
Heterotopic pancreas in Meckel’s diverticulum in an adult man with lower gastrointestinal bleeding: a case report and literature review
Highlight box
Key findings
• We presented a case of an adult man presented with recurrent hematochezia and finally diagnosed with heterotopic pancreas in Meckel’s diverticulum, combining double balloon enteroscopy and pathology study post laparoscopy.
What is known and what is new?
• Meckel’s diverticulum is a rare blind-end true diverticulum that contains all layers, normally found in the ileum. GI bleeding is a common complication of Meckel’s diverticulum.
• Heterotopic pancreas in Meckel’s diverticulum is a rare clinical situation. Herein, we presented a man in his 40s with lower GI bleeding, whose diagnosis comes out as heterotopic pancreas in Meckel’s diverticulum.
What is the implication, and what should change now?
• Heterotopic pancreas in Meckel’s diverticulum is a relatively rare clinical condition in adult which can cause recurrent lower GI bleeding. Thus, special attention should be paid in cases with unexplained lower gastrointestinal bleeding in adult.
Introduction
Heterotopic pancreas, or so-called ectopic pancreas, accessory pancreas, aberrant pancreas, and pancreatic heterotopia, is defined as pancreatic tissue outside its usual location, without anatomical or vascular continuity of pancreas proper (1). The incidence of heterotopic pancreas is at a large range of 0.5% to 14.0% in autopsy studies, which is a rare clinical situation and can be found in any site of the alimentary system, mostly in the stomach, duodenum and jejunum, and then other organs include esophagus, terminal ileum, omentum, mesentery, spleen, liver, Meckel’s diverticulum, colon, ampulla of Vater, gallbladder, urinary bladder, lung and lymph nodes as well (2).
Meckel’s diverticulum is a blind-end true diverticulum that contains all layers, normally found in the ileum (3). Prevalence of Meckel’s diverticulum is around 2% in the population, and even rare among adults (4). Gastrointestinal (GI) bleeding is a common complication of Meckel’s diverticulum and in most cases, caused by peptic ulceration of the diverticulum or adjacent mucosa, due to ectopic gastric mucosa, while in minority cases, pancreatic tissue would also appear in around 6% of all Meckel’s diverticulum patients (5). Herein, we present a case of heterotopic pancreas in Meckel’s diverticulum in a 45-year-old adult, who presented to our hospital for hematochezia of over one-month. We present the following case in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-22-105/rc).
Case presentation
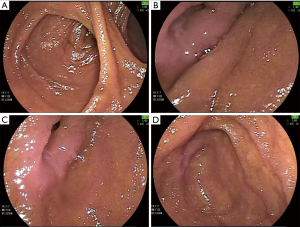
A 45-year-old man presented with recurrent hematochezia for over one-month in our hospital. Over one month ago, our patient started to have loose bloody stool five to six times per day, without abdominal pain, hemorrhoids, loss of weight, etc. He visited local hospital, where both gastroscopy and colonoscopy were negative. The patient did not present with remarkable comorbidities, with no history of either drinking or smoking, no home medication or drug abuse. On physical examination at initial contact, he did not reveal any abnormalities. Weight was stable with body mass index of 23.1 kg/m². In blood laboratory examinations, the patient presented with mild anemia of hemoglobin 114 g/L and otherwise unremarkable, including platelet, coagulation function, tumor markers, blood biochemistry, auto-immune studies, etc. Fecal routine showed ++++ in stool occult blood test but no red blood cell was seen. Contrasted abdominopelvic computerized tomography (CT) was normal and Meckel’s electroconvulsive therapy (ECT) for identification of ectopic gastric mucosa was also negative. Thus, small intestine bleeding was suspected and double balloon enteroscopy was adopted which revealed double duct sign at about 100 cm proximal to ileocecal valve and indicated existence of diverticulum (Figure 1A). Further, ulceration was found and the far-end bottom of the blind-ending tube (Figure 1B-1D).
