Al Wakra emergency presentation of Behcet’s disease
Introduction
Behcet’s disease or Behcet syndrome is an autoimmune disease with ocular, oral, genital, and dermatological manifestations. The primary cause of the symptoms is vasculitis that lead to damage of blood vessels. The condition is named after the Turkish doctor, Hulusi Behcet, who described this disease in modern medicine in 1937 (1).
The common and classic features of Behcet’s disease encompass a young male with recurrent oral ulcer, genital ulcer, skin lesions, and ocular manifestations. The disease is common in men than women and mostly found in the countries on the silk road (2).
Currently, a cure for this disease is absent, and the patient is required to administer corticosteroids for immunosuppression. Also, lidocaine and colchicine might be administered for symptomatic disorders (3).
The admitted to the Emergency Department presented various symptoms. The physicians had to treat and plan for diagnosis with a follow-up. The symptoms, signs, and history were recorded, followed by the early diagnosis that directed towards the final diagnosis.
Herein, we reported a case of a young patient presenting back pain concerning the right leg, a result of extensive bilateral deep vein thrombosis (DVT) in both legs that extended to inferior vena cava (IVC) and renal veins. After a bundle of investigations and medical examinations, the case was diagnosed as Behcet’s disease with an atypical presentation.
Case presentation
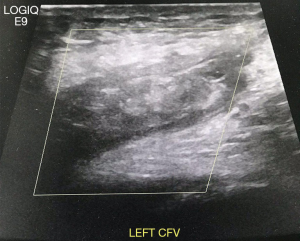
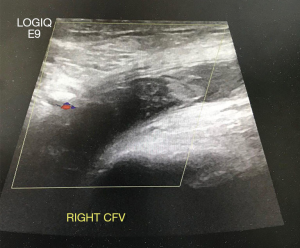
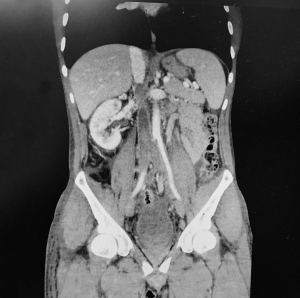
A 38-year-old male patient presented lower abdominal pain, which increased when he walked. The medical examination did not reveal any remarkable condition; thus, the patient was administered some medications and sent home. After 2 weeks he returned with non-traumatic lower back pain with respect to the right thigh. Further examination revealed an increased swelling on the right thigh. Then, the patient underwent blood investigation and Doppler ultrasound (US) of the right lower limb to exclude DVT. The patient had a history of intermittent fever. The laboratory results were not significant; however, the US showed bilateral DVT in both the lower limbs (see Figures 1 and 2) that extended to both iliac veins and IVC. Subsequently, the patient was admitted to the hospital, and the medical team carried out a bundle of investigations to exclude malignancies, TB, HIV, infections, and autoimmune diseases. Computed tomography (CT) of the abdomen and chest showed renal vein thrombosis (Figure 3), indicating a putative prostatic infection. Also, magnetic resonance imaging (MRI) confirmed the IVC thrombosis. The urologist also seconded the opinion on the CT result for the possibility of a prostatic infection. In addition, the examination of the patient revealed scrotal ulcer. Although this cleared from the possibility of having prostatitis, the collection at seminal vesicles was suspected. Next, the US, on the testes did not reveal any abnormality. Then, the patient was reevaluated by the medical and rheumatology teams that found: (I) recurrent oral ulcer; (II) the patient was not a smoker and had no medical history, but a history of recurrent oral and scrotal ulcer; (III) a few acne- type lesions on his back, and hence, the rheumatologists diagnosed it as Behcet’s disease. The CT angiography for pulmonary artery was normal. The transthoracic and trans esophageal echocardiogram (ECHO) did not present any remarkable features.
Discussion and review
Becket disease is an autoimmune disease with pan vasculitis, damaging the vessels throughout the body. The classical manifestation of Behcet’s disease is a young patient (male more than female) has recurrent oral ulcer, genital ulcers, and, ocular manifestation with skin lesion (4).
