
Electromagnetic navigation bronchoscopy transbronchial lung nodule ablation with IllumisiteTM platform corrects CT-to-body divergence with tomosynthesis and improves ablation workflow: a case report
Introduction
Patients with multifocal lung cancers or multiple lung oligometastases are candidates for lung-preserving treatment options (1,2), among which local ablative therapies are increasing in interests and applications (3-5). Transbronchial route of local ablation using microwave energy in the hybrid operating room (HOR) has been described, yielding good short-term safety and mid-term local control rates (6). However, this is limited by CT-to-body divergence, leading to imprecision of navigation. The IllumisiteTM platform utilizes real-time imaging to correct for the CT-to-body divergence, in addition to fluoroscopic navigation technology to enhance the visibility of lung nodules. Alignment with the target nodule is visualized and maintained throughout procedure as the tip of the extended working channel (EWC) provides positional information even after the locatable guide (LG) has been removed. We present below our first case of electromagnetic navigation bronchoscopy (ENB) transbronchial microwave ablation of lung nodule using the IllumisiteTM platform in the HOR. We present this case in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-22-49/rc).
Case presentation
A 66-year-old lady with a past history of multiple treated lung adenocarcinomas was found to have growing suspicion of one of the remaining lung nodules. She had a T2N0M0 EGFR G719X mutation positive lung adenocarcinoma with right lower lobectomy 5 years ago, showing complete resection and not requiring adjuvant treatment. Subsequent CT showed 2 more suspicious left lower lobe nodules which were wedge-resected 1 year ago, pathology showing a 4 mm EGFR mutation negative adenocarcinoma-in-situ and a 1 mm atypical adenomatous hyperplasia. Upon follow up of the remaining multiple ground-glass opacities (GGO) in bilateral lungs, one in the right middle lobe (RML) (Suzuki class 3) had increased in size and solidity slowly over years. Her forced expiratory volume in 1 second (FEV1) was 110% predicted while diffusion capacity of carbon monoxide (DLCO) was 68% predicted. Thoracic multi-disciplinary meeting concluded that this mixed RML nodule was likely an evolving early primary lung adenocarcinoma similar to the previous resected nodules. The patient was referred to us for lung-conserving ablative therapy, since there were other lung nodules scattered in bilateral lobes which may require future treatment in case of progression. The target RML nodule was approximately 1 cm in maximal diameter, adjacent to a 3 mm vessel bifurcation, with a narrow airway leading to the lesion (bronchus sign positive). It consisted of mostly GGO with a solid centre (Figure 1). The patient agreed for transbronchial ENB microwave ablation of the lung nodule after discussion of other local treatment options, and informed consent was taken.
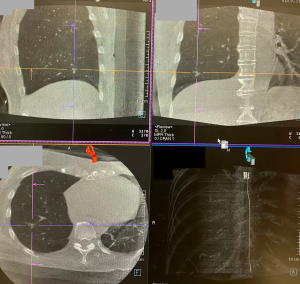
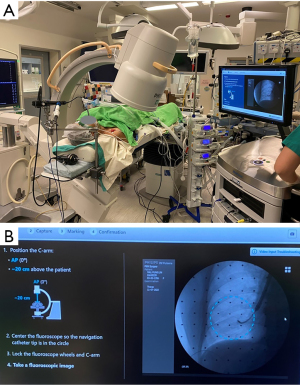
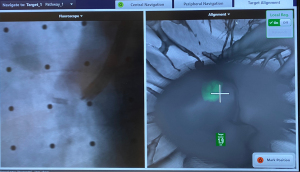
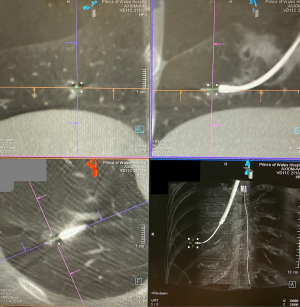
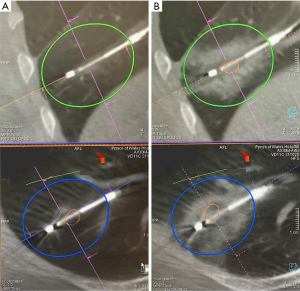
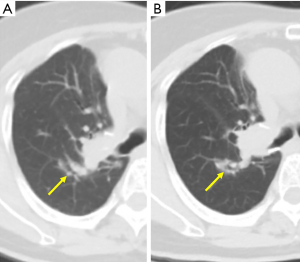
On the day of procedure, the patient underwent general anaesthesia and was intubated with single lumen endotracheal tube. Similar to all other ENB cases, bronchoscopic toileting and pre-operative cone-beam CT (CBCT) was performed (Figure 1), followed by registration and navigation by the IllumisiteTM ENB system. A 180-degree EWC was used and the LG was navigated to a point just within 2.5 cm from the centre of lesion. Local registration by fluoroscopic navigation to correct for CT-body divergence was performed using a mobile C-arm 60-degree spin to generate tomosynthesis images (Figure 2). The GGO was not readily seen on fluoroscopy, but the nodule marking was accurate based on the visualized adjacent vessels (Figure 3). By comparing the 3D reconstructed view to the 2D fluoroscopy image, the lesion was much better visualized and can be marked for subsequent navigation. After the position of the green ball (representing the target lesion) was adjusted by IllumisiteTM platform, the LG was renavigated to a more distal airway, and with the help of CBCT and fluoroscopy, the LG was directly aligned with the adjusted target (Figure 4). A CrossCountryTM needle (CovidienTM, Plymouth, MN, USA) for transbronchial access was deployed with patient in inspiration, corresponding to the green ball’s most bullseye view. CBCT showed the needle puncturing through the GGO (Figure 5), and the dilator and EWC was advanced over the needle to the desired position. Due to the positional electronics available in the tip of the IllumisiteTM EWC, we placed it at 1 cm beyond the centre of GGO lesion so that the