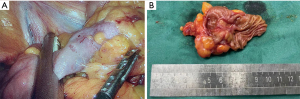
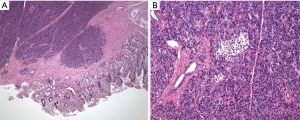
Finally, heterotopic pancreas in Meckel’s diverticulum was diagnosed based on double balloon enteroscopy and verified by further pathology study of surgical specimen (Figure 2A,2B). The patient then underwent laparoscopic resection of Meckel’s diverticulum under general anesthesia. The patient was placed in supine position, and conventional disinfection was carried out. During surgery, intraoperative exploration showed no obvious ascites, no obvious abnormalities in abdominal wall or pelvic cavity. While a diverticula-like mass with 3 cm × 2 cm in size was found in the intestine at about 1 meter away proximal to the ileocecal valve, with clear boundary and then complete resection was conducted (Figure 3A). And the ulcer in the diverticula-like mass was 0.5 cm × 0.6 cm in size and 0.3 cm in depth. Pathology study showed heterotopic pancreas in Meckel’s diverticulum with negative margins on both sides of ectopic pancreas (Figure 3B). The surgery underwent smoothly and the patient started feeding two days post-surgery.
The patient was discharged two weeks after surgery with resolve of anemia and absence of hematochezia recurrence. The patient was further arranged with a monthly follow-up in outpatient clinic.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Meckel’s diverticulum is one of the most common congenital malformations of the gastro-intestinal tract, of which incidence ranging from 0.14% to 4.5% in a previous autopsy study, with male-dominant pattern at the ratio of nearly 2:1, but no ethnic tendency (6). In children (under 10 years), the most common age group of presentation is infants (under 1 year of age), while in the adolescent/adult group, the most common age for symptomatic ones is between 11 and 30 years of age (5). And herein, we presented an adult in his 40s with Meckel’s diverticulum presenting with lower GI bleeding, which is a relatively rare clinical situation.
Meckel’s diverticulum is usually clinically asymptomatic, particularly in adults, while the others would present intestinal obstruction, GI bleeding, and inflammation with or without perforation. Interestingly, clinical presentation of Meckel’s diverticulum follows an age-trend: almost half of all children with Meckel’s diverticulum present symptoms of rectal bleeding or intussusception before 2 years of age; while adult patients tend to present with inflammation or obstruction rather than bleeding (7). Since our case presented an adult man, whose chief complaint is hematochezia, we analyzed and found that, on the other hand, for all patients with lower GI bleeding, Meckel’s diverticulum accounts for a relatively large proportion as 20–55% of all cases, indicating that special attention should be paid when encountering adult lower GI bleeding cases in real clinical situation (8).
Diagnosis of Meckel’s diverticulum might be sort of challenging, and traditional diagnostic approaches usually include ultrasonography, CT scan, magnetic resonance imaging (MRI), and Meckel’s ECT, but with relatively low detecting rate, thus in some cases finally leads to diagnostic laparoscopy (5). Previous small sample pilot studies raised possibility and advantage of capsule endoscopy in identifying bleeding Meckel’s diverticulum when conventional modalities (gastroscopy, colonoscopy, CT and Meckel’s ECT) did not show any lesion, in which cases, either a double-duct sign, with or without bleeding was discovered, indicating capsule endoscopy as an effective and promising modality which can potentially be of added value in the diagnosis, especially bleeding, of Meckel’s diverticulum in the future (9,10). Moreover, in recent years, as development of double balloon enteroscopy, Meckel’s diverticulum would also be helpful, as in our case, specific refined structure could be well observed and even biopsied under enteroscopy was possible, providing a new approach of Meckel’s diverticulum diagnosis and thus raising positive rate of diagnostic laparoscopy. A recent study even proposed the possibility of treatment under double balloon enteroscopy, such as argon plasma coagulation, balloon dilatation, polypectomy, etc., but still need further experience (11).
