Major acetabular prosthetic protrusion following total hip arthroplasty: a case report of a reconstruction challenge
Introduction
Acetabular protrusion is an acetabular defect caused by the shift of the femoral head through the pelvic bone. On anterior-posterior (AP) view radiograph, we can observe the femoral head lying medially to the ilioischial Köhler’s line (1). This condition is more likely to appear 8 years after total hip arthroplasty (THA) implantation (2). The inadequate medial wall found in acetabular protrusion can cause major difficulties in performing THA. Because of bone loss, usual anatomical landmarks may be confusing or absent, leading to a particularly challenging surgical reconstruction in case of THA implantation, without adequate support of the acetabulum. In the presence of previous hip prosthesis requiring revision, additional difficulties appear regarding expected prosthetic function and joint stability. However, some authors described reconstruction methods such as, for example, Ganz reinforcement ring (3) and modular reconstruction stem femoral prosthesis (4) for overcoming these issues. Additional techniques exist like the use of bone graft (5), of cemented acetabular components, or the acetabuloplasty (6).
To our knowledge, no article has dealt with acetabular defects to this extent and associated femoral osteolysis. Thus, we hereby describe the case of a major acetabular defect following osteolysis of a multiple-revised THA which could be an interesting, reasonable and applicable alternative in order to propose a solution to such a surgical challenge. We present the following case in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-22-1/rc).
Case presentation
Anamnesis
A 77-year-old patient presented himself to the emergency department of our local hospital because of a left hip pain which occurred 3 days ago, not related to a trauma. He reported pain after standing up from the toilet seat, without any fall. Then, he described a persistent hip pain with functional impairment, and the need to sleep in a sitting position to relieve the worsening pain.
Ethical statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
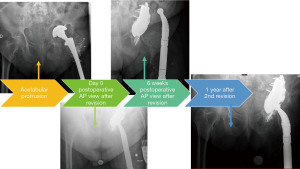
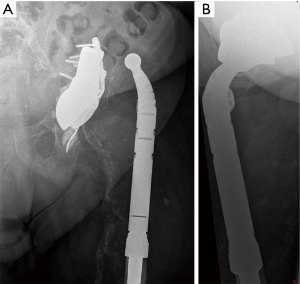
Medical history (Figure 1)

In the medical history of the patient, were relevant: a severe obesity, an ischemic cardiomyopathy with a status post-stenting, an atrial fibrillation treated by acenocoumarol, diabetes mellitus, a high blood pressure and a dyslipidemia. His left primary THA was performed in 1973 after a traffic accident, with a cup revision in 1994 at the age of 54. He underwent an osteosynthesis by cerclage wiring of the femoral stem because of a periprosthetic fracture Vancouver type B1 secondary to a fall from his height in 2015.
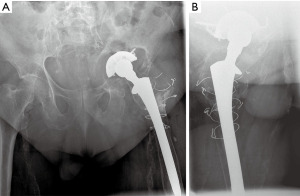
Clinical and radiological findings (Figure 2)
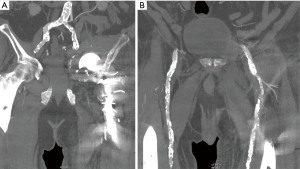
The clinical assessment showed left groin and thigh pain while palpation and passive delicate mobilization. He could not walk but had no other grievance. There was no vascular or nervous injury, and the skin was in order. We performed an AP radiograph of the pelvic ring and an axial incidence of the left hip. We discovered a substantial prosthesis protrusion through a major pelvic discontinuity (Figure 3). We classified its pattern as a type IIIB for the acetabulum according to the Paprosky classification, and a type IV for the femur (7,8). Additionally, we carried out an injected computed tomography (CT)-scan which showed no vascular injury (Figure 4).
Procedure
The patient was hospitalized in the orthopaedic surgery department of our local hospital for observation and analgesia. The pain was well controlled, and a thromboprophylaxis was administered, because of impossible weight-bearing, with subcutaneous enoxaparin 0.40 mL per day. We transferred him to the university hospital for definitive operative management.
