Case report: video-assisted thoracoscopic repair of right main bronchus transection after blunt chest injury
Highlight box
Key findings
• Rt main bronchial transection.
What is known and what is new?
• Current standard treatment for traumatic transection of right main bronchial injury is open thoracotomy. Minimally invasive surgery could be alternative approach for this injury.
What is the implications, and what should change now?
• VATS approach could be an alternative choice which is safe and effective compare to standard approach.
Introduction
Blunt tracheal injury is a rare condition that accounts for 0.5–2.0% of all blunt trauma (1). It usually occurs within 2 cm of the right main stem bronchus due to the relatively fixed position of the carina in the chest and its reduced protection from mediastinal organs. Blunt tracheal injury typically presents with massive subcutaneous emphysema and unilateral or bilateral pneumothorax, which may result in respiratory failure. Bronchoscopy is the primary method of diagnosis, and computed tomography (CT) of the chest is an adjunct imaging modality. We present the following case in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-22-83/rc).
Case presentation
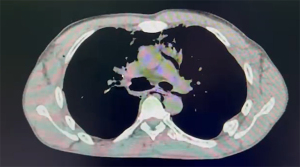
This case report was approved by the Institutional Review Board of Vajira Hospital, Navamindradhiraj University (COE No. 17/2022X). All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal. A 44-year-old male patient suffered a blunt chest injury after a large metallic plate fell from a height and direct crushed at his upper trunk. He was transported to the emergency room of a local hospital. At emergency room, his blood pressure was 140/85 mmHg, and the heart rate was 110/min with 88% of oxygen saturation at room air. Chest radiography revealed mediastinal emphysema and intercostal chest drain was placed (Figure 1). a chest CT with intravenous contrast was performed to further evaluate the mediastinal emphysema. The chest CT revealed right main bronchus injury, mediastinal emphysema, right pneumothorax, and fracture of the 2nd–4th right ribs (Figure 2). Hence, the patient was referred to our institution (Faculty of Medicine, Vajira Hospital, Navamindradhiraj University, Bangkok, Thailand) for surgical treatment. After obtaining informed consent from the patient and his family, Video-assisted thoracoscopic surgery (VATS) repair of the right main bronchus was immediately performed under emergent conditions.
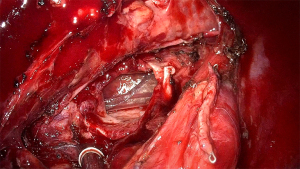
General anesthesia was induced and the right lung was isolated by inserting a double-lumen endotracheal tube into the left main bronchus under fiber optic guidance. We performed uniport VATS from the right 4th intercostal space. Intraoperatively, the azygos vein was divided to expose the injury site, and the transected right main bronchus was identified at the proximal carina (Figure 3). Tracheal release maneuvers were performed, such as division of the inferior pulmonary ligament and the right hilum, to decrease tension between the carina and the right main bronchus. A U-shaped incision was created in the pericardium near hilar region. We used polypropylene 4-0 as running sutures to anastomose the posterior wall of the trachea and the right main bronchus. For the rest of anterior wall anastomosis, we used polypropylene 4-0 as simple interrupted sutures. The anastomosis line was tested under water with positive pressure ventilation of 30 mmHg, secured by the application of fibrin sealant glue, and buttressed with pericardial fat pad tissue. Two chest tubes were placed at the anterior and posterior thorax. Postoperative bronchoscopy was performed to evaluate the anastomosis. The patient was extubated intra-operative and transferred to the intensive care unit. Both of chest tube was removed on postoperative day 3. On postoperative day 7, a bronchoscopy was performed and revealed good anastomosis. The patient was discharged the next day. He reported no dyspnea and only minimal pain at the surgical site at follow-up in our out-patient department 4 weeks after discharge. His chest X-ray showed full right lung expansion with no residual pneumothorax or effusion.
Discussion
Currently, there are no standard guidelines for the treatment of traumatic tracheobronchial injury; however, Cardillo et al. have proposed morphologic classification of injury from level I to level IIIB (2). Consequently, surgery is primarily indicated in traumatic tracheobronchial injury classifications of IIIA or IIIB, along with the deterioration of the patient’s condition, such as impending respiratory failure (3). In contrast, conservative treatment is popular in selected patients, i.e., if there is no risk of surgery or long-term morbidity. Farley et al. have suggested that conservative strategies should be explored in the following scenarios: iatrogenic tracheal injury, if the laceration is >2 cm long, there are no concomitant injuries, and if the patient can be stabilized without the persistence of symptoms (4). Conservative management can be done by passing the endotracheal with balloon cuff distal to the injury site with PEEP and low tidal volume for 7–14 days. Bronchoscope is needed to ensure good healing of the injury site. Some of the cases might be needed stent placement. Nevertheless, stenting is becoming more popular as it is less invasive, despite the risk of stent migration, fracture, or infection (4). At present, there are many wide types of stents and shapes including straight, T and Y shape, and silicone and metallic with metallic stent having varying degrees of coating. As a result, the selection in of stent in tracheal injury is still art (5). Therefore, the future of stenting appears promising.
VATS is a well-developed technique that has become a standard procedure in recent decades. Multiple procedures, such as wedge resection, pleural biopsy, and lobectomy or tracheal resection have been performed under VATS. However, VATS surgery is very challenging in trauma patients due to multiple organ injuries or tissue trauma, ill-defined surgical plane, and time-sensitive surgery. Therefore, the standard approach for right main stem bronchial injury remains thoracotomy or even clamshell incision in some cases, with a repair under direct inspection. To the best of our knowledge, this is the first description of the use of VATS for the repair of blunt traumatic right main bronchial injury. This technique has several benefits compared to the conventional approach, such as lower postoperative pain, less tissue trauma, and better visualization of the surgical field (6).
We believe that VATS represent an alternative approach for the repair of the right main bronchus transection after a blunt chest injury.
Conclusions
Blunt traumatic tracheal injury is a rare disease after blunt chest injury. VATS repair is safe and feasible as an alternative approach to conventional thoracotomy approach.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-22-83/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-22-83/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-22-83/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This case report was approved by the Institutional Review Board of Vajira Hospital, Navamindradhiraj University (COE No. 17/2022X). All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Karmy-Jones R, Wood DE. Traumatic injury to the trachea and bronchus. Thorac Surg Clin 2007;17:35-46. [Crossref] [PubMed]
- Cardillo G, Carbone L, Carleo F, et al. Tracheal lacerations after endotracheal intubation: a proposed morphological classification to guide non-surgical treatment. Eur J Cardiothorac Surg 2010;37:581-7. [Crossref] [PubMed]
- Grewal HS, Dangayach NS, Ahmad U, et al. Treatment of Tracheobronchial Injuries: A Contemporary Review. Chest 2019;155:595-604. [Crossref] [PubMed]
- Farley LS, Schlicksup KE. Tracheal Injury. Treasure Island (FL): StatPearls Publishing; 2022.
- Flannery A, Daneshvar C, Dutau H, et al. The Art of Rigid Bronchoscopy and Airway Stenting. Clin Chest Med 2018;39:149-67. [Crossref] [PubMed]
- Li J, Wang W, Jiang L, et al. Video-Assisted Thoracic Surgery Resection and Reconstruction of Carina and Trachea for Malignant or Benign Disease in 12 Patients: Three Centers' Experience in China. Ann Thorac Surg 2016;102:295-303. [Crossref] [PubMed]
Cite this article as: Yu J, Laohathai S. Case report: video-assisted thoracoscopic repair of right main bronchus transection after blunt chest injury. AME Case Rep 2023;7:17.