centre of ablation zone will coincide with the centre of lesion. The CrossCountryTM tool was then exchanged to EmprintTM Ablation Catheter (CovidienTM, Plymouth, MN, USA) and unsheathed, with the final CBCT showing satisfactory position with predicted ablation margin >10 mm. The predicted ablation margin is defined as the minimal distance between edge of lesion and edge of predicted ablation zone, the size of which was provided by the manufacturer. After the first ablation with 100 W for 10 minutes, the ablated zone was smaller than predicted especially over the side where there was heat sink effect due to the 3 mm blood vessel. Re-ablation at the same position with 100 W for 10 minutes was performed, CBCT showed ablation zone being more consolidated and minimal margin improved to 4 mm, not taking into account tissue contraction from ablation (Figure 6). Total procedure time was 171 minutes and radiation dose was 26,129 µGym2.

The patient had uneventful recovery and was discharged on post operative day 1; 16 days later, the patient received right upper lobectomy for resection of multiple right upper lobe nodules. The post-ablation 1-month and 4-month CT scans show shrinkage of ablation zone (Figure 7) and no short-term complications or early recurrence.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
This is the first case of ENB transbronchial microwave ablation of lung nodule using the IllumisiteTM platform in the HOR. The IllumisiteTM platform is the first navigational system on market to correct for CT-to-body divergence, that is the discrepancy between the static pre-operative planning CT scan and the dynamic breathing lung. This digital tomosynthesis-based navigation correction is achieved by utilizing fluoroscopic navigation technology which creates a 3D image enhancing the nodule’s visibility, so that the adjusted nodule position (represented by the green ball on screen) can be updated. Throughout procedure, it provides real time confirmation that the catheter is aligned to the nodule, and this alignment can be maintained even after the LG is removed, owing to the presence of sensor coils embedded in the tip of EWC. This continuous positional data allows for multidirectional sampling and more thorough biopsy, as have been demonstrated in biopsy series using this platform (7,8).
The improved navigation and accuracy provided by this platform may also simplify the workflow of transbronchial microwave lung ablation. In the present case, the unadjusted green ball position initially led us to a more superior airway, but after nodule adjustment with fluoroscopic navigation technology, we were able to quickly recognize that the LG was in a slightly different airway and renavigated accordingly. Fewer numbers of CBCT and therefore less radiation was required in order to confirm that the LG had reached the target nodule. In addition, in previous models without EWC positional electronics, after the LG is removed the EWC often returns to its original curvature, and deployment of subsequent CrossCountryTM needle would require fluoroscopy marking and multiple confirmation in right anterior oblique (RAO) and left anterior oblique (LAO) planes. Often after needle deployment, CBCT would show that the needle is slightly off-centre and redeployment of needle was required, especially for ablation where a high level of precision is required. With the continuous positional data provided by the tip of the new system’s EWC, we would be able to advance the CrossCountryTM needle directly at the green ball in the most bullseye view, and CBCT indeed confirmed direct puncture of the nodule. Moreover, contrary to previous platforms, apart from the direction, the exact distance between the centre of nodule and the tip of EWC is available too, allowing precise placement of the tip of ablation catheter. Since the centre of ablation is 1 cm proximal to the tip of EmprintTM ablation catheter, we advanced the EWC 1 cm beyond the centre of lesion and placed the ablation catheter flush to the EWC, so that the centre of ablation coincided with the centre of lesion. This is confirmed by CBCT and did not require further adjustment of the catheter before ablation.
In general, the IllumisiteTM platform improves navigational accuracy and is best suited to institutions where CBCT is a scarce resource (9). For biopsy, the fluoroscopic navigation technology with adjustment of green ball location is probably sufficient for accurate biopsy without the need of CT to confirm needle position. However, for lung ablation, without a hybrid theatre and floor-mounted CBCT, one would rely on mobile CBCT machines for lung nodule ablation, and each CBCT requires additional time and effort. Therefore, the workflow of ablation and biopsy can be greatly improved by decreasing the number of CBCT spins required for confident instrument placement.
