
Perforated ileus after L5-S1 anterior lumbar interbody fusion: a case report presentation
Introduction
Various approaches exist to treat lumbar spine pathology. Each method has its advantages and disadvantages. The anterior approach to the lumbar spine allows for direct and efficient access to the anterior column and may be indicated for degenerative pathologies of the lumbar spine including instability, chronic pain, and deformity (1,2). Studies have shown reduced blood loss, shorter operative times, and shorter hospital stays when compared to posterior approaches (1).
In anterior lumbar surgery, there is no damage to posterior spinal musculature and ligaments, which may lead to faster patient recovery. Other studies have shown increased complication rates of ileus, pneumonia, deep venous thrombosis, and infection when compared to posterior approaches (2-4). The rate of ileus after anterior lumbar interbody fusion (ALIF) has been reported in the literature to be between 3% and 5.44% (5). To our knowledge, there have been no reports of a bowel perforation after postoperative ileus in patients who have undergone ALIF (1,5,6).
The objective of this paper is to discuss the postoperative clinical course of a patient who developed a postoperative ileus complicated by subsequent bowel perforation after undergoing L5-S1 ALIF and to review the literature related to the colonic perforation resulting from postoperative ileus.
Case presentation
The patient is a 72-year-old male with a symptomatic history of severe chronic pain in bilateral buttocks and lumbosacral regions as well as a prominent L2 spinous process. His past medical history included hypertension, hyperlipidemia, gastroesophageal reflux disease, nephrolithiasis, deep venous thrombosis, and severe postoperative constipation after prior surgery, which was successfully treated with conservative management. His surgical history included bilateral inguinal hernia repair, removal of nephrolithiasis, and multiple posterior spinal surgeries resulting in fusion from L2-L5. He had continued symptoms of lumbosacral spondylosis with failure of nonoperative management including physical therapy, injections, and pharmaceutical therapy. Radiographic (Figure 1) and MRI findings were consistent with degenerative disc disease of L5-S1 and evidence of successful fusion L2-L5.

After an appropriate discussion regarding the risks and benefits of surgical intervention, the patient underwent a L5-S1 ALIF with posterior instrumentation, removal of hardware L2-3 with fusion exploration, and removal of a prominent L2 spinous process. A highly experienced vascular surgeon performed the anterior approach and was present for the entire anterior portion of the case. There were no apparent intraoperative complications. The peritoneum was not violated. The patient was admitted to the hospital after surgery for therapy, pain control, and medical management. He was initially placed on intravenous opioid pain medication for pain control and placed on “ice chips and sips of water” only per ALIF surgery postoperative protocol.
On postoperative day 1, the patient had flatus, his diet was advanced, and he did have a small bowel movement. On postoperative day 2 the patient had severe abdominal pain and distension with hypoactive bowel sounds. At this point, the general surgery service was consulted. No abnormalities were noted in his laboratory values. Radiographic findings (Figure 2) were consistent with postoperative ileus with no evidence of obstruction or pneumoperitoneum. He received bisacodyl suppositories, was encouraged to ambulate, and started on a clear liquid diet.

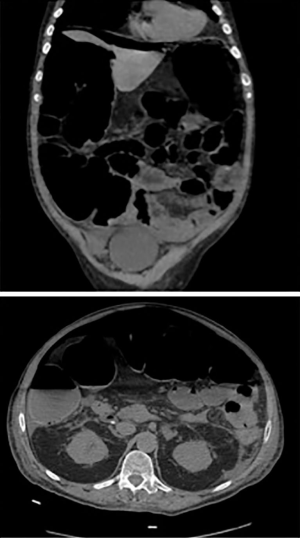
On postoperative day 5, the patient suddenly experienced an acute exacerbation of abdominal pain. An upright abdominal radiograph (Figure 3) demonstrated findings consistent with free air under the diaphragm. A computed tomography scan of the abdomen (Figure 4) demonstrated pneumoperitoneum and dilation of the large and small bowel extending to the splenic flexure. Of note, there was no apparent orthopaedic implant complications or suspicion of mechanical obstruction. He was started on antibiotics and was taken to the operating room by general surgery for an exploratory laparotomy. Intra-operative findings were significant for multiple abdominal adhesions and multiple pinhole sized perforations at the splenic flexure and cecum. Suture repair of all perforations and an adhesiolysis was performed. A nasogastric tube was placed at the end of surgery.

