This article has an erratum available at: http://dx.doi.org/10.21037/acr-2021-01 the article has been update on 2021-12-09 at here.
Surgical treatment of kidney tumor on a patient with second case of staghorn calculus and associated renal hydronephrosis: case report
Introduction
Staghorn, struvite or coral calculus are the ones that completely or partially occupies the renal pelvis and branches to the renal calices. It is most likely associated with recurrent urinary tract infections and the presence of urea-splitting bacteria, with Proteus mirabilis being one of the most common species (1). The presence of this kind of calculi may lead to a decrease of the renal function due to pyelonephritis that could result on the loss of the affected kidney's function (2,3). Furthermore, the presence of renal calculi of any kind in the urinary tracts is related to the appearing of malign tumor in the kidneys, especially in the absence or failed treatment (4). The following case reports a patient that presents both complications in both kidneys, something rare in the current literature and with complicated progress. Written informed consent was obtained from the patient for publication of this Case Report and any accompanying images.
Case presentation
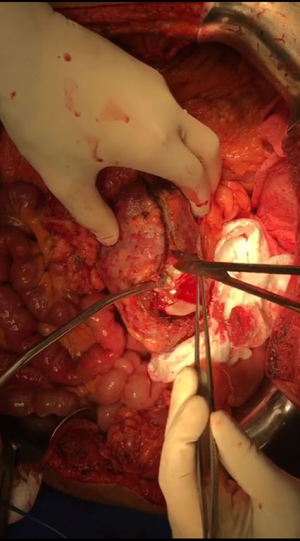
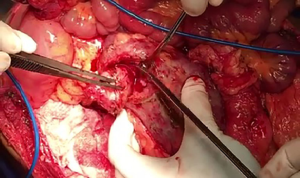
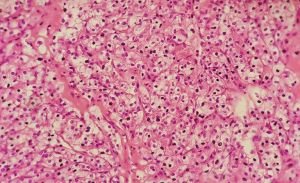
A male patient, 51 years old, native of Manaus, reports dysuria and polyuria associated with constant fever episodes and urinary tract infections with improvement by using several antibiotics but returning the symptoms after suspending it; evolving over a year with left flank and back pain and spreading out to the left inguinal region and testicle associated with anemia displayed at routine exams. The patient reports a surgical treatment 12 years ago for treating a staghorn calculus in the right kidney with similar symptoms, at the time in another hospital, but without further medical assistance after the procedure, even though claiming an improvement of the symptoms. He denies drug allergies, familiar history of calculus and cancer or any other comorbidities. He confirmed that after the first episode of staghorn calculi, he increased water intake, but did not maintain the same way over time. Six months after the beginning of his condition, during an ambulatory visit, it was requested a complete abdominal tomography with emphasis in the urinary system, blood and urine tests for clinical association, in addition to non-steroidal anti-inflammatory medicines. The patient return was in a month and no improvement of the pain in the patient’s feeling, with the tomography image tests result showing atrophy in the right kidney, which presents dilatation of the collector system, that it’s filled with material with density varying between thick liquid and soft parts (average of 45 UH), in addition to calculus in the pelvis and ureteropelvic junction, suggesting a pattern for xanthogranulomatous pyelonephritis and matching previous history of right staghorn calculus (Figure 1). The left kidney presented normal dimensions, exophytic nodule in the lower pole measuring 3.4 cm × 2.8 cm with contrast enhancement similar to renal parenchyma, associated with a simple cortical cyst and a large staghorn calculus (6.0 cm × 3.5 cm) in this kidney, with average density of 300 UH, 7.7 cm distant from the pelvis, causing dilatation of superior caliceal group in this kidney. Presented abnormal test results for urea with 109 mg/dL and creatinine with 4.4 mg/dL. It was decided for partial left nephrectomy and total right nephrectomy, considering that it had significant hydronephrosis, a relevant decrease in the parenchyma and, mainly, being an infectious focus. The patient also had history of several episodes of urinary infection resistant to antibiotics, presenting potential risk of sepsis. The incision made was bilateral subcostal, followed by exploration and control of right renal hilum. The right kidney presented with hydronephrosis, although with rigid consistency and intense inflammatory process. Total right nephrectomy was performed. After that, partial left nephrectomy began, with isolation and controlling of the left renal hilum vessels, performing for excision of the renal nodule of the upper pole, followed by anatrophic nephrolithotomy with Brödel’s line incision, that revealed great purulent discharge escape (about 500 milliliters) (Figures 2-4). Staghorn calculus was removed with double-J stent implanted in left ureter and layer suture performed. The surgery went through eight hours and was attended by nephrology service of the same hospital. In the following four days after the procedure, the patient was maintained under observation in the intense therapy unity, performing dialysis every two days, with progressive improvement of the pain and operative wound with great appearance. The left renal function showed constant increasing during the dialysis. On the fifth post-operative day, the patient returns to the urology nursery care with renal function still impaired but presenting diuresis of 1,500 milliliters per day on average. In the seventh day presented obvious hematuria by Foley catheter, needing a successful bladder washing. The patient was discharged from hospital in the 12th post-operative day with pain improvement and clear renal function progress, not needing continuous post-operative dialysis. The anatomopathological examination of the left kidney showed renal cell carcinoma, clear cell type, with nuclear grade of Führman 1, measuring 25 cm in larger diameter (5) (Figure 5). The right kidney just showed hydronephrosis without neoplasms signs.
