
Endoscopic decompression of epidural spinal metastasis causing lumbar radiculopathy through a transforaminal approach: report of two cases
Introduction
Improving therapies have led to increased survival rates for a variety of cancer types, however this has led to greater incidence of metastatic spine disease (MSD) (1). Up to 40% of these patients will have involvement of the vertebral column, leading to pain and loss of neurologic function (2-4). Radiculopathy in patients with epidural MSD may be palliated with open or microsurgical techniques though delay of chemoradiation, infection risk, extended hospitalization periods, and surgical site pain may complicate surgical efforts to improve these patients’ lives.
Endoscopic approaches, heretofore used almost exclusively in degenerative spine disease, may also palliate debilitating pain while mitigating the drawbacks of surgical intervention in providing focal tumor debulking. Specimen for pathology, which is of increasing importance in oncology treatments, may also be obtained by the endoscopic approach.
Case presentation
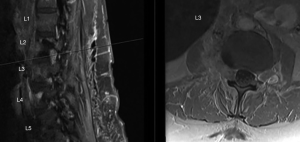
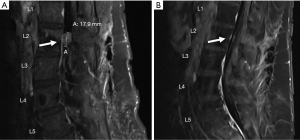
Patient A, a 61-year-old woman with right thigh pain and weakness, presented for neurosurgical evaluation with history notable for metastatic adenocarcinoma of unknown primary, in the setting of a remote history of ovarian tumor for which she had undergone total abdominal hysterectomy with bilateral salpingo-oophorectomy and omentectomy 26 years prior. Metastases to the neck and chest were more recently treated with surgery and chemoradiation. Her exam showed right quadriceps strength 4/5 and decreased sensation over the right anterior thigh. Reflexes were absent and there was no sphincter dysfunction. Contrasted magnetic resonance imaging (MRI) of the lumbar spine confirmed retroperitoneal mass with infiltration of the right psoas muscle. The soft tissue mass extended into the right neuroforamen at the L2−L3 level encasing the exiting L2 nerve root, effacing the right aspect of the spinal canal and abutting the cauda equina nerve roots (Figure 1). The intra-foraminal mass was determined to be the most symptomatic causing anterior thigh pain and weakness. The psoas retroperitoneal component, as well as the intra-dural components, were judged to be asymptomatic. These findings were discussed with the patient who consented to undergo an endoscopic approach with the understanding that this would not preclude the possibility of future open laminectomy and intradural exploration to excise the foraminal and intradural mass. Patient B, informed consent was provided by both patients for participation in this report and the documentation of these cases met the criteria for exemption from the institutional review board. Postoperative radiation therapy was also planned to address the bony component as well as residual micro and likely macro-disease.
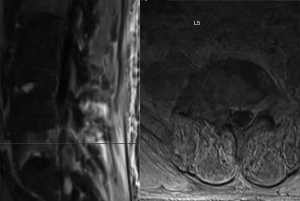
Patient B, a 50-year-old man with history of urothelial cell carcinoma and emphysema presented to our clinic for evaluation of right leg and low back pain. He had undergone radical nephroureterectomy 9 months prior. Subsequently, osseous metastases were confirmed and radiation was administered to the lumbosacral spine and pelvis, finishing 8 months prior to our procedure. In the intervening time he had undergone four cycles of cisplatin/gemcitabine stopped due to osseous progression. Pembrolizumab was initiated but halted for autoimmune pneumonitis, complicating his suitability for general endotracheal anesthesia. His examination revealed dermatomal pain in the L5 distribution without associated weakness. MRI confirmed MSD compressing the right L5 exiting nerve root at the L5-S1 interspace, as well as compression fractures of L4 and L5 with loss of vertebral body height (Figure 2). Vertebroplasty was performed at L4 and L5 concurrently in the standard fashion, which is not described further in this report.
Technique
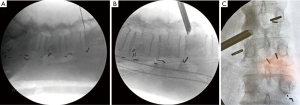
The patients were positioned prone as for standard lumbar decompression, the first under general endotracheal anesthesia and the second under monitored anesthesia care (MAC). Electromyographic (EMG) neuromonitoring was employed in each case. Using a transforaminal approach, serial dilation was performed into the foramina between L2 and L3 for the first case, and between L5 and S1 for the second case (Figure 3). Crown reamer was used to perform a superior facetectomy. A dock was then placed and an endoscope was inserted, which brought into view the traversing nerve root and epidural mass. A 15-gauge Myriad side-cutting aspiration device (NICO, Indianapolis, IN, USA) with a length of 26.5 cm was used through the endoscope to assist with tumor resection. The exiting root was clean from tumor extending superiorly towards the axilla. In the first case, there was noted to be a hole where it appeared that there was intradural extension. This portion could not be delivered as it was densely adherent to the rootlets internally. In both cases, the exiting and traversing nerve roots were decompressed under direct visualization and hemostasis was obtained. Depo-Medrol was left behind, and the port was removed. Incisions were closed using Vicryl sutures and surgical glue on the skin. Pathology was consistent with adenocarcinoma and urothelial carcinoma respectively.
EMG monitoring was conducted in each patient to detect and alert the surgeon to specific nerve root irritation. Paired, subdermal needle electrodes (13 mm length and 0.4 mm diameter) were placed bilaterally in the adductor magnus, quadriceps, tibialis anterior, gastrocnemius, and abductor hallucis muscles. An impedance of less than 5 KΏ was maintained in all electrodes throughout the procedure. Baseline EMG traces were obtained after intubation and prior to incision. The surgeon was notified of baseline EMG data and if any pre-existing nerve root injury was present. The surgeon was notified and acknowledged any significant changes to the baseline data, especially sustained bursts and A-train firing activity. Cadwell (Kennewick, WA, USA) machines were used to record and store all case data files.