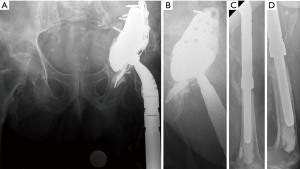
Surgical technique
The patient was under general anaesthesia on a right lateral position. Cefuroxim 1.5 g intravenous was used for antibiotic prophylaxis, and repeated half after 3 hours. A postero-lateral approach of the left hip prolonged distally was performed, with additional opening of the fascia lata. Arthrotomy revealed a major granuloma with wear debris and infiltration of soft tissue around the prosthesis. Samples were taken for microbiological analysis. Exploration confirmed intrapelvic migration of the acetabular components and major osteolysis of the proximal femur, also absence of the medial wall of the acetabulum, its anterior and posterior columns. The proximal femur was resected on 20 cm length of bone. Material removed from the femur and also the acetabular components were sent to sonication. The granuloma was thoroughly debridated, local haemostasis control and wash out were performed. An acetabular reconstruction augment was anchored to the iliac bone with 5 titanium screws. Above it, a titanium revision shell cup (TMARS revision cup, diameter 68 mm, uncemented, TMT/Zimmer Biomet, Warsaw, IN, USA), anchored by 3 anterosuperior screws, and oriented with 15° of anteversion and 45° of inclination. A little amount of cement was applied on its surface. A Burch Schneider armor (TMARS armor, long flange, left, 66/68/70 mm/Zimmer Biomet, Warsaw, IN, USA) was placed within. The armor was cemented on the ischium, and locked by 4 cortex screws on the ilium. Finally, a cemented acetabular cup (Symbol cup DM CEM 22.2 mm, size 48, UHMW/Dedienne Santé, Mauguio, France), diameter of 48 mm, was placed above, with 20° of anteversion and 45° of inclination. For the femur, abundant wash out and reaming from 9 to 13 mm were performed. A cemented modular proximal femoral resection stem (Zimmer Segmental System ZSS/Zimmer Biomet, Warsaw, IN, USA) was cemented until the femoral condyles, with a tantalum collar. Proximally a 15 cm stem, and above a modular neck with 38 mm of offset were placed. Temporary reduction showed adequate stability, allowing implantation of a metal head diameter 22.2 mm (Protasul-S30, modular head, 22 mm, M/Zimmer Biomet, Warsaw, IN, USA) with a neck 12/14 average, with an ultra-high molecular weight polyethylene (UHMWPE) insert 48/22.2 (Symbol insert, 22.2 mm, 0°, 48 mm, PE/Dedienne Santé, Mauguio, France). Mobility and stability controls were satisfactory. Wash out, haemostasis control and final closure were performed, with 3 drains.
Follow-up
Postoperative radiographs were satisfactory (Figure 5). In postoperative follow-up, the patient developed a right basal pneumonia caused by Moraxella catarrhalis treated by levofloxacin 500 mg during 1 week, with complete healing. The patient had a satisfying recovery and was authorized to come back to our orthopedic surgery department. All bacteriological samples such as implant sonication and granuloma biopsy remained negative after 10 days. He presented an uneventful evolution, without wound issue (Figure 6), and with good progression on physiotherapy. Then he could leave our department in the direction of a musculoskeletal rehabilitation center.
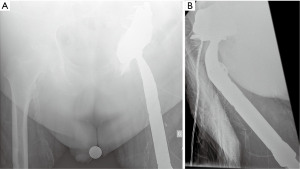

After 6 weeks postoperatively, the patient described pain on his left hip after sitting on a chair, with external rotation and shortening at clinical assessment. Radiographs confirmed a prosthesis dislocation (Figure 7), which was reduced under general anaesthesia. The patient was treated by analgesics and was sent to his surgeon at the university hospital consultation. At the clinical examination, the left hip showed an irreducible chronic dislocation. A revision was then scheduled.
Surgical technique of the revision
The revision surgery was performed under spinal anaesthesia on a right lateral position. Fascia lata was opened and arthrotomy released hematic fluid and a postero-lateral mobility chamber. Fluids were sampled for systematic microbiological analysis. Attempts of prosthesis reposition showed persistent instability. The femoral head was removed and sent to sonication for microbiological studies. Femoral anteversion was controlled and appeared adequate, measured to 15°. Unipolar revision of the acetabulum was then performed, after removal of the previous cup and cement, and sending them to sonication. Wash out. A 48 mm diameter constraint UHMWPE acetabular cup (Groupe Lépine, Genay, France) was cemented and placed with 25° of anteversion and 45° of inclination. A chrome-cobalt 22.2 mm head with a short neck −2 mm (Zimmer Biomet, Warsaw, IN, USA) was implanted. Manual reduction was performed and the hip showed adequate stability. Closure was performed as usual, after a wash out and with a single drain for 48 hours.
