A rare case of ectopic chest-wall thymoma: a case report
Introduction
Thymomas are the most common anterior mediastinal tumors (1,2). Ectopic thymomas are rare events, taking up only 4% of all thymomas (3,4). The most common locations for ectopic thymomas are the neck, middle, and lung (5,6), whereas the chest-wall location is extremely rare, and only a few cases have been reported, which were all identified as hamartomatous thymomas and hemangioendotheliomas (7-9). Ectopic chest-wall thymomas can cause substantial diagnostic difficulty because of its location and atypical symptoms. Here a case of an ectopic chest-wall thymoma was reported, which was resected and correct postoperative diagnosis. Besides, type B1 was confirmed according to 2018 World Health Organization (WHO) histological classification.
Case presentation
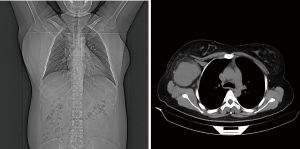
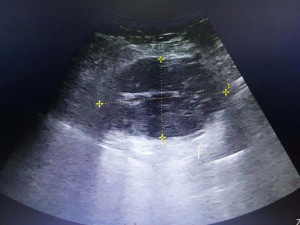
A healthy 32-year-old woman visited our hospital to detect an ever-growing subaxillary mass about 7 months but with no other symptoms. She first came to galactophore department when the mass was of the similar size to an egg and diagnosed as accessory breast 6 months ago. Subsequently, she had on medication for half a year, but it did not work very well. Because of persistent enlarging mass, she went to see a thoracic surgeon this time. On physical examination, a right subaxillary mass occupied subcutaneous, and a movable elastic lump can be touched. On image diagnosis, chest computed tomography showed a soft tissue tumor in the thoracic wall of right armpit (largest dimensions, 63 mm × 85 mm, Figure 1). Ultrasound showed a hypoechoic mass (dimensions, 78 mm × 48 mm) in the chest wall of right subcutaneous, boundaries are explicit (Figure 2). A hematological examination indicated some normal findings, including normal tumor marker levels and CBC (WBC 3.37×109/L, RBC 4.58×1012/L, CA153 14.6 U/mL, CA125 6.4 U/mL, CA724 2.9 U/mL, AFP 3.8 IU/mL). She also had no symptoms of specificity but only compression. Judgment of the nature of the mass and the treatment are the key.
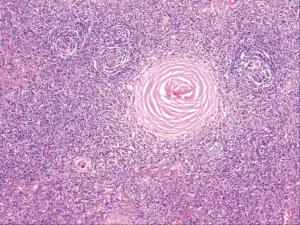
According to her medical inspection, the patient was recommended for a surgery treatment and went through. Thus, the tumor resection was performed in a short period. The tumor was easily dissected from adjacent structures and completely removed. The postoperative histopathological findings showed germinal center, abundance of immature lymphocytes and calcification. Immunohistochemical results also showed that the expression of CD3, CD20 and CD5 in interfollicular area revealed positive. Based on morphological and immunohistochemical results, the tumor was confirmed as a type B1 thymoma according to the 2018 WHO histological classification (Figure 3). The tumor cell had no invasion to fat tissues around the capsule membrane of the tumor equivalent to Masaoka stage I.
The patient was healed from surgery and discharged a week later. Six months after the operation, the patient was in good condition and no recurrence was found by examination.
Discussion
During the embryonic period, the thymus develops from the third and fourth pharyngeal pouches and descends caudally with the third parathyroid into the anterior mediastinum by the fifth or sixth week of gestation (1). Ectopic thymomas may develop from relevant origin that along this pathway. Most previous reports have indicated that the ectopic thymoma was located in the neck, the thyroid and supraclavicular region, while a few reports have indicated that the ectopic thymoma was originated in the lung, mediastinum or pleura (10-12). The most common ectopic position is the middle mediastinum. In the past literatures, 5 types ectopic thymomas were reported, namely typical, carcinoma, hamartomatous, hemangioendotheliomas and spindle sarcomatous (13). In the case, the treatment of an ectopic chest-wall thymoma for a woman patient was summarized, the tumor was removed and classified type B1. Thus far, there have been no reports of typical pathological types of ectopic chest-wall thymomas.
Our report provides a reference for those chest masses that symptoms are atypical. ectopic chest-wall thymomas are difficult to identify for unspecific symptoms. Its accurate diagnosis depends on pathological findings, and a biopsy may be taken if necessary. Main treatment is surgery and subsequent treatment, depending on the pathological classification.
In this study, though the operation was finally performed and correctly diagnosed, and the patient was cured and discharged, what are the areas that are specific to our diagnosis and treatment, namely, if a similar case is encountered next time, which areas can be identified for diagnosis?
We think this specificity is minimal, yet some features should be noted. First, the growth time and rate of the mass should be noticed, an increase in the rate within half a year suggests a possible tumor factor. In addition, the growth area is critical. Most previous reports have indicated that the ectopic thymoma was located in the neck, the thyroid and supraclavicular region, while a few reports have suggested that the ectopic thymoma originated from the lung, mediastinum or pleura (10-12). Besides, there are rare reports of ectopic extrathoracic thymoma that developing from the chest wall (7-9). Lipoma, chondroma and metastatic tumor often occur on the chest wall. Accordingly, facing the optional to the breast wall of mass, tumor factor is the priority. Early biopsy and surgical treatment are necessary. Besides, when it is diagnosed as an ectopic thymus tumor after operation, the relation between ectopic tumor and its’ primary site should be noted. In this case, the primary site of the thymus gland was not abnormal, but that’s not definite in all cases. In additions, in metastatic tumors, we should find the primary sites of the tumors in time. We should combine clinical symptoms to make a diagnosis, for example, symptoms of myasthenia gravis and hypothermia help to indicate thymus tumors and chest wall tuberculosis. When no abnormality was found by routine examination, we should do pathological examination as soon as possible. Furthermore, neither imaging nor laboratory testing is highly specific, calcification in mass is also not representative. In terms of clinical symptoms, the symptoms of myasthenia gravis and chest pain are not obvious. So, when we are facing similar cases again, if there is no obvious clinical specificity, priority should be given to the biopsy, making the best clinical decisions and guiding treatment.