Etiology of heterotopic pancreas in Meckel’s diverticulum is still unclear. In Meckel’s diverticulum, the intestinal mucosa which lines both the walls of ileum and also Meckel’s, but frequently the Meckel’s contains ectopic tissue, commonly gastric tissue (12). In rare cases of 0–12%, pancreatic tissue also lines in Meckel’s (13). As for formation of heterotopic pancreatic tissue, it is believed to arise embryonically during rotation of the foregut and fusion of the dorsal as well as ventral pancreatic buds or from the pancreatic metaplasia of endodermal tissue (14). On the other hand, as for heterotopic pancreas, the most common location is the upper GI tract, especially the stomach, duodenum, and proximal jejunum and less common sites are the esophagus, ileum, Meckel’s diverticulum, and biliary tree, or in some rare cases, heterotopic pancreas may also be reported in mediastinum, lungs, spleen, fallopian tubes, umbilicus, and omentum as well (15). GI bleeding is an associated complication of heterotopic pancreas. The cause of GI bleeding in patients with heterotopic pancreas is thought to be the ulcerated mucosal barrier overlying the abnormal lesion, which can be explained by two reasons. First chemical stimulation and inflammation can cause destruction of gastric mucosa, and second, pancreatic enzymes, like elastase, can lead to the corrosion and thinning of vessel walls (16). A case series have reported ulceration of mucosa in patients with evident bleeding, which strongly supported ulceration as the etiology of GI bleeding (17).
It is commonly acknowledged that ectopic gastric mucosa or pancreatic tissue is what causes GI bleeding brought on by peptic ulcer in Meckel’s diverticulum (MD) (18). According to a study, symptoms are present in about 2–4% of all cases of MD, while it can be up to 60% of cases of MD with ectopic tissue (18). However, Takeyama J pointed out that Dieulafoy’s lesion (DL), a vascular abnormality, is the actual cause of GI bleeding in MD, with 100% detection rate of DL in 10 cases, and no ectopic tissue was found in one of the cases (19). This finding suggests that ectopic tissue may not be the only reason of GI bleeding in MD. However, DL was not found in our case and the ulceration was evident, we believe it was the heterotopic pancreas that caused GI bleeding. But for those cases with GI bleeding in MD in which no ectopic tissue is found or ulceration is not evident, DL has to be considered and special examinations like pieces of step sections or angiography are needed to distinguish if GI bleeding is caused by DL.
Treatment principle of Meckel’s diverticulum is dependent on whether it is complicated or incident. Surgical resection is the consensus of complicated Meckel’s diverticulum treatment, diverticulectomy, wedge or segmental resection, either through laparoscopically or with laparotomy. As for the incident Meckel’s diverticulum, whether or not to operate is still controversial. Early expertise advocated that since only a small chance of asymptomatic Meckel’s diverticulum would become symptomatic during the whole lifetime, surgery is not necessary considering preventing death in the last century (20). While later, different voices spring up that risk factors should be taken into account when deciding whether or not to resect incident Meckel’s diverticulum. These risk factors include age over 50, male gender, diverticulum length over 2 cm, presence of abnormal tissue on histopathological examination, broad-based diverticulum, and presence of fibrous bands attached to the diverticulum (3).