To diagnose this syndrome, the patient should have a recurrent attack of oral ulcer and at least two of the following manifestations: ocular-like retinal vasculitis, uveitis and hypopyon, recurrent attack of genital ulcer that heal by scarring, skin manifestations as acne form lesions, erythematous papule, and positive pathergy skin test (5).
Behcet’s disease is common in men than women and primarily found in the Silk Road countries from the Middle East to China, and currently, predominant in the USA (1,6).
Behcet’s disease may have critical manifestations such as vascular manifestations and lethal complication such as pulmonary embolism, aortic thrombosis, DVT, and cerebral stroke. The coronary artery disease might be detected in Becket’s disease, which is a result of vasculitis, thrombosis, and pericarditis. Pulmonary manifestations and complications have been reported as autoimmune plural effusion, pulmonary embolism, massive hemoptysis, and pulmonary hypertension (7-9).
The other manifestations might include genital ulcers: scrotal ulcer in men and vulva ulcer in women. Epididymitis was found in men and salpingitis was detected in women. The gastrointestinal manifestation of Behcet’s disease might be accompanied by abdominal pain and bloating of the abdomen that results in intestinal ulcer, which also affects the esophagus and ileocecal area. Arthritis and arthralgia occur in 60% of the patients mostly affect wrist, elbow, and ankle. In addition, mono arthritis or poly arthritis might also be noted (10-13).
The kidney and urinary tract systems might be affected; such as glomerulonephritis, proteinuria, amyloidosis, and renal vein thrombosis (14).
Some medical studies described the neurological type of Behcet’s disease. It was divided into the parenchymal tissue, which causes brain stem lesion, cerebral lesion, and spinal cord disease. On the other hand, the non-parenchymal disease causes like cerebral veins thrombosis and acute meningeal syndrome. Also, seizures, dysphagia, and mental changes have been reported (15).
In the Emergency Medicine Department at the Al Wakra Hospital, Hamad Medical Corporation in Qatar, we found the usual emergency complains like non traumatic back pain in young patients with no history of medical issues. Next, we investigated the patient and found severe causes such bilateral DVT that extended to Iliac veins and IVC, and directed him to medical examinations where he was diagnosed of Behcet’s disease based on (I) recurrent oral ulcer, (II) scrotal ulcer, (III) acne form lesion, (IV) the bilateral DVT also supported the diagnosis as suspected complication of Behcet’s disease. However, they did not request a pathergy test because the patient obtained the essential clinical score to be diagnosed with Behcet’s disease. Some of the Behcet’s disease patients have a negative pathergy test, and so, irrespective of the result of the pathergy test, the Behcet’s disease is based on the clinical diagnosis without a specific test (5).
The patient in the Emergency Department did not complain about oral or scrotal ulcer or skin lesion. Although the patient counteracted the recurrent oral ulcer and scrotal ulcer, he could not fight the lower back and leg pain.
The diagnosis of this case was a teamwork between the emergency medicine, radiology, internal medicine, urology, infectious disease, and rheumatology departments. Interestingly, the physician at thee Emergency Department is responsible for diagnosing and directing case to the appropriate care. The DVT might be one of the complications of Behcet’s disease. However, in emergency medicine, the lower back pain or lower abdominal pain might be considered as the key for diagnosis because the patients would not know be aware about DVT or IVC thrombosis, and hence, the lower abdominal pain with non-traumatic lower back pain might be one of the manifestations of the severe like Behcet’s disease. During the first visit, the patient complained of lower abdominal pain while walking only. Since the examination did not yield any adverse results, the patient was sent home with prescribed medicines. Strikingly, the reason underlying the lower abdominal pain only during walking could be iliac vein thrombosis. Thus, the lower abdominal pain and non-traumatic lower back pain should not be neglected, and the history, examination, and investigation of the patient should be the focus during the second visit. Furthermore, Behcet’s disease and autoimmune diseases should be considered if thromboembolism activity is observed in young patients.