Some experts once analyzed the morphology and clinical behavior of neck tumors, they classified ectopic cervical thymoma into four subtypes: hamartomatous thymoma, typical, spindle epithelial tumor with thymus-like differentiation, and carcinoma showing thymus-like differentiation (13), but this classification has not been proposed in ectopic chest thymoma. So, is it possible that this subtype existing in the chest thymoma or having a similar subtype in the chest? Or try to classify ectopic chest thymoma?
Those subtypes in ectopic cervical thymoma according from pathological types, rather than position or gross morphology. We think it is likely that this subtype existing in chest. Hamartomatous thymomas, typical, spindle and sarcomatous, carcinoma and hemangioendotheliomas were reported (7-9,14), and other tissue types may be discovered later. If the subtypes depend on pathology, chest subtypes may resemble neck or may be exists a new type. If try to class ectopic chest thymoma, both intrathoracic and extrathoracic, lung and mediastinum should be contained, not only chest wall. Besides, from the current literatures, this similar classification is not valid in the chest wall but may exists in chest. Reports from the ectopic chest-wall thymomas are rare, and the most typical thymic tumors has not been reported much, let alone some rare types. Thus, the prudent classification is to refer to NCCN guides of 2018 version 2 and reported literatures. If try to classify those tumors, types can be classified to typical, carcinoma, hamartomatous and unusual types (hemangioendotheliomas and spindle sarcomatous). In addition, if you classify ectopic chest-wall thymomas from pathological types, the literatures are rare. But there are some aspects guiding other classifications, such as location, size and benign and malignant. From the location classification, anterior chest-wall location, lateral chest-wall location and posterior chest-wall location exists. Chest wall, mediastinum, lung and pleura can also be divided. From the size classification, massive type, nodular type and microminiature exists. Still, these types of classifications exist only in theory. Subsequent studies may have more reasonable classifications.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this Case Report and any accompanying images.
References
- Filosso PL, Delsedime L, Cristofori RC, et al. Ectopic pleural thymoma mimicking a giant solitary fibrous tumour of the pleura. Interact Cardiovasc Thorac Surg 2012;15:930-2. [Crossref] [PubMed]
- Moran CA, Travis WD, Rosado-de-Christenson M, et al. Thymomas presenting as pleural tumors. Report of eight cases. Am J Surg Pathol 1992;16:138-44. [Crossref] [PubMed]
- Amodeo G, Cipriani O, Orsini R, et al. A rare case of ectopic laterocervical thymoma. J Craniomaxillofac Surg 2013;41:7-9. [Crossref] [PubMed]
- Fushimi H, Tanio Y, Kotoh K. Ectopic thymoma mimicking diffuse pleural mesothelioma: a case report. Hum Pathol 1998;29:409-10. [Crossref] [PubMed]
- Lee SN, Cho MS, Koo H, et al. Ectopic hamartomatous thymoma: a case report showing CD99+ lymphocytes and a low proliferation index. Arch Pathol Lab Med 2003;127:e378-81. [PubMed]
- Weissferdt A, Moran CA. Ectopic primary intrathyroidal thymoma: a clinicopathological and immunohistochemical analysis of 3 cases. Hum Pathol 2016;49:71-6. [Crossref] [PubMed]
- Jing H, Wang J, Wei H, et al. Ectopic hamartomatous thymoma: report of a case and review of literature. Int J Clin Exp Pathol 2015;8:11776-84. [PubMed]
- Li L, Zhang WY, Liu WP. Heterotopic dislocation thymoma with differentiation of skin appendages. Zhonghua Bing Li Xue Za Zhi 2016;45:128-9. [PubMed]
- Pai KR, Thonse VR, Azadeh B, et al. Ectopic thymoma of the chest wall. Interact Cardiovasc Thorac Surg 2005;4:9-11. [Crossref] [PubMed]
- Cohen JB, Troxell M, Kong CS, et al. Ectopic intrathyroidal thymoma: a case report and review. Thyroid 2003;13:305-8. [Crossref] [PubMed]
- Skoutelis K, Nikolopoulos DD, Markopoulos K, et al. Ectopic thymoma of the lung; a rare case report and review of the literature. Cases J 2009;2:9149. [Crossref] [PubMed]
- Kitada M, Sato K, Matsuda Y, et al. Ectopic thymoma presenting as a giant intrathoracic tumor: a case report. World J Surg Oncol 2011;9:66. [Crossref] [PubMed]
- Chan JK, Rosai J. Tumors of the neck showing thymic or related branchial pouch differentiation: a unifying concept. Hum Pathol 1991;22:349-67. [Crossref] [PubMed]
- Matsuoka K, Murata Y, Ueda M, et al. Ectopic thymic carcinoma presenting as an intrathoracic mass. Asian Cardiovasc Thorac Ann 2016;24:480-3. [Crossref] [PubMed]
Cite this article as: Cao X, Lin R, Han B, Chen C. A rare case of ectopic chest-wall thymoma: a case report. AME Case Rep 2019;3:18.