
Juvenile psammomatoid ossifying fibroma of the ethmoid sinus successfully treated by endoscopic sinus surgery: a case report
Highlight box
Key findings
• JPOF may be treated successfully with endoscopic sinus surgery (ESS).
What is known and what is new?
• Recurrence rate and anatomical preservation are the main challenges in the treatment of JPOF.
• ESS may guarantee preservation of structures even in revision surgery after JPOF’s recurrence.
What is the implication, and what should change now?
• Further research should investigate the real time CT-assisted ESS and the adjuvant interferon alpha therapy in the treatment of JPOF.
Introduction
Ossifying fibroma is a benign tumour first described by Menzel in 1872, characterized by the replacement of normal bone tissue with a fibrous cellular stroma that contains numerous foci of mineralization (1). It generally occurs in patients in their second to the fourth decade, women are more commonly affected than men and there is no evidence of inheritance (2). Ossifying fibromas of the head and neck are rare, mostly affecting the mandible/maxilla and rarely the orbit, the skull base, and the paranasal sinuses (3). The term “juvenile” is used when patients under 15 years old are affected.
The juvenile variant tends to be locally aggressive, with high risk of recurrence if incompletely removed. Juvenile ossifying fibromas (JOF) are usually divided into two subtypes: trabecular (JTOF) and psammomatoid (JPOF). Hystologically, JTOF is characterized by the deposition of minerals leading to the formation of trabeculae of woven bone, while JPOF shows fibrous stroma and spheroidal calcifications called “psammona-like bodies”. The mean age of the trabecular type is usually younger than the psammomatoid (4). A recent systematic review reported a total 143 cases of paranasal JOF, 12 were trabecular and 131 psammomatoid (5), so paranasal JOFs are psammomatoid in most cases. Clinical management do not differ between the two types. Paranasal JPOFs occur more frequently in frontal and ethmoid sinuses, from which it can extent to the orbit and the anterior cranial fossa (4,5). The clinical manifestations are due to the bony expansion, and may include nasal obstruction, facial swelling, proptosis, and headaches. Nonetheless, JPOF are asymptomatic in 96.5% cases (4). When properly treated, the prognosis of paranasal JPOF is good, however a recurrence rate 27.8–56% is reported in literature mainly due to the infiltrative nature of the tumour borders (4,5). The treatment is surgical excision by open, endoscopic, or combined techniques, depending on the location and extension of the pathology (5,6). We report a case of a 13-year-old boy with an ethmoid-maxillary JOF accidentally diagnosed by cranial computerized tomography (CT) and successfully treated by sinus endoscopic surgery. This case report was prepared following the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-22-90/rc) (7).
Case presentation
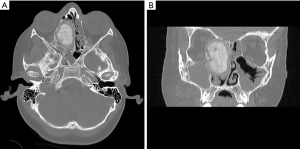
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent for publication of this case report and accompanying images was not obtained from the patient or the relatives after all possible attempts were made to contact them, and the article has been sufficiently anonymized to cause no harm to the patient or his family. We present the case of a 13-year-old Caucasian male transferred to the emergency room of Bambino Gesù Children’s Hospital from another hospital due to accidental facial trauma, after which maxillofacial CT was performed. The clinical history revealed that the patient had been suffering from a nasal obstruction for several months. He was in good health before the onset of the obstruction, with unremarkable medical, surgical, and family histories. The CT showed an expansive bony mass originating from the right ethmoid that expanded into the ipsilateral nasal cavity, the orbit, and the maxillary sinus (Figure 1). He was hospitalized and a magnetic resonance imaging (MRI) was performed to define the mass more fully and to clarify the involvement of the surrounding soft tissues, particularly the orbit. MRI excluded any intracranial and orbital complications.
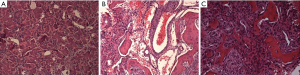
Among the possible differential diagnoses, a giant osteoma or ossifying fibroma appeared to be the most compatible; histological typing was therefore considered necessary. The neoformation was biopsied under general anaesthesia with endoscopic control by 0° optics; the histological examination definitively confirmed a juvenile ossifying fibroma of the psammomatoid subtype (Figure 2). At the periphery of the lesion, the ossicles were fused and formed bone trabeculae showing numerous reversal lines (Figure 2B). Spherical small ossicles called psammonma-like bodies were founded in the sample examined (Figure 2A). There was focal pseudocystic haemorrhagic degeneration bordered by multinucleated giant cells similar to an aneurysmal bone cyst (Figure 2C).
A few days later, the patient underwent endoscopic surgery to remove the lesion. After infiltrating the lining mucosa, the mass was evacuated; the inside of the lesion appeared fibrous. The middle turbinate was removed, and the cleavage plane was collected from the nasal septum, after which the capsule delimiting the neoformation was excised, but, as a precaution, left in place in its lateral component in direct continuity with the papyrus lamina, which manifested signs of wear. No post-operative complications occurred. The patients did not complain any discomfort after the procedure.
