJ, et al. Association between choroidal thickness and ocular perfusion pressure in young, healthy subjects: enhanced depth imaging optical coherence tomography. Invest Ophthalmol Vis Sci 2012;53:7710-7. [Crossref] [PubMed]
- Hirata M, Tsujikawa A, Matsumoto A, et al. Macular choroidal thickness and volume in normal subjects measured by swept-source optical coherence tomography. Invest Ophthalmol Vis Sci 2011;52:4971-8. [Crossref] [PubMed]
- Kang SH, Hong SW, Im SK, et al. Effect of myopia on the thickness of the retinal nerve fiber layer measured by Cirrus HD optical coherence tomography. Invest Ophthalmol Vis Sci 2010;51:4075-83. [Crossref] [PubMed]
- Nickla DL, Wallman J. The multifunctional choroid. Prog Retin Eye Res 2010;29:144-68. [Crossref] [PubMed]
- Budgell B, Hirano F. Innocuous mechanical stimulation of the neck and alteration in heart-rate variability in healthy young adults. Auton Neurosci 2001;91:96-9. [Crossref] [PubMed]
- Welch A, Boone R. Sympathetic and parasympathetic responses to specific diversified adjustments to chiropractic vertebral subluxations of the cervical and thoracic spine. J Chiropr Med 2008;7:86-93. [Crossref] [PubMed]
Cite this article as: Chu EC, Pong JC. Spontaneous resolution of myopic retinoschisis. AME Case Rep 2019;3:3.