The accuracy of IllumisiteTM platform is still limited by the solidity of lesion. Solid components in mixed GGOs can be augmented by tomosynthesis much more than pure GGOs. In addition, the need for parking and unparking of mobile C-arm machine in a hybrid theatre with floor-mounted CBCT machine may prolong procedure, however this may be offset by more accurate navigation in the first attempt, thus saving time from repeated CBCT spins due to mis-navigation related to CT-to-body divergence. Total radiation dose in the present case was 26,129 µGym2, only slightly less than the average of 27,120 µGym2 in our previous case series of ENB ablation. This may be due to the effect of initial learning curve of using the new platform, and the need of double ablation in this case.
Conclusions
IllumisiteTM is an advance electromagnetic navigation platform that corrects for CT-to-body divergence by fluoroscopic navigation technology. Accurate access to nodule is ensured by the adjusted nodule location, and continuous positional data is provided by the novel embedment of positional coils at the tip of EWC. This precision is especially important for the placement of ablation catheter, as slight deviation would lead to insufficient ablation margin and future recurrence.
Acknowledgments
Funding: This study was supported by Research Grants Council (RGC) Hong Kong, General Research Fund (GRF) No. 14119019.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, AME Case Reports for the series “Case Reports in Hybrid Operating Theatre”. The article has undergone external peer review.
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-22-49/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-22-49/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-22-49/coif). The series “Case Reports in Hybrid Operating Theatre” was commissioned by the editorial office without any funding or sponsorship. JWYC served as the unpaid Guest Editor of the series. RWHL is a consultant for Medtronic, USA; Johnson & Johnson; and Siemens Healthineer. CSHN served as the unpaid Guest Editor of the series and serves as an unpaid editorial board member of AME Case Reports. CSHN is a consultant for Medtronic, USA; Johnson and Johnson; and Siemens Healthineer. All remaining authors declare no potential conflicts of interest that exist with any companies/organizations whose products or services are discussed in this article. The IllumisiteTM platform (Medtronic, Minneapolis, MN, USA) is not involved in the management of the case, and all authors declare no financial interest with the above device company. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Chan JWY, Lau R, Chang A, et al. 96P Transbronchial microwave ablation: Important role in the battle of lung preservation for multifocal lung primaries or metastases. Ann Oncol 2022;33:S76-7. [Crossref]
- Chan JWY, Lau RWH, Ng CSH. Image-Guided Ablative Therapies for Lung Tumors. Lung Cancer - Modern Multidisciplinary Management 2021. doi:
10.5772/intechopen.94216 .10.5772/intechopen.94216 - Xie F, Zheng X, Xiao B, et al. Navigation Bronchoscopy-Guided Radiofrequency Ablation for Nonsurgical Peripheral Pulmonary Tumors. Respiration 2017;94:293-8. [Crossref] [PubMed]
- Niu L, Xu K, Mu F. Cryosurgery for lung cancer. J Thorac Dis 2012;4:408-19. [PubMed]
- Yuan HB, Wang XY, Sun JY, et al. Flexible bronchoscopy-guided microwave ablation in peripheral porcine lung: a new minimally-invasive ablation. Transl Lung Cancer Res 2019;8:787-96. [Crossref] [PubMed]
- Chan JWY, Lau RWH, Ngai JCL, et al. Transbronchial microwave ablation of lung nodules with electromagnetic navigation bronchoscopy guidance-a novel technique and initial experience with 30 cases. Transl Lung Cancer Res 2021;10:1608-22. [Crossref] [PubMed]
- Avasarala SK, Roller L, Katsis J, et al. Sight Unseen: Diagnostic Yield and Safety Outcomes of a Novel Multimodality Navigation Bronchoscopy Platform with Real-Time Target Acquisition. Respiration 2022;101:166-73. [Crossref] [PubMed]
- Dunn BK, Blaj M, Stahl J, et al. Evaluation of Electromagnetic Navigational Bronchoscopy Using Tomosynthesis-Assisted Visualization, Intraprocedural Positional Correction and Continuous Guidance for Evaluation of Peripheral Pulmonary Nodules. J Bronchology Interv Pulmonol 2023;30:16-23. [Crossref] [PubMed]
- Zhao ZR, Lau RW, Ng CS. Hybrid theatre and alternative localization techniques in conventional and single-port video-assisted thoracoscopic surgery. J Thorac Dis 2016;8:S319-27. [PubMed]
Cite this article as: Chan JWY, Chang ATC, Siu ICH, Lau RWH, Ng CSH. Electromagnetic navigation bronchoscopy transbronchial lung nodule ablation with IllumisiteTM platform corrects CT-to-body divergence with tomosynthesis and improves ablation workflow: a case report. AME Case Rep 2023;7:13.