One month after surgery, the first control CT scan showed residue of the “shell” of the lesion at the level of the right orbital region. The patient’s clinical conditions were stable and nasal endoscopic controls were normal.
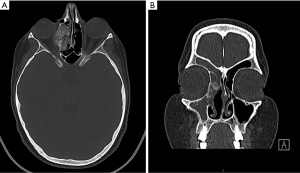
The patient was stable up to the second postoperative month, until he experienced a headache and underwent an emergency CT which revealed an increase in the volume of the residual “shell” with convexity on the medial profile of the right orbit (Figure 3).
The patient was therefore hospitalized and underwent revision surgery with complete removal of the bone wall (newly formed “shell”) laterally towards the orbit until Tenon’s capsule was discovered, and up to the roof of the ethmoid. There were no postoperative complications, with regular recovery and discharge.
Subsequent monthly endoscopic checks together with control CT (10 months after the last surgery) have highlighted the results of previous surgeries, without detecting any further residual disease, but only a minimal plus image of the profile of the medial wall of the orbit was likely reactive in nature (Figure 4).

Thirty-six months after the last surgery, the patient was asymptomatic with negative endoscopic controls for disease recurrence and was clinically stable. The patient is still continuing a regular follow-up, and no recurrence has been observed.
Discussion
JOF of paranasal sinuses is a rare pathology. Endoscopic treatment is accepted as applicable by now, however practical expertise may be not sufficient to guarantee radicality after the first surgery.
In this clinical case, we obtained the patient’s recovery and respected the integrity of the anatomical structures, although a surgical review was necessary.
A literature review revealed that paranasal osteofibrous lesions are often asymptomatic and incidentally diagnosed during investigations for other diseases, such as the head trauma in this case.
Only when the lesion protrudes into the nasal cavity it is possible to identify it endoscopically as a rounded swelling covered with an apparently healthy mucosa (5).
CT is the preferred imaging modality for this type of tumour and allows to distinguish the different subtypes of osteofibrous lesions. The ossifying fibroma often appears as a mass with a well-defined edge, unlike fibrous dyplasia (FD), a disturbance of bone metabolism resulting in bone replacement with fibrous connective tissue. Radiologically the ossifying fibroma does not resemble a ground-glass opacity but has a mixed density between compact bone and fibrous tissue (8). In lesions of this type, MRI may help to evaluate the surrounding soft tissue involved, but a preoperative biopsy is always recommended in order to differentiate between the malignant forms (9,10). In addition to FD, other several pathologies should be taken into account in differential diagnosis: osteoblastoma, osteosarcoma, primary aneurysmal bone cyst, intraosseus cavernous hemangioma and eosinophilic granuloma. In doubtful cases, histological diagnosis may be performed with immunohistochemistry (5).
Open surgery (craniofacial resection) has been the gold standard of treatment of ossifying fibromas so far (11). This approach may still be valid for removing frontal sinus osteomas, which are the most frequent (about 57% of paranasal localization) and the most difficult to completely eradicate transnasally (12,13). Endoscopic techniques offer an optimal approach in all the other localization (ethmoidal, sphenoidal, and maxillary sinus) and also in frontal sinus when reachable through the ostium (14,15).
Recent studies have shown that with the advancement of endoscopic techniques, in expert hands, complete excision is possible by ESS in the majority of cases (13-16). Direct visualization of the anatomical structures avoids damage to surrounding structures. A real time CT navigation equipment can be used to guide surgeons in much safe and effective endoscopic procedures (12). The ESS allows a decidedly less invasive approach, which may be especially preferred in pediatric patients with still immature bony structures (13-16). In case of intracranial or orbital involvement, an external or combined approach is necessary for better control of the operative field, avoiding complications and reducing the risk of recurrence (17,18). The JOFs have an infiltrative behavior and incomplete excision on the tumour border causes relapses. Some Author suggests radical, en bloc resection in case of aggressive, rapid growing JOF, but a very extensive mass would require major demolitive surgery (18-20). This aspect in the case of benign tumor in childhood should be carefully evaluated. There are no effective medical therapies, because it is still unclear if the etiology is osteogenic (due to multipotential mesenchymal cells of the periodontal ligament), traumatic, or infective (20). Nonetheless, some author experienced a protocol for aggressive JOF, consisting in surgical removal in combination with adjuvant interferon-alpha therapy (20,21). In both open and endoscopic surgery, enucleation should be followed by the curettage or osteotomy of the apparently healthy bone tissue neat the margins of the tumour.
Conclusions
In the present case, a non-radical excision of the JOF led to a short-term relapse, confirming that complete excision of this type of lesion is essential for resolution. The endoscopic approach, therefore, should be the technique of choice, given the excellent access to the paranasal sinuses, greater preservation of the anatomical structures, the best postoperative course, and best functional and aesthetic results for a patient of developmental age. Further studies will provide more data about interferon therapy, in combination with endoscopic surgery, to avoid recurrences and demolition surgery, and to obtain radicality while conserving anatomical structures and function in young patients.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-22-90/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-22-90/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-22-90/coif). The authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Menzel A. A failed case of osteofibroma of the corpus mandible. Arch Klin Chir 1892;13:212.
