
Adult primary gastric volvulus, a report of two cases
Introduction
Gastric volvulus is the medical situation that a stomach is twisted beyond the physiological range. Gastric volvulus is classified into two types, organoaxial volvulus (long axis type) and mesenteroaxial volvulus (short axis type). And also, there is complex type in which long axis type mixes with short axis type (1,2). Furthermore, it is classified into primary and secondary from the viewpoint of cause. Most of the onsets in childhood are primary due to underdeveloped stomach and ligaments for gastric fixation. On the other hand, nearly two thirds of adult onset cases are secondary, which are induced by stomach lesions such as esophageal hiatus hernia, diaphragmatic laxity, gastric ulcer, gastric cancer and so forth (3,4).
Principally surgical treatment is essential for the acute type. However, the conservative therapy should be attempted if situations allow, such as decompression of a stomach by insertion of a nasogastric tube, endoscopic reduction and so forth.
Concerning surgical operation, the base is reduction of the torsion and immobilization of stomach. Generally laparotomy surgery has been performed. Recently, laparoscopic surgery is performed for the case that the general condition is stable or chronically progressive in the early stages of onset (5). During a certain period in the past, gastric fixation with percutaneous endoscopic gastrostomy (PEG) had been performed as a treatment method with less invasiveness (6).
In this paper, we present two cases on adult primary gastric volvulus. For the first case, endoscopic reduction was not good enough to release the torsion state completely. Then laparoscopic gastropexy was performed successfully. For the second case, we performed the laparoscopic gastropexy in a similar way to the first case. However, gastric volvulus recurred partially and then PEG was performed. The gastrostomies were removed 6 months after the surgery.
Case presentation
The first case
A 75-year-old woman presented to the emergency department with main complaints of vomiting and abdominal distension since the previous day. She did not have significant medical history. The patient was conscious and oriented and had a pulse of 110 beats per minutes, a blood pressure of 120/78 mmHg, a body temperature of 37.2 °C and an oxygen saturation 98% on room air. Physical examination revealed abdominal distension with slight epigastric tenderness. Laboratory testing revealed as follows, white blood cell count: 22,000/mL (normal, 4,000–9,000/mL), serum C-reactive protein concentration: 10.7 mg/dL (normal, <0.3 mg/dL).
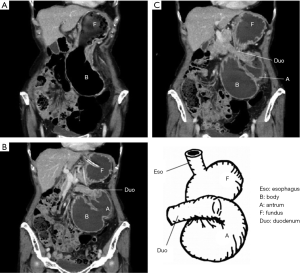
Figure 1 shows the contrast-enhanced computed tomography (CT) findings, radiogram of the abdomen. The schematic diagram of stomach drawn based on the findings is also shown in Figure 1. CT image of Figure 1A confirms for the stomach to be markedly distended and filled with gas and fluid. And it also confirms that the gastric antrum was displaced so as to overlap with gastroesophageal junction. In the image of Figure 1C, gastrointestinal (GI) endoscope is inserted to duodenal bulb. The tube of the endoscope is bended so as to make a spiral. It does not conflict with the CT images but rather supports them. CT image of Figure 1B demonstrates that the spleen is close to the fundus of the stomach and the positions of the spleen and duodenum are definitely shifted to right side. It is itself normal that the spleen is close to the fundus of the stomach. However, it is abnormal that both of the spleen and the fundus of the stomach are far away from the left diaphragm.
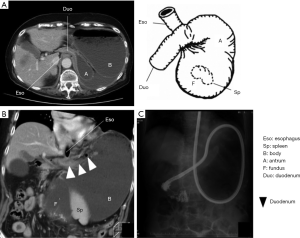
We diagnosed mesenteroaxial gastric volvulus. A nasogastric tube was placed, draining immediately 1,700 mL of gastric fluid. It was food residue and no apparent blood contamination was observed. After correcting dehydration, an upper GI endoscopy was performed on the third day after the hospitalization. It showed extensive ulcers and erosions in a wide region from the cardia to the middle of the stomach. When the tip of GI endoscope was progressed beyond the stenosis and arrived at duodenal bulb, the torsion was once released radiographically. However, the torsion state reoccurred just after the GI endoscope was withdrawn.