Final follow-up
Samples were negative for infection and the patient was transferred again to our orthopaedic surgery department before the rehabilitation centre. Finally, after 1 year, the evolution of the patient was uneventful without recurrence of instability and no need for reoperation. Radiographs were satisfactory (Figure 8), we can notice adequate appearance of the THA and no sign of osteolysis or dislocation. Pain was relieved and he could walk with the help of a rolling walker.
Patient perspective
I felt anxious regarding my current condition with the prosthesis issues. The surgical team at the hospital helped me to prepare myself for the surgery, and was nice to me for my healing process postoperatively. I was in the rehabilitation center after few days at the hospital, and felt confident for progression on my mobility and success of the operation.
Discussion
Acetabular protrusion, as a rare complication in patients with total hip replacement, is often the result of high-velocity accidents (9) and occurs mostly in patients who had a THA in their youth, as in the current case (10). Indeed, mechanical constraints in active patients, obesity, revisions, wear of material, bone lysis of the acetabulum, sepsis, rheumatoid arthritis (11) are the main causes of this complication (9,12).
Initial work-up should include 3-dimensional imaging to assess the bone stock, and infection must also be ruled out. Subsequently, the surgical challenge is based on the technique used to obtain satisfactory support for the acetabular prosthesis (13) and on the management of the abductor apparatus (14).
To achieve adequate stability, a THA requires a well-oriented acetabular cup (15), within a sufficient femoral offset (16) and femoral anteversion and finally a competent abductor apparatus (17).
In the current case, following the surgical revisions, initially the abductor apparatus was damaged, due to the repeated posterior approaches. In a second phase, with the progressive alteration of the bone stock following implant changes, the restoration of the initial anatomy became a real challenge. In particular with the absence of the usual landmarks for the positioning of the cup, the restoration of the initial offset became almost impossible. This is why we opted, after having made sure to restore the initial biomechanics as well as possible, for a constraint ring and a dual-mobility head.
Once the infection had been ruled out, and given the poor bone stock of the acetabulum, which did not allow satisfactory support of a regular prosthetic acetabulum, we had to opt for an acetabular augment in which we cemented our metal back. Besides, since he had initial THA, he underwent two revision surgeries (in 1994 and 2015), the trochanter mass as well as the abductor apparatus were non-existent, this is why a reconstruction femoral stem was our choice. Once the stage of the intraoperative infection had been passed, among other things the possible complications of decubitus (type thrombosis, pneumopathy of decubitus) with an abductor apparatus not efficient enough, the first complication to be feared was the dislocation. This happened in our patient at 6 weeks postoperatively when he was sitting on a chair. A reoperation was necessary to increase the tension in the total hip prosthesis. The use of a constraint acetabular cup (18) with slightly higher anteversion also helped to increase the stability of the prosthesis (19).
Other authors published about acetabular reconstruction in case of major pelvic discontinuity. Jeong et al. reported good clinical results at a 2-year follow-up of patients operated with a tantalum augment for Paprosky III and IV acetabular defects mainly (87%) related to aseptic cup loosening of THA (20). The authors used similar technique as described in the current case for acetabular reconstruction, and also for 5 patients with a revision femoral stem in case of femoral osteolysis as well. However, the authors did not find any postoperative dislocation as the abductor apparatus seemed to be intact in all cases. To solve this issue, Shapiro et al. (18) and Hernigou et al. (19) advocate the use of retentive cup, which appeared to be effective in the current case by increasing the stability of the revision THA.
The limitations of this case report are first, the lack of epidemiological quantities, indeed not being chosen from a representative population sample does not allow us to generate information on rates, or incidence of this pathology. Second, generalization is not possible. In order to generalize we need both cause-effect relationship and a representative population. Finally, the surgery was carried out by one of our senior surgeons who was being a success in his hands after several times but was not necessarily reproducible in the hands of everyone and an important learning curve seems to us essential before being able to launch out in a surgery so demanding.
Thus, although acetabular protrusion is a rare complication in total hip replacement patients and despite the limitations of this case report, we would like to draw attention to the challenging nature of this complication, both in terms of initial assessment and surgical management. The described strategy showed effective function of the reconstructed hip joint and final adequate stability of the prosthesis despite the absence of a competent abductor apparatus.