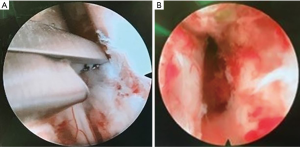
Intraoperative visualization
Anatomical entry sites were consistent with those described previously in the literature for herniated lumbar discs (5). Bleeding did not obscure the surgical field and several techniques were utilized to maintain good visibility (Figure 4). Irrigant flow was augmented as necessary. The bipolar probe is effective for hemostasis so long as visualization is maintained. Irrigant pressure can be increased by feathering closed the outflow with a finger and increasing the counterpressure to help with hemostasis. Hemostatic matrix of gelatin and thrombin may be inserted directly through the chamber as a further measure.
Postoperative course
Both patients received biopsy-proven results. The first had complete pain relief and resolution of weakness. One year post-operative MRI confirmed durable epidural decompression (Figure 5). The second patient appreciated stabilization of pain but not complete relief. He transitioned to comfort measures only when his systemic disease progressed 3 months later, precluding follow-up MRI. Neither patient experienced any surgical complication. Both were observed inpatient overnight out of an abundance of caution.
Discussion
MSD offers a unique opportunity to implement adaptations of current technology, originally designed for degenerative indications. Ultimately, the objectives of metastatic disease management are focused on the preservation of neurologic function and stability while achieving palliation. Here we report our novel experience of a working channel endoscope used exclusively and successfully for biopsy and decompression of a lumbar metastasis compressing the exiting spinal nerve root.
The use of endoscope and specially-designed instruments, introduced through a beveled cannula between the traversing and exiting nerves in an area known as Kambin’s Triangle is well-described (5). With the epidural space well-visualized, a multi-channel flow-integrated endoscope may provide high quality imaging. Newer approaches have emerged incorporating the use of the endoscope in treating MSD. Ravindra et al. described a thoracoscopic-assisted approach at the thoracolumbar junction with significant improvement in pain scores and no loss of neurologic function (2). A case of thoracic radiculopathy treated by endoscopic decompression has been reported (6). More recently a case of ventral thoracic epidural metastasis was resected through a single port endoscopic approach with excellent radiographic improvement (7). The transforaminal approach, which has been well described in applications for decompression of synovial cysts, has been extended recently in a report detailing the decompression of a lumbar epidural hematoma (8).
One potential concern from this approach is perceived risk of increased difficulty in controlling bleeding. Using simple techniques, we avoided any hemorrhagic complications. In the absence of further experience with the techniques, tumors that notoriously bleed such as renal cell may be less ideal candidates. Additionally, the endoscopic approach possesses a learning curve, however this should not dissuade from its implementation in MSD.
Undoubtedly, patients with MSD present with many different syndromes. We believe these two cases illustrate a super-select subset of metastasis radiculopathy, and we report a new application of existing technology to augment the neurosurgical armamentarium. This approach represents a feasible diagnostic and treatment option for those with discrete radicular complaints and does not preclude future, more invasive options, and may indeed afford speedy convalescence towards further chemoradiation therapy.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patients and/or medical power of attorney for publication of this Case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Bhatt AD, Schuler JC, Boakye M, et al. Current and emerging concepts in non-invasive and minimally invasive management of spine metastasis. Cancer Treat Rev 2013;39:142-52. [Crossref] [PubMed]
- Ravindra VM, Brock A, Awad AW, et al. The role of the mini-open thoracoscopic-assisted approach in the management of metastatic spine disease at the thoracolumbar junction. Neurosurg Focus 2016;41:E16. [Crossref] [PubMed]
- Petteys RJ, Sciubba DM, Gokaslan ZL. Surgical management of metastatic spine disease. Semin Spine Surg 2009;21:86-92. [Crossref]
- Byrne TN. Spinal cord compression from epidural metastases. N Engl J Med 1992;327:614-9. [Crossref] [PubMed]
- Gibson JN, Cowie JG, Iprenburg M. Transforaminal endoscopic spinal surgery: the future 'gold standard' for discectomy? - A review. Surgeon 2012;10:290-6. [Crossref] [PubMed]
- Joo YC, Ok WK, Baik SH, et al. Removal of a vertebral metastatic tumor compressing the spinal nerve roots via a single-port, transforaminal, endoscopic approach under monitored anesthesia care. Pain Physician 2012;15:297-302. [PubMed]
- Telfeian AE, Choi DB, Aghion DM. Transforaminal endoscopic surgery under local analgesia for ventral epidural thoracic spinal tumor: Case report. Clin Neurol Neurosurg 2015;134:1-3. [Crossref] [PubMed]
- Wu ZY, Zhu YJ, Chu L, et al. Full-Endoscopic Transforaminal Approach for Removal of a Spontaneous Spinal Epidural Hematoma. World Neurosurg 2017;98:883.e13-20. [Crossref] [PubMed]
Cite this article as: Henderson F Jr, Hubbard ZS, Jones S, Barley J, Frankel B. Endoscopic decompression of epidural spinal metastasis causing lumbar radiculopathy through a transforaminal approach: report of two cases. AME Case Rep 2020;4:2.