On postoperative day 4 from the exploratory laparotomy, the patient began to have flatus. At this point, the nasogastric tube was removed and his diet was advanced to clear liquids. On postoperative day 5 from exploratory laparotomy, his bowel function returned and he was tolerating soft foods. He was discharged from the hospital to an inpatient rehab facility on postoperative days 12 and 7 from the spine surgery and exploratory laparotomy, respectively. At follow-up appointments at 6 weeks and 6 months, the patient had been doing well and was eating a normal diet with normal bowel function.
Discussion
Selection of an anterior approach is determined by patient-specific pathology and surgeon preference. Several studies have shown that the anterior approach may provide better access to the anterior disc space, decreased trauma to posterior structures, decreased blood loss, increased fusion rates (1), and better stability secondary to availability of larger interbody devices (5,7-9). The anterior approach is not without its complications. Current studies have shown increased rates of infection, injury to major vascular structures, and gastrointestinal complications (2-4,8). The rate of postoperative ileus after anterior approach has been found to be more than 2 times that of a posterior approach (2).
Acute colonic pseudo-obstruction (ACPO) is characterized by acute dilation of the large bowel in the absence of any mechanical obstruction (9). It is also known as acute colonic ileus or Ogilvie’s syndrome. It is associated with many metabolic, surgical, and pharmacologic factors. Diagnosis of ACPO is typically made by clinical presentation of abdominal distension, constipation, nausea, and vomiting. Bowel sounds may or may not be present. The pathogenesis is not completely understood but likely results from autonomic dysregulation of colonic motor function (10). ACPO is typically treated conservatively, which includes treating the underlying disease such as correcting underlying electrolyte abnormalities, discontinuing drugs causing gastric hypomotility, increasing hydration, ambulation, and encourage use of bowel stimulating medications. Administration of neostigmine is considered in severe cases to stimulate bowel function. Neostigmine is an anticholinesterase inhibitor, which allows an increase in acetylcholine availability and parasympathetic activity. This results in increased colonic peristalsis. It should be used cautiously in patients at risk for severe bradycardia (6). When conservative treatment fails, decompression is required via colonoscopy or a transrectal tube. Decompression of the colon is used to decrease the parietal tension, increasing blood flow, and promoting peristalsis to relieve symptoms. In severe cases, an increase in intraluminal pressure can cause bowel necrosis and eventual spontaneous perforation can occur, which has a mortality rate approaching 50% (10).
Postoperative ileus as a complication has been reported in orthopaedic and spine related surgery; however, perforation as a result of ileus is rare. It often affects older and debilitated patients, which explains the significant morbidity and mortality associated. Nunez et al. described a case where a patient had colonic perforation after a drug-related ileus, which required a large bowel resection (11). Khajehnoori et al. reported a case of caecal perforation after caesarean section requiring ileocolic resection and creation of a stoma (12). These represent the severe morbidity associated with bowel necrosis resulting from ACPO.
Risk factors for ACPO include trauma, electrolyte abnormalities, surgery, narcotic use, and infection. In this particular case, the patient had multiple risk factors for the development of postoperative ileus. The patient had a history of constipation following previous surgeries, was taking narcotic pain medication, and he had a history of abdominal surgery, all of which placed him at risk of developing ACPO. After considering the significant potential risks with posterior lumbar fusion in this patient secondary to scar tissue and altered anatomy, we decided to use an anterior approach. After developing a bowel perforation secondary to postoperative ileus, we treated the patient in an urgent manner, avoiding a bowel resection or diverting ostomy.
At our institution our current protocol for patients with postoperative ileus after ALIF is to initially make the patient nothing by mouth (NPO), obtain plain abdominal radiographs and labs including complete blood count (CBC) and complete metabolic profile (CMP). A general surgery consult is also obtained initially. Fluid resuscitation and electrolyte imbalances are corrected, all possible offending medications are discontinued, and nasogastric decompression is started while ambulation is encouraged. Neostigmine is not routinely used at our institution. Patients are followed closely with general surgery for return of bowel function and serial abdominal radiographs are obtained. Computed tomography is performed if mechanical obstruction is not ruled out or if symptoms fail to improve with conservative treatment. Mechanical decompression is considered for patients failing to improve with conservative treatment.