Acknowledgments
The authors would like to thank Prof. Olivier Guyen for his involvement in the patient’s surgical treatment.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-22-1/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-22-1/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-22-1/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zuh SG, Zazgyva A, Gergely I, et al. Acetabuloplasty with bone grafting in uncemented hip replacement for protrusion. Int Orthop 2015;39:1757-63. [Crossref] [PubMed]
- Apel DM, Smith DG, Schwartz CM, et al. Threaded cup acetabuloplasty. Early clinical experience. Clin Orthop Relat Res 1989;183-9. [PubMed]
- Gerber A, Pisan M, Zurakowski D, et al. Ganz reinforcement ring for reconstruction of acetabular defects in revision total hip arthroplasty. J Bone Joint Surg Am 2003;85:2358-64. [Crossref] [PubMed]
- Mumme T, Müller-Rath R, Andereya S, et al. Uncemented femoral revision arthroplasty using the modular revision prosthesis MRP-TITAN revision stem. Oper Orthop Traumatol 2007;19:56-77. [Crossref] [PubMed]
- Kinzinger PJ, Karthaus RP, Slooff TJ. Bone grafting for acetabular protrusion in hip arthroplasty. 27 cases of rheumatoid arthritis followed for 2-8 years. Acta Orthop Scand 1991;62:110-2. [Crossref] [PubMed]
- Dearborn JT, Harris WH. Acetabular revision after failed total hip arthroplasty in patients with congenital hip dislocation and dysplasia. Results after a mean of 8.6 years. J Bone Joint Surg Am 2000;82:1146-53. [Crossref] [PubMed]
- Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplasty 1994;9:33-44. [Crossref] [PubMed]
- Paprosky WG, Bradford MS, Younger TI. Classification of bone defects in failed prostheses. Chir Organi Mov 1994;79:285-91. [PubMed]
- Weber W, Moore J, Cheema N. Traumatic Acetabular Protrusion. Clin Pract Cases Emerg Med 2018;2:260-1. [Crossref] [PubMed]
- Salvati EA, Bullough P, Wilson PD Jr. Intrapelvic protrusion of the acetabular component following total hip replacement. 1975. Clin Orthop Relat Res 2006;8-12. [Crossref] [PubMed]
- Płomiński J, Kwiatkowski K. Cemented primary total arthroplasty for acetabular protrusion in patients with rheumatoid arthritis. Ortop Traumatol Rehabil 2008;10:26-34. [PubMed]
- Mori Y, Mori N, Mori T, et al. Risk of acetabular protrusion is low in rheumatoid arthritis patients treated with bipolar hemiarthroplasty for displaced femoral neck fractures without rheumatoid change in hip joints. Eur J Orthop Surg Traumatol 2014;24:905-9. [Crossref] [PubMed]
- Garcia-Cimbrelo E, Diaz-Martin A, Madero R, et al. Loosening of the cup after low-friction arthroplasty in patients with acetabular protrusion. The importance of the position of the cup. J Bone Joint Surg Br 2000;82:108-15. [Crossref] [PubMed]
- Firestone TP, Hedley AK. Extended proximal femoral osteotomy for severe acetabular protrusion following total hip arthroplasty. A technical note. J Arthroplasty 1997;12:344-5. [Crossref] [PubMed]
- Seagrave KG, Troelsen A, Malchau H, et al. Acetabular cup position and risk of dislocation in primary total hip arthroplasty. Acta Orthop 2017;88:10-7. [Crossref] [PubMed]
- Cech A, Kase M, Kobayashi H, et al. Pre-operative planning in THA. Part III: do implant size prediction and offset restoration influence functional outcomes after THA? Arch Orthop Trauma Surg 2020;140:563-73. [Crossref] [PubMed]
- Kung PL, Ries MD. Effect of femoral head size and abductors on dislocation after revision THA. Clin Orthop Relat Res 2007;170-4. [Crossref] [PubMed]
- Shapiro GS, Weiland DE, Markel DC, et al. The use of a constrained acetabular component for recurrent dislocation. J Arthroplasty 2003;18:250-8. [Crossref] [PubMed]
- Hernigou P, Ratte L, Roubineau F, et al. The risk of dislocation after total hip arthroplasty for fractures is decreased with retentive cups. Int Orthop 2013;37:1219-23. [Crossref] [PubMed]
- Jeong M, Kim HJ, Lim SJ, et al. Revision Total Hip Arthroplasty Using Tantalum Augment in Patients with Paprosky III or IV Acetabular Bone Defects: A Minimum 2-year Follow Up Study. Hip Pelvis 2016;28:98-103. [Crossref] [PubMed]
Cite this article as: Prod’homme M, Dietrich G, Helfer L, Müller JP, Barrera Uso M, Grasset D, Lallemand G. Major acetabular prosthetic protrusion following total hip arthroplasty: a case report of a reconstruction challenge. AME Case Rep 2022;6:24.