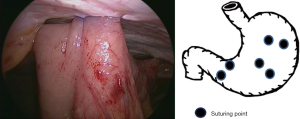
Laparoscopic gastropexy was performed under general anesthesia. A 12-mm port was inserted at the umbilicus and four 5-mm ports were placed around there. The omentum was shifted to the upper side and was twisted.
Immobility of organs under the left diaphragm was poor compared to usual case and the spleen and the fundus were easy to move. The upper, middle gastric bodies and the gastric antrum were secured to the anterior abdominal wall with two interrupted absorbable sutures as shown in Figure 2.
The postoperative period was uneventful. The patient was discharged on 15th fifteenth day postoperatively and presented no complaints one and a half years after the surgery.
The second case
A 67-year-old woman presented to the emergency department with a 7-day history of abdominal distention and epigastric pain. She had experienced similar symptoms and had been diagnosed with gastric volvulus 3 years ago. Her other medical history was unremarkable. The patient was conscious and oriented and had a pulse of 58 beats per minutes, a blood pressure of 127/92 mmHg, a body temperature of 36.3 °C, and an oxygen saturation 94% on room air. Physical examination revealed abdominal distension with mild epigastric tenderness. Laboratory testing revealed as follows, white blood cell count: 11,400/mL (normal, 4,000–9,000/mL), serum C-reactive protein concentration: 0.05 mg/dL (normal, <0.3 mg/dL).
Figure 3 shows CT images and the schematic diagram of stomach drawn based on the findings. The stomach is grossly enlarged and filled with gas and fluid. The gastric antrum was displaced so as to overlap with gastroesophageal junction. Figure 3B demonstrates that position of the spleen and fundus are definitely shifted to inferior side. Figure 3C demonstrates that abdominal esophagus is abnormally close to duodenum and position of the spleen and fundus are definitely shifted to inferior side.
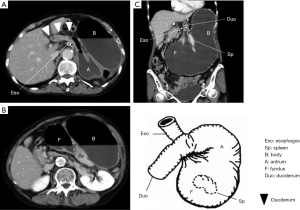
CT images of Figure 3B,C also demonstrates that the spleen is close to the fundus of the stomach. This configuration is itself normal. However, it is abnormal that both of the spleen and the fundus of the stomach are far away from the left diaphragm.
These situations are similar to 1st the first case. We diagnosed mesenteroaxial gastric volvulus.
Upper GI endoscopy also revealed the torsion of the stomach. Then we tried to release the torsion and succeeded in the detorsion of the stomach. GI endoscope passed through the pylorus and reached the duodenum. After this treatment, the symptoms of the patient improved and disappeared.
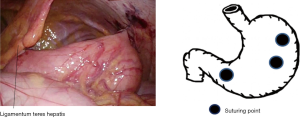
As the patient had already experienced gastric volvulus, laparoscopic gastropexy was performed under general anesthesia. A 12-mm port was inserted at the umbilicus and two 5-mm ports were placed at the both of left and right sides of lower abdomen. The stomach was in its normal anatomical position. However, it was found that the stomach was distended and peritoneal ligament was so loose. Immobility of organs under the left diaphragm was poor compared to usual case. And the spleen and the fundus were easy to move.
The upper and middle gastric bodies were secured to the anterior abdominal wall with absorbable sutures. And the gastric antrum was also secured to the ligamentum teres hepatis with interrupted absorbable sutures as shown in Figure 4. The postoperative period was uneventful. The patient was discharged on seventh postoperatively.