Conclusions
Al Wakra emergency presentation of Behcet’s disease: non-traumatic lower back pain, thigh pain with swelling, or lower abdominal pain during walking that was due to bilateral DVT and thrombosis in iliac vein, IVC, and renal vein along with intermittent fever. They are vascular complications of Behcet’s disease. Behcet’s disease should be considered in thromboembolic manifestations in young patients.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The authors got the permission for publication of this case report from medical research center, Hamad Medical Corporation, Qatar. It was under Ref. No.: MRC-04-18-458.
References
- Mutlu S, Scully C. The person behind the eponym: Hulûsi Behçet (1889-1948). J Oral Pathol Med 1994;23:289-90. [Crossref] [PubMed]
- Savey L, Resche-Rigon M, Wechsler B, et al. Ethnicity and association with disease manifestations and mortality in Behçet's disease. Orphanet J Rare Dis 2014;9:42. [Crossref] [PubMed]
- Hatemi G, Silman A, Bang D, et al. EULAR recommendations for the management of Behçet disease. Ann Rheum Dis 2008;67:1656-62. [Crossref] [PubMed]
- Feigenbaum A. Description of Behçet's syndrome in the Hippocratic third book of endemic diseases. Br J Ophthalmol 1956;40:355-7. [Crossref] [PubMed]
- Davatchi F, Schirmer M, Zouboulis C, et al. Evaluation and Revision of the International Study Group Criteria for Behcet's disease. Proceedings of the American College of Rheumatology Meeting; November 2007; Boston, MA. Abstract 1233.
- Calamia KT, Wilson FC, Icen M, et al. Epidemiology and clinical characteristics of Behçet's disease in the US: a population-based study. Arthritis Rheum 2009;61:600-4. [Crossref] [PubMed]
- Hamuryudan V, Er T, Seyahi E, et al. Pulmonary artery aneurysms in Behçet syndrome. Am J Med 2004;117:867-70. [Crossref] [PubMed]
- Bayraktar Y, Balkanci F, Bayraktar M, et al. Budd-Chiari syndrome: a common complication of Behçet's disease. Am J Gastroenterol 1997;92:858-62. [PubMed]
- Ames PR, Steuer A, Pap A, et al. Thrombosis in Behçet's disease: a retrospective survey from a single UK centre. Rheumatology (Oxford) 2001;40:652-5. [Crossref] [PubMed]
- Seyahi E, Melikoglu M, Yazici H. Clinical features and diagnosis of Behcet's syndrome. Int J AdvRheumatol 2007;5:8.
- Kobayashi K, Ueno F, Bito S, et al. Development of consensus statements for the diagnosis and management of intestinal Behçet's disease using a modified Delphi approach. J Gastroenterol 2007;42:737-45. [Crossref] [PubMed]
- Kaklamani VG, Vaiopoulos G, Markomichelakis N, et al. Recurrent epididymo-orchitis in patients with Behçet's disease. J Urol 2000;163:487-9. [Crossref] [PubMed]
- Cho YH, Jung J, Lee KH, et al. Clinical features of patients with Behçet's disease and epididymitis. J Urol 2003;170:1231-3. [Crossref] [PubMed]
- Hemmen T, Perez-Canto A, Distler A, et al. IgA nephropathy in a patient with Behçet's syndrome--case report and review of literature. Br J Rheumatol 1997;36:696-9. [Crossref] [PubMed]
- Al-Araji A, Kidd DP. Neuro-Behçet's disease: epidemiology, clinical characteristics, and management. Lancet Neurol 2009;8:192-204. [Crossref] [PubMed]
Cite this article as: Elrobaa I, Elserhy M, Ahmad M, Subidar M, Alhadi H. Al Wakra emergency presentation of Behcet’s disease. AME Case Rep 2019;3:34.