
Treatment of male genital lymphedema with non-elastic fabric
Introduction
Lymphedema is a specific type of edema stemming from a failure in the formation or drainage of lymph. This condition can be congenital or acquired. In congenital cases, the individual is born with an abnormal lymphatic system that may or may not lead to the development of lymphedema throughout the course of his/her life. In secondary cases, the individual is born with the lymphatic system intact, but this system is damaged at some point in life, which can lead to lymphatic insufficiency and the development of edema (1,2).
Regarding genital lymphedema, a review study shows that there is no consensus on either the preoperative evaluation or surgical treatment. Patients who received excisional procedures were cases of late-stage lymphedema. Patients in the group submitted to excision and reconstruction of the flap seem to have greater complication rates (3,4).
The clinical treatment of genital lymphedema involves compression mechanisms of the penis and scrotum. Recently, the grosgrain was considered an appropriate material for penial compression (5). This non-elastic fabric is used to envelope the penis and is held in place with Velcro, enabling therapeutic pressure that leads to the reduction in penile edema (6,7). The aim of the present study is to report a case series involving this type of therapy for the treatment of male genital lymphedema. We present the following case series in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/acr-20-71) (8).
Case presentation
Thirteen consecutive patients with penoscrotal lymphedema aged 22 to 56 years (mean: 42.3 years) were treated at the Godoy Clinic. Inclusion criteria were patients with primary and secondary penoscrotal lymphedema. Volume larger than three times the normal size of the scrotum was excluded.
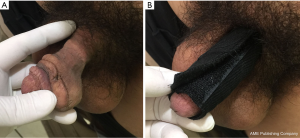
All patients with penile lymphedema were evaluated clinically and those with the volume no larger than three times the normal scrotum size (subjective assessment) were considered for clinical treatment. Grosgrain fabric was used with a size that could envelope the penis and fixed with Velcro (Figure 1). The patients or wives were trained to place the bandage, whereas the grosgrain wrap was placed and removed by the patient as necessary. They were followed up at every three, six or 12 months, depending on each patient's possibility of returning to the clinic. The patients were told that the proper use of the material would lead to the reduction in edema and the normalization or near normalization of the penis. The placement of the penis wrap is easier and can be done quickly and easily.
Reductions in edema occurred in the penis in all patients. Such reductions varied in accordance with the adherence of the patients to the use and duration of compression. The patients used the compression device at times that best fit their schedules. An interesting aspect was the fact that the patients reported the possibility of leaving the penis the size they wished—neither very small nor very large—for sexual activity. All were able to control the size of the edema within the standards they considered acceptable. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Discussion
The present study offers a therapeutic option for penile lymphedema in which the patient is trained to place a compression mechanism. The non-elastic material for the penis is grosgrain, which is attached with Velcro to enable the adjustment to the proper pressure. This grosgrain wrap is easily placed and removed and the result depends on the duration of the compression as well as the size of the edema. With this device, patients can have sexual activity without difficulty.
The grosgrain wrap must be adjusted as the penis reduces in size due to the reduction in the edema. The adjustments are made by a seamstress. This aspect is fundamental for the continuous reduction in edema until reading standards of normality or near normality. The patient must be made aware of the need for these adjustments. In practice, we have seen patients become upset because the wrap was loose and frequently slipped off. When the patient learns to place the compression mechanism properly, he has control over the edema and the freedom to wear the wrap whenever he deems it necessary. Thus, there is a degree of flexibility in the treatment depending on need.
Patients who see the positive results and understand the control they have over the size of the edema end up adhering well to treatment. At the beginning of the process, it is necessary to make the patient aware that lymphedema has no cure and treatment must continue for the rest of his life. The assistance and encouragement of the spouse is another important factor. This interaction of the couple is a decisive factor to adherence to treatment. Therefore, the psychological and sexual aspects of treatment need to be discussed along with the physical control of the edema. The grosgrain fabric should have a specific characteristic so that it can be adapted to the treatment of penile lymphedema (9).
Grosgrain fabric adapted as a penile wrap combined with a bandage for the treatment of penile lymphedema enables transferring an effective form of edema reduction to the patient and the maintenance of the results.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/acr-20-71
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/acr-20-71). FNF Jr serves as an unpaid Urology Section Head of ACR Case Report and LCFS serves as unpaid Urology Editor from June/2018. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Keo HH, Gretener SB, Staub D. Clinical and diagnostic aspects of lymphedema. Vasa 2017;46:255-61. [Crossref] [PubMed]
- Lee BB, Antignani PL, Baroncelli TA, et al. Iua-Isvi consensus for diagnosis guideline of chronic lymphedema of the limbs. Int Angiol 2015;34:311-32. [PubMed]
- Guiotto M, Bramhall RJ, Campisi C, et al. A systematic review of outcomes after genital lymphedema surgery: microsurgical reconstruction versus excisional procedures. Ann Plast Surg 2019;83:e85-91. [Crossref] [PubMed]
- Kanth AM, Krevalin M, Adetayo OA, et al. Surgical management of pediatric lymphedema: a systematic review. J Reconstr Microsurg 2019;35:462-70. [Crossref] [PubMed]
- de Godoy JM, Facio FN Jr, de Carvalho EC, et al. New compression mechanism in penile-scrotal lymphedema and sexual rehabilitation. Urol Ann 2014;6:88-90. [Crossref] [PubMed]
- Pereira de Godoy JM, de Fatima Guerreiro Godoy M, Spessoto LC, et al. Penile and sexual rehabilitation in a patient with lymphedema of the penis. Urol Int 2013;91:121-3. [Crossref] [PubMed]
- Facio MF, Spessoto LC, Gatti M, et al. clinical treatment of penile fibrosis after penoscrotal lymphedema. Urol Case Rep 2017;11:14-6. [Crossref] [PubMed]
- Riley DS, Barber MS, Kienle GS, et al. CARE 2013 Explanations and Elaborations: Reporting Guidelines for Case Reports. J Clin Epidemiol 2017;89:218-35. [Crossref] [PubMed]
- Godoy JMP, Godoy ACP, Godoy MFG. Godoy & Godoy compression sleeve in the treatment of arm lymphedema: new concepts for materials. Braz Arch Biol Technol 2015;58:864-8. [Crossref]
Cite this article as: Godoy JMP, Godoy MF, Facio MFW, Arruda GJF, Spessoto ACN, Spessoto LCF, Facio FN Jr. Treatment of male genital lymphedema with non-elastic fabric. AME Case Rep 2020;4:29.