She presented to the emergency department again with abdominal distension 7 days after leaving the hospital. Figure 5 shows CT examination results. All of the images are coronal scan images and scan levels are as follows: ventral (Figure 5A), dorsal (Figure 5C) and intermediate between ventral and dorsal (Figure 5B). And it also shows the schematic diagram drawn based on the findings. CT images confirm that partial gastric volvulus occurs due to coming off of the suture at the antrum which had been secured to the ligamentum teres hepatis with interrupted absorbable sutures.
PEG for 2 points of lower body and antrum were performed to secure the antrum where the partial torsion occurred.
The postoperative period was uneventful and she was discharged on the 7th seventh post-operative day. The gastrostomies were removed 6 months after the surgery. She has presented no complaints two years after these series of treatment.
Discussion
Gastric volvulus was first reported by Berti, which was found during an autopsy in 1866 (7). It is caused by poor immobility of a stomach and working of some factor to induce the torsion on a stomach.
Gastric volvulus is classified into two types, organoaxial volvulus (long axis type) and mesenteroaxial volvulus (short axis type). The former is the type that stomach is twisted around the organoaxis connecting the cardia and pylorus. The latter is the type that stomach is twisted around mesenteroaxis connecting the greater curvature and the lesser curvature. And also, there is complex type in which long axis type mixes with short axis type. Furthermore, it is classified into primary and secondary from the viewpoint of cause. Most of cases in childhood are primary due to underdeveloped stomach and ligaments for gastric fixation. On the other hand, about two thirds of adult cases are secondary, which are caused by stomach lesions such as esophageal hiatus hernia, diaphragmatic laxity, gastric ulcer, gastric cancer and so forth.
Some papers show that mesenteroaxial volvulus is caused by wandering spleen (8). Wandering spleen is the state that spleen is excessively easy to move around. Wandering spleen is caused by the acquired factors such as weakening of the supporting ligament due to pregnancy or trauma, weakness in abdominal muscle and so forth.
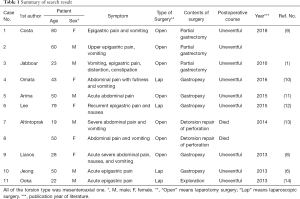
Gastric volvulus is a rare disease and is hardly experienced in routine medical examination. We searched the literature on adult and primary gastric volvulus reported from 2000 to 2018 using PubMed. Nine literatures were found and we could not find any paper or report before 2013 (1,6,8-14).
The search results are summarized in Table 1. All of the torsion type was mesenteroaxial and two of 11 cases are dead cases (cases No. of 7 and 8). Except for special case No. 11, surgeries were performed in all cases. For the case of No. 11, the twisted stomach was reduced by the insertion of nasogastric tube without surgery. Gastropexy is main surgery and partial gastrectomy is done in 3 cases. Laparoscopic surgery occupies nearly half of the cases.
Full table
Symptoms of chronic type gastric volvulus are light because the angle of torsion is usually less than 180 degrees and are often found incidentally. On the other hand, the angle of torsion is usually more than 180 degrees and symptoms are serious for acute type. Symptoms include Borchardt’s triad (strong epigastric pain, upper abdominal bloating, strong nausea without vomit and difficulty to pass through a nasogastric tube) (15). However, all symptoms do not always appear. As gastric volvulus is a rare disease, you might misdiagnose unless you distinguish carefully acute abdominal pain with keeping it in mind.
Principally surgical treatment is essential for the following acute cases, when gastric perforation or massive bleeding occur, when the mesenteroaxial volvulus causes cardia blockage and nasogastric tube and when endoscopes can not be inserted. On the other hand, the conservative therapy should be attempted if situations allow, such as decompression of a stomach by insertion of a nasogastric tube, endoscopic reduction and so forth. However, surgical treatment becomes also essential, when there is no improvement by conservative treatment or relapse is repeated (16,17).
Concerning surgical operation, the base is reduction of the torsion and immobilization of stomach. If necessary, the following treatments are also needed; treatments of complicated lesions such as necrosis, perforation and bleeding of the stomach. Furthermore, the treatment of the casual lesion (Cause Lesions) of torsion are also needed in some cases such as esophageal hiatus hernia and so forth.
