
Ciliated muconodular papillary tumor of the lung presenting with polymyalgia rheumatica-like symptoms: a case report
Introduction
Ciliated muconodular papillary tumors (CMPTs) of the lung have been recently characterized as low-grade malignant tumors. It is difficult to distinguish CMPT from adenocarcinoma in situ (AIS) (1-3). Polymyalgia rheumatica (PMR)-like symptoms have been reported as paraneoplastic symptoms associated with lung cancer (4,5). CMPT is thought to be associated with benign tumors; however, we herein report a case of CMPT with PMR-like symptoms that resolved after resection, which was indistinguishable from AIS before pulmonary resection.
Case presentation
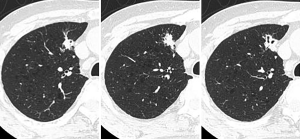
A 78-year-old man with a history of diabetes mellitus and hypertension had experienced bilateral pain and stiffness in his proximal thigh muscle, which occurred throughout the day, starting first thing in the morning; however, he was not hospitalized. He was referred to our hospital because of a lung tumor, which was identified on computed tomography (CT). Laboratory investigations showed a carcinoembryonic antigen level of 7.5 ng/mL and a C-reactive protein level of 0.4 mg/dL. CT indicated the presence of a lung nodule, 1.9 cm in diameter, with a cavity in the right S3 segment (Figure 1). The nodule had a standardized uptake value of 3.56 on 18F-fluorodeoxyglucose positron emission tomographic imaging. No other nodules were identified. Based on these findings, lung cancer was suspected. However, a diagnosis could not be made based on bronchoscopic biopsy findings, and, therefore, surgical biopsy was performed. After the patient’s health was assessed, thoracoscopic surgery was performed utilizing four ports to biopsy the tumor.
Intraoperative rapid diagnosis with a frozen section of the tumor indicated AIS; hence, we performed right upper lobectomy with lymph node dissection. After the surgery, we consulted another hospital, because histological examination of the resected specimen showed a low nuclear grade, and the tumor did not resemble AIS. The tumor consisted of a mixture of ciliated columnar, mucous, and basal cells in glandular and papillary growth patterns, and basal cells showed positive p40 staining. These features were consistent with those of CMPT; thus, the patient was diagnosed accordingly (Figure 2). After the surgery, his bilateral pain and stiffness in the proximal thigh muscle were relieved. Symptom relief was maintained despite reducing the dose of analgesics. We performed antinuclear antibody tests; however, no abnormality was noted. Thirty months after the surgery, the patient did not have any symptoms and had no tumor recurrence. Nonetheless, he is being monitored carefully because the etiology of the tumor is not understood clearly.

Discussion
This case demonstrates two key points: the paraneoplastic symptoms of CMPT can indicate PMR, and it is difficult to diagnose peripheral lung tumor cases as CMPT without obtaining a completely resected specimen.
The diagnosis of PMR is based on the Provisional Classification Criteria for Polymyalgia Rheumatica (Table 1) (6). The current patient had experienced bilateral pain and stiffness in his proximal thigh muscle, which started upon waking up every morning. Laboratory investigations just before the operation showed absence of anti-citrullinated protein antibodies and other antinuclear antibodies. Thus, it was revealed that he had PMR, because he met two criteria and his score was 4. However, after the surgery, his symptoms disappeared. He is being monitored carefully, and his symptoms have not returned.

Full table
Secondly, AIS is a precancerous lesion. Moreover, it is difficult to distinguish CMPT from AIS, because they are both abundant in the mucous cells and spread along the alveolar walls. In a previous study, the authors reported that they could judge that the tumor was a low-grade malignant tumor using frozen sections (7). However, we could not determine that the tumor was not AIS. After the surgery, we consulted with another hospital, and two more features were identified consistent with CMPT. First, there were no atypical cells. Second, there were mixed structures constructed with ciliated cells, mucous cells, and basal cells positive for p40. The differential diagnosis for CMPT and AIS may become easier with the accumulation of data from more cases; however, currently, it is difficult to investigate in detail without observing viable pathological specimens after the operation.
In summary, CMPT can present with paraneoplastic symptoms that indicate PMR; therefore, it is difficult to diagnose peripheral lung tumors as CMPT without obtaining a completely resected specimen. Hence, it is important to resect the tumor completely.
Acknowledgments
We would like to thank Editage (www.editage.jp) for English language editing.
Footnote
Conflicts of Interest: This paper was presented at the 57th Annual Meeting of the Japan Lung Cancer Society at Fukuoka on December 20, 2016.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of written consent is available for review by the Editor-in-Chief of this journal.
References
- Kamata T, Yoshida A, Kosuge T, et al. Ciliated muconodular papillary tumors of the lung: a clinicopathologic analysis of 10 cases. Am J Surg Pathol 2015;39:753-60. [Crossref] [PubMed]
- Miyai K, Takeo H, Nakayama T, et al. Invasive form of ciliated muconodular papillary tumor of the lung: A case report and review of the literature. Pathol Int 2018;68:530-5. [Crossref] [PubMed]
- Zheng Q, Luo R, Jin Y, et al. So-called "non-classic" ciliated muconodular papillary tumors: a comprehensive comparison of the clinicopathological and molecular features with classic ciliated muconodular papillary tumors. Hum Pathol 2018;82:193-201. [Crossref] [PubMed]
- Naschitz JE, Slobodin G, Yeshurun D, et al. A polymyalgia rheumatica-like syndrome as presentation of metastatic cancer. J Clin Rheumatol 1996;2:305-8. [Crossref] [PubMed]
- Hakkou J, Rostom S, Bahiri R, et al. Paraneoplastic rheumatic syndromes: report of eight cases and review of literature. Rheumatol Int 2012;32:1485-9. [Crossref] [PubMed]
- Dasgupta B, Cimmino MA, Kremers HM, et al. 2012 Provisional classification criteria for polymyalgia rheumatica: a European League Against Rheumatism/American College of Rheumatology collaborative initiative. Arthritis Rheum 2012;64:943-54. [Crossref] [PubMed]
- Sato S, Koike T, Homma K, et al. Ciliated muconodular papillary tumour of the lung: a newly defined low-grade malignant tumour. Interact Cardiovasc Thorac Surg 2010;11:685-7. [Crossref] [PubMed]
Cite this article as: Uchida T, Matsubara H, Ohnuki Y, Sugimura A, Matsuoka H, Ichihara T, Nakajima H. Ciliated muconodular papillary tumor of the lung presenting with polymyalgia rheumatica-like symptoms: a case report. AME Case Rep 2019;3:37.