- Mohsenifar Z, Nouhi S, Abbas FM, et al. Ossifying fibroma of the ethmoid sinus: Report of a rare case and review of literature. J Res Med Sci 2011;16:841-7. [PubMed]
- Eller R, Sillers M. Common fibro-osseous lesions of the paranasal sinuses. Otolaryngol Clin North Am 2006;39:585-600. x. [Crossref] [PubMed]
- Chrcanovic BR, Gomez RS. Juvenile ossifying fibroma of the jaws and paranasal sinuses: a systematic review of the cases reported in the literature. Int J Oral Maxillofac Surg 2020;49:28-37. [Crossref] [PubMed]
- Radzki D, Szade J, Nowicki T, et al. Juvenile psammomatoid ossifying fibroma. Pol J Pathol 2021;72:277-81. [Crossref] [PubMed]
- Al Arfaj D, Almomen A, Bakri M, et al. Aggressive juvenile ossifying fibroma of the ethmoid sinus with orbital and intracranial extension: A case report. Int J Surg Case Rep 2022;96:107255. [Crossref] [PubMed]
- Riley DS, Barber MS, Kienle GS, et al. CARE guidelines for case reports: explanation and elaboration document. J Clin Epidemiol 2017;89:218-35. [Crossref] [PubMed]
- Sontakke SA, Karjodkar FR, Umarji HR. Computed tomographic features of fibrous dysplasia of maxillofacial region. Imaging Sci Dent 2011;41:23-8. [Crossref] [PubMed]
- Nair SN, Kini R, Rao PK, et al. Fibrous Dysplasia versus Juvenile Ossifying Fibroma: A Dilemma. Case Rep Dent 2016;2016:6439026. [Crossref] [PubMed]
- Efune G, Perez CL, Tong L, et al. Paranasal sinus and skull base fibro-osseous lesions: when is biopsy indicated for diagnosis? Int Forum Allergy Rhinol 2012;2:160-5. [Crossref] [PubMed]
- Lund VJ, Howard DJ, Wei WI, et al. Craniofacial resection for tumors of the nasal cavity and paranasal sinuses--a 17-year experience. Head Neck 1998;20:97-105. [Crossref] [PubMed]
- Kim DY, Lee OH, Choi GC, et al. A Case of Juvenile Psammomatoid Ossifying Fibroma on Skull Base. J Craniofac Surg 2018;29:e497-9. [Crossref] [PubMed]
- Castelnuovo P, Valentini V, Giovannetti F, et al. Osteomas of the maxillofacial district: endoscopic surgery versus open surgery. J Craniofac Surg 2008;19:1446-52. [Crossref] [PubMed]
- Pagella F, Pusateri A, Matti E, et al. Transnasal endoscopic approach to symptomatic sinonasal osteomas. Am J Rhinol Allergy 2012;26:335-9. [Crossref] [PubMed]
- London SD, Schlosser RJ, Gross CW. Endoscopic management of benign sinonasal tumors: a decade of experience. Am J Rhinol 2002;16:221-7. [Crossref] [PubMed]
- Wang H, Sun X, Liu Q, et al. Endoscopic resection of sinonasal ossifying fibroma: 31 cases report at an institution. Eur Arch Otorhinolaryngol 2014;271:2975-82. [Crossref] [PubMed]
- Savastano M, Guarda-Nardini L, Marioni G, et al. The bicoronal approach for the treatment of a large frontal sinus osteoma. A technical note. Am J Otolaryngol 2007;28:427-9. [Crossref] [PubMed]
- Turri-Zanoni M, Dallan I, Terranova P, et al. Frontoethmoidal and intraorbital osteomas: exploring the limits of endoscopic approach. Arch Otolaryngol Head Neck Surg 2012;138:498-504. [Crossref] [PubMed]
- Peterson BR, Nelson BL. Juvenile Active Ossifying Fibroma. Head Neck Pathol 2015;9:384-6. [Crossref] [PubMed]
- Troulis MJ, Williams WB, Kaban LB. Staged protocol for resection, skeletal reconstruction, and oral rehabilitation of children with jaw tumors. J Oral Maxillofac Surg 2004;62:335-43. [Crossref] [PubMed]
- Kelly PR. Interferon Alpha Therapy for Aggressive Juvenile Ossifying Fibroma. J Oral Maxillofac Surg 2008;66:76-7. [Crossref]
Cite this article as: Panatta ML, De Vincentiis M, Marini G, Santarsiero S, Sitzia E. Juvenile psammomatoid ossifying fibroma of the ethmoid sinus successfully treated by endoscopic sinus surgery: a case report. AME Case Rep 2023;7:16.