Discussion
Cases like this tend to have unwanted outcomes, considering the high possibility of the patient progress to death due to the large-scale procedure and the great risk of complications, besides the possibly evolution to renal function loss and consequent need for dialysis for the rest of life. The presence of xanthogranulomatous pyelonephritis in the atrophied right kidney is rare when associated with the fact that the presence of previous coral-like calculi is the cause of the renal atrophy, however it’s a risk factor to complications like sepsis and necrosis of the renal tissue (6). The emergence of staghorn calculus can be bilateral, which means the continuous monitoring of patients that presented calculus in only one kidney and the previous report of the occurrence of new calculus during life. The recurrent infection factor is also a warning factor for those patients, as it can grow to renal failure and the overload from continuous use of antibiotics. In the reported case, the patient was already presenting purulent discharge in both kidneys, which leads to think of a chronic infection case for the staghorn calculus as in an atrophied kidney, another source of bacterial growth due to the decreasing blood flow in the region. The monitoring must always have the assistance of the nephrology service, since the need of post-operative dialysis is almost certain, because apart from the nephrectomy itself, the renal tissue goes through ischemia periods during the procedure. The incidence of carcinoma concomitant with the presence of renal calculus may occur due to the constant inflammatory reaction, especially if the patient presents with constant renal calculi or staghorn type with repetitive urinary infections. However, despite this well-defined pathophysiology, few studies have related the staghorn calculi with the incidence of clear cell adenocarcinoma. A case report related the long-term renal calculus renal with carcinoma, different from the case reported here, besides the anatomical location, the diagnostic of carcinoma was found only after nephrolithotomy (7).
Conclusions
The association between kidney cancer and staghorn calculus should be consider through the treatment. Patients with renal diseases of severe prognosis in both kidneys must be kept under constant surveillance by the urology and nephrology team, the association of both clinics is essential to a fortunate ending like the case reported. To better assist the patient, it must be performed a research of the urinary component that may induce the emergence of new calculus after surgical treatment, what could have avoided the complication presented in this article.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Sallami S, Zrayer O, Mizouni H, et al. Association of renal cell carcinoma and staghorn calculi complicated with emphysematous pyelonephritis. Tunis Med 2014;92:235-7. [PubMed]
- Jain A, Mittal D, Jindal A, et al. Incidentally detected squamous cell carcinoma of renal pelvis in patients with staghorn calculi: case series with review of the literature. ISRN Oncol 2011;2011:620574. [Crossref] [PubMed]
- Jongyotha K, Sriphrapradang C. Squamous Cell Carcinoma of the Renal Pelvis as a Result of Long-Standing Staghorn Calculi. Case Rep Oncol 2015;8:399-404. [Crossref] [PubMed]
- Cheungpasitporn W, Thongprayoon C, O'Corragain OA, et al. The risk of kidney cancer in patients with kidney stones: a systematic review and meta-analysis. QJM 2015;108:205-12. [Crossref] [PubMed]
- Moch H, Humphrey PA, Ulbright TM, et al. WHO Classification of Tumours of the Urinary System and Male Genital Organs. Fourth edition. WHO/IARC Classification of Tumours, Volume 8. Lyon, France: International Agency for Research on Cancer, 2016.
- Tseng CW, Chen WNJ, Juang GD, et al. Staghorn calculi and xanthogranulomatous pyelonephritis associated with transitional cell carcinoma. Urol Sci 2015;26:69-71. [Crossref]
- Sivaramakrishna B, Aron M, Ansari MS, et al. Squamous cell carcinoma of the renal pelvis manifesting after percutaneous nephrolithotomy for long standing calculus. Int Urol Nephrol 2004;36:149-51. [Crossref] [PubMed]
Cite this article as: Alves RA, Barroso FM, de Andrade GF Jr, Façanha Neto CD, Brito FC, Takeda AN, da Costa Neto EF, Costa TM, Rodriguez JE, Caminha RC, Santana MF, Paiva CS, de Sousa FA. Surgical treatment of kidney tumor on a patient with second case of staghorn calculus and associated renal hydronephrosis: case report. AME Case Rep 2019;3:19.