Conclusions
In conclusion, Meckel’s diverticulum is a rare blind-end true diverticulum that contains all layers, normally found in the ileum. GI bleeding is a common complication of Meckel’s diverticulum and in most cases, caused by peptic ulceration due to ectopic gastric mucosa. While herein, we presented a case of an adult man presented with recurrent hematochezia and finally diagnosed with heterotopic pancreas in Meckel’s diverticulum, combining double balloon enteroscopy and pathology study post laparoscopy. Special attention should be paid to cases with unexplained recurrent lower GI bleeding in adults.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-22-105/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-22-105/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-22-105/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Yang X, Guo K. Massive lower gastrointestinal bleeding from Meckel's diverticulum with heterotopic pancreas: case report and a brief review of the literature. JOP 2013;14:269-72. [PubMed]
- Dutei C, Husar-Sburlan IA, Tudor S, et al. Heterotopic pancreas located in the ileum. J Gastrointestin Liver Dis 2017;26:335. [Crossref] [PubMed]
- Kuru S, Kismet K. Meckel's diverticulum: clinical features, diagnosis and management. Rev Esp Enferm Dig 2018;110:726-32. [Crossref] [PubMed]
- Choi SY, Hong SS, Park HJ, et al. The many faces of Meckel's diverticulum and its complications. J Med Imaging Radiat Oncol 2017;61:225-31. [Crossref] [PubMed]
- Lindeman RJ, Søreide K. The Many Faces of Meckel's Diverticulum: Update on Management in Incidental and Symptomatic Patients. Curr Gastroenterol Rep 2020;22:3. [Crossref] [PubMed]
- Lequet J, Menahem B, Alves A, et al. Meckel's diverticulum in the adult. J Visc Surg 2017;154:253-9. [Crossref] [PubMed]
- Rossi P, Gourtsoyiannis N, Bezzi M, et al. Meckel's diverticulum: imaging diagnosis. AJR Am J Roentgenol 1996;166:567-73. [Crossref] [PubMed]
- Strate LL, Gralnek IM. ACG Clinical Guideline: Management of Patients With Acute Lower Gastrointestinal Bleeding. Am J Gastroenterol 2016;111:459-74. [Crossref] [PubMed]
- Silva M, Cardoso H, Peixoto A, et al. The role of capsule endoscopy in urgent evaluation of obscure gastrointestinal bleeding: a case series of Meckel diverticulum. Arq Bras Cir Dig 2018;31:e1409. [Crossref] [PubMed]
- Krstic SN, Martinov JB, Sokic-Milutinovic AD, et al. Capsule endoscopy is useful diagnostic tool for diagnosing Meckel's diverticulum. Eur J Gastroenterol Hepatol 2016;28:702-7. [Crossref] [PubMed]
- Olafsson S, Yang JT, Jackson CS, et al. Bleeding Meckel's diverticulum diagnosed and treated by double-balloon enteroscopy. Avicenna J Med 2012;2:48-50. [Crossref] [PubMed]
- Chen JJ, Lee HC, Yeung CY, et al. Meckel's Diverticulum: Factors Associated with Clinical Manifestations. ISRN Gastroenterol 2014;2014:390869. [Crossref] [PubMed]
- Piñero A, Martínez-Barba E, Canteras M, et al. Surgical management and complications of Meckel's diverticulum in 90 patients. Eur J Surg 2002;168:8-12. [Crossref] [PubMed]
- Biswas A, Husain EA, Feakins RM, et al. Heterotopic pancreas mimicking cholangiocarcinoma. Case report and literature review. JOP 2007;8:28-34. [PubMed]
- Kung JW, Brown A, Kruskal JB, et al. Heterotopic pancreas: typical and atypical imaging findings. Clin Radiol 2010;65:403-7. [Crossref] [PubMed]
- LeCompte MT, Mason B, Robbins KJ, et al. Clinical classification of symptomatic heterotopic pancreas of the stomach and duodenum: A case series and systematic literature review. World J Gastroenterol 2022;28:1455-78. [Crossref] [PubMed]
- Pang LC. Pancreatic heterotopia: a reappraisal and clinicopathologic analysis of 32 cases. South Med J 1988;81:1264-75. [Crossref] [PubMed]
- Keese D, Rolle U, Gfroerer S, et al. Symptomatic Meckel's Diverticulum in Pediatric Patients-Case Reports and Systematic Review of the Literature. Front Pediatr 2019;7:267. [Crossref] [PubMed]
- Takeyama J. Meckel's Diverticulum with Dieulafoy's Lesion: A Cause of Severe Hematochezia. Fetal Pediatr Pathol 2022;41:865-70. [Crossref] [PubMed]
- Soltero MJ, Bill AH. The natural history of Meckel's Diverticulum and its relation to incidental removal. A study of 202 cases of diseased Meckel's Diverticulum found in King County, Washington, over a fifteen year period. Am J Surg 1976;132:168-73. [Crossref] [PubMed]
Cite this article as: Chen S, Zhang H, Yu X, Chen Y. Heterotopic pancreas in Meckel’s diverticulum in an adult man with lower gastrointestinal bleeding: a case report and literature review. AME Case Rep 2023;7:19.