Generally laparotomy surgery has been performed. In recent years, laparoscopic surgery is performed for the case when the general condition is stable or chronically progressive in the early stages of onset.
During a certain period in the past, gastric fixation with PEG was performed as a treatment method with less invasion. However, the recurrences and problems of twisting around the gastrostomy site were reported in addition to the problem of cosmetic outcomes. The number of cases of gastric fixation with PEG for adult is decreasing (18).
The problems on PEG mentioned before can be overcome by the fixation of multi-point with PEG and removal of gastrostomy after the surgery.
About our cases
We have experienced two cases of gastric volvulus. Neither of them showed a severe ischemia due to torsion and conservative treatments were initially attempted. For the first case, although the torsion was repaired by inserting the endoscope up to the duodenal bulb, the torsion occurred again just after the endoscope was withdrawn. Therefore, we decided to perform laparoscopic gastropexy to enable oral intake.
For the second case, we succeeded in repositioning the stomach endoscopically. The laparoscopic gastropexy was carried out, because the patient had medical history of gastric volvulus. However, the suture between the antrum and the ligamentum teres hepatis was pulled apart and partial torsion occurred again ten and a several days postoperatively. Considering the reduction of the patient’s burden, additional 2 points fixations of gastric antrum and lower body were done with PEG which has the characteristics of minimum invasiveness.
As a cause of the avulsion of the suture between the antrum and the ligamentum teres hepatis, the ligamentum teres hepatis might not be tough enough to hold the suture. The suture between the antrum and abdominal wall was tried once during the surgery but it failed due to the avulsion of the sutured part of the abdominal wall. In order to avoid such a kind of accident, it is important to perform enough amount of sutures so that the suture is hard to be pulled apart and the force applied to the suture is dispersed. If the space between the stomach and the abdominal wall is large, internal herniation might be induced. So, it should be considered to stitch the stomach to the abdominal wall as closely as possible.
As mentioned before, immobility of organs under the left diaphragm was poor compared to usual case and the spleen and the fundus were easy to move with keeping the normal configuration of spleen and fundus for our both cases. It most likely seems that the peritoneal ligaments except the gastrosplenic ligament are not firm enough to keep the stomach and the spleen at anatomical positions.
We can consider two possible causes of gastric volvulus for our cases. One is that the spleen is in the wandering state and the spleen pulls the fundus of the stomach through the gastrosplenic ligament to induce the torsion of stomach. Another is that some factor except spleen works on a stomach to induce torsion. Spleen is moved according to the deformation of stomach because it is connected to the fundus of stomach tightly through gastrosplenic ligament. Unfortunately, we do not have enough data to decide which actual cause for our cases is.
Laparoscopic surgery is useful and minimally invasive. However, it is difficult to secure a visual field unless the twisted and highly expanded stomach is decompressed. Therefore, first of all, the decompression of the expanded stomach is essential for laparoscopic surgery. Even though pressure reduction with the nasogastric tube is difficult, it can be sometimes done with endoscope. So, one should never abandon laparoscopic surgery even though it is hard to decompress the stomach with nasogastric tube. The important thing is that laparoscopic surgery does have the merit of minimum invasiveness.
The fixation by PEG has problems of cosmetic outcome. And also, the cases of recurrence and torsion around the gastrostomy have been reported. However, PEG has the significant merit of minimum invasiveness. The fixed gastrostomy can be removed after healing (19). The frequency of complications may decrease if multiple sites are fixed as in our case. Therefore it is definite that the fixation by PEG is useful as one of the options in some case.
In conclusion, laparoscopic gastropexy for gastric volvulus is useful when the patient’s condition is stable, since it has the significant merit of minimum invasiveness compared to laparotomy surgery. Especially, the number of sutures is very important, when stomach is secured to abdominal wall with gastropexy. Less sutures may make it easy for the secured part to be torn off.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Informed consent was obtained from the patients for publication and any accompanying images.