After review of this case, further recommendations include possible avoidance of anterior lumbar surgery in patients at increased risk of ACPO. More aggressive conservative treatment such as administration of neostigmine should be considered early in the nonoperative management. NG tube should be routinely considered, and if patients are not improving over 48–72 hours, further aggressive decompression should be considered either using a rectal tube, or colonoscopy per general surgery recommendations (10,13).
This report presents a unique case of bowel perforation resulting from postoperative ACPO after ALIF. We did not find a similar described case in the literature. Although an ileus is a common complication associated with lumbar spine surgery in general, this review reveals that bowel perforation after anterior lumbar spine surgery is a possible complication that surgeons should discuss with patients preoperatively, especially those with risk factors.
Acknowledgments
None.
Footnote
Conflicts of Interest: D Pahl declares that he is a shareholder in Trainer Rx, Nanovis, and Vertera. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Mobbs RJ, Loganathan A, Yeung V, et al. Indications for anterior lumbar interbody fusion. Orthop Surg 2013;5:153-63. [Crossref] [PubMed]
- Qureshi R, Puvanesarajah V, Jain A, et al. A Comparison of Anterior and Posterior Lumbar Interbody Fusions: Complications, Readmissions, Discharge Dispositions, and Costs. Spine (Phila Pa 1976) 2017;42:1865-70. [Crossref] [PubMed]
- Mobbs RJ, Phan K, Daly D, et al. Approach-Related Complications of Anterior Lumbar Interbody Fusion: Results of a Combined Spine and Vascular Surgical Team. Global Spine J 2016;6:147-54. [Crossref] [PubMed]
- Rothenfluh DA, Koenig M, Stokes OM, et al. Access-related complications in anterior lumbar surgery in patients over 60 years of age. Eur Spine J 2014;23 Suppl 1:S86-92. [Crossref] [PubMed]
- Quraishi NA, Konig M, Booker SJ, et al. Access related complications in anterior lumbar surgery performed by spinal surgeons. Eur Spine J 2013;22 Suppl 1:S16-20. [Crossref] [PubMed]
- Ponec RJ, Saunders MD, Kimmey MB. Neostigmine for the treatment of acute colonic pseudo-obstruction. N Engl J Med 1999;341:137-41. [Crossref] [PubMed]
- Crock HV. Anterior lumbar interbody fusion: indications for its use and notes on surgical technique. Clin Orthop Relat Res 1982.157-63. [PubMed]
- Goz V, Weinreb JH, Schwab F, et al. Comparison of complications, costs, and length of stay of three different lumbar interbody fusion techniques: an analysis of the Nationwide Inpatient Sample database. Spine J 2014;14:2019-27. [Crossref] [PubMed]
- Rao PJ, Loganathan A, Yeung V, et al. Outcomes of anterior lumbar interbody fusion surgery based on indication: a prospective study. Neurosurgery 2015;76:7-23; discussion 23-4. [Crossref] [PubMed]
- Saunders MD, Kimmey MB. Systematic review: acute colonic pseudo-obstruction. Aliment Pharmacol Ther 2005;22:917-25. [Crossref] [PubMed]
- Núñez-García E, Valencia-García LC, Sordo-Mejía R, et al. Drug related colonic perforation: Case report. Cir Cir 2016;84:65-8. [PubMed]
- Khajehnoori M, Nagra S. Acute colonic pseudo-obstruction (Ogilvie's syndrome) with caecal perforation after caesarean section. J Surg Case Rep 2016;2016. [Crossref] [PubMed]
- Daniels AH, Ritterman SA, Rubin LE. Paralytic ileus in the orthopaedic patient. J Am Acad Orthop Surg 2015;23:365-72. [Crossref] [PubMed]
Cite this article as: Mahoney JR, Barnes D, Pahl D. Perforated ileus after L5-S1 anterior lumbar interbody fusion: a case report presentation. AME Case Rep 2019;3:21.