References
- Jabbour G, Afifi I, Ellabib M. Spontaneous acute mesenteroaxial gastric volvulus diagnosed by computed tomography scan in a young man. Am J Case Rep 2016;17:283-8. [Crossref] [PubMed]
- Akhtar A, Siddiqui FS, Sheikh AAE. Gastric volvulus: A Rare Entity Case Report and Literature Review. Cureus 2018;10:e2312. [PubMed]
- Smith RJ. Volvulus of the stomach. J Natl Med Assoc 1983;75:393. [PubMed]
- Sevcik WE, Steiner IP. Acute gastric volvulus: case report and review of the literature. CJEM 1999;1:200-3. [Crossref] [PubMed]
- Channer LT, Squires GT, Price PD. Laparoscopic Repair of Gastric Volvulus. JSLS 2000;4:225-30. [PubMed]
- Jeong SH, Ha CY, Lee YJ. Acute gastric volvulus treated with laparoscopic reduction and percutaneous endoscopic gastrostomy. J Korean Surg Soc 2013;85:47-50. [Crossref] [PubMed]
- Carter R, Brewer LA, Hinshaw DB. Acute gastric volvulus. A study of 25 cases. Am J Surg 1980;140:99-106. [Crossref] [PubMed]
- Lianos G, Vlachos K, Papakonstantinou N. Gastric volvulus and wandering spleen: a rare surgical emergency. Case Rep Surg 2013;2013:561752.
- Costa MRP, Matos ASB, Almeida JR. Primary gastric volvulus: a report of two cases. J Surg Case Rep 2018;2018:rjy227.
- Omata J, Utsunomiya K, Kajiwara Y. Acute gastric volvulus associated with wandering spleen in an adult treated laparoscopically after endoscopic reduction: a case report. Surg Case Rep 2016;2:47. [Crossref] [PubMed]
- Arima K, Hashimoto D, Takata N. Acute gastric volvulus in a patient with trisomy 21. Surg Case Rep 2015;1:5. [Crossref] [PubMed]
- Lee HY, Park JH, Kim SG. Chronic gastric volvulus with laparoscopic gastropexy after endoscopic reduction: a case report. J Gastric Cancer 2015;15:147-50. [Crossref] [PubMed]
- Altintoprak F, Yalkin O, Dikicier E. A rare etiology of acute abdominal syndrome in adults: gastric volvulus - cases series. Int J Surg Case Rep 2014;5:731-4. [Crossref] [PubMed]
- Ooka M, Kohda E, Iizuka Y. Wandering spleen with gastric volvulus and intestinal non-rotation in an adult male patient. Acta Radiol Short Rep 2013;2:2047981613499755. [Crossref] [PubMed]
- Borchardt M. Zur Pathologie und Therapie des Magenvolvulus. Arch Klin Chir 1904;74:243-8.
- Morelli U, Bravetti M, Ronca P, et al. Laparoscopic anterior gastropexy for chronic recurrent gastric volvulus: a case report. J Med Case Rep 2008;2:244. [Crossref] [PubMed]
- Laurent S, Grayet D, Lavigne CM. Acute and chronic gastric volvulus: a radical different prognosis and management. Case report. Acta Chir Belg 2010;110:76-9. [Crossref] [PubMed]
- Eckhauser ML, Ferron JP. The use of dual percutaneous endoscopic gastrostomy (DPEG) in the management of chronic intermittent gastric volvulus. Gastrointest Endosc 1985;31:340-2. [Crossref] [PubMed]
- Joshi MA, Dewoolkar V, Subramanyan P, et al. Treatment of Chronic Gastric Volvulus by Percutaneous Endoscopic Gastrostomy. Digestive Endoscopy 1998;10:327-30. [Crossref] [PubMed]
Cite this article as: Miura Y, Otsuka R, Arita A, Ishida Y. Adult primary gastric volvulus, a report of two cases. AME Case Rep 2019;3:43.


