Incorporating transitional palliative care in a bone marrow transplant unit by serious illness conversation: a case report
Highlight box
Key findings
• Complex psychosocial needs in transplant patients.
• Integrated palliative model is important for transition by serious illness conversation.
• Coping improved and grief largely resolved.
What is known and what is new?
• Serious illness conversation is already useful for advanced cancer patients.
• Hereby, we presented its use in bone marrow transplant patient for transition to palliative care in Hong Kong.
What is the implication and what should change now?
• Early palliative care engagement would be important for her smooth transition to hospice by serious illness conversation.
Introduction
Transplant professionals are specialized in providing lifesaving organs to patients in whom organ failure including bone marrow, in a way that gives strong hope to patients and families (1). We should be aware of that patients with advanced medical conditions must have an advanced care planning (ACP) in place, though it is difficult to balance possible outcomes and hope (2-4). ACP is a discussion on how a patient wants decisions to be handled when they can no longer be mentally competent for themselves. This kind of document outlines their delegate for specific items including medical procedure, medications, or nutrition issues. ACP is far beyond a do-not-active-resuscitation order, asking upon admission if there is a living will or a physician order for sustainable treatment (4). However, transplant patients usually have difficulty to accept their condition and thus rarely have a chance to discuss their ACP. Hereby, we presented a case of bone marrow transplant (BMT) patient who subsequently had ACP discussion and received palliative care (PC) by our serious illness conversation program (SICP). PC is an approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness (3). We present the following case in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-22-77/rc).
Case presentation
This was a 60-year-old lady, with a diagnosis of myelodysplastic syndrome (MDS) (with RAEB-2 with TP 53 mutation) and acute myeloid leukaemia (AML) transformation, who had BMT in early 2019. Postoperatively, she was complicated by septicemia and mucositis, thus requiring total parenteral nutrition. However, her AML was relapsed, just one month after the BMT. She was found to have grave prognosis because of relapse and worsening medical condition. She was quite worried about her disease status, possible treatments and interventions.
During her stay in haematology unit, she had frequent blood transfusions (both red cells and platelet), episodes of sepsis treated with antibiotics, and regular use of chemotherapy including vidaza and venetoclax, however the disease still did not respond well. Because of persistent symptoms especially ulcer pain and low mood, she was then referred to our PC team for further management. In fact, she could not accept her disease at all, and often questioned her diagnosis and also about the competency of PC team including the central line and other nursing care. On the other hand, she had low self-esteem as she came from mainland China with language barrier, and her previous job was only a security guard. In addition, there was poor social support as she was divorced and had to take care of 2 children (one boy and one daughter). She had no religious belief for spiritual support. Her great distress was related to the long period of treatment and also the prolonged stay in hospital, although she appreciated the efforts from the transplant team. As she was still relatively young, there was strong hope for further disease modifying or novel treatment even her disease had relapsed.
Given the complex nature of BMT patients, our skilled PC nurse launched our SICP, a system-level care delivery approach developed by a group of PC specialists locally in Hong Kong. The SIC Guide provides a framework for clinicians, including doctors, nurses, and other allied health professionals, to examine items that are essential for fully comprehending and respecting the concerns of patients (5). The objective of our SIC is to provide more, better, and sooner dialogues with their clinicians about their goals, values, and priorities, which will shape their future care for every critically ill patient with our transitional PC program (Table 1).
Table 1
| Components |
| Effective communications with parent team and patient about the current disease status, treatment plan and prognosis |
| Stepwise transition to palliative care and hospice by trained staff using serious illness conversation |
| Formulation of goals of care plan aligned with patient values |
| Regular monitor of symptom burden and psychosocial distress by palliative care team |
| Support for families and staff |
| Continuity of care across settings |
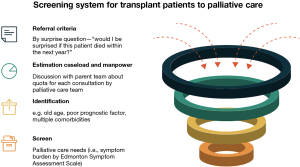
Process of SICP
In our program, the nurse first established good rapport with this patient by several sessions of introduction and briefing. After gaining trust, the nurse then went through all the necessary items including understanding their own diseases, information preferences, treatment plans and exploring psychosocial issues with the patient, one by one, and shared the decision together. Our nurse also assessed the PC needs of this patient and then referred to other appropriate team members including doctor, social worker and clinical psychologist for support. Our PC physician provided on-site symptom management including bone pain, anorexia and pruritus; nurse gave symptom advice and coordination of care, apart from ACP discussion and, social worker had counseling and given support for practical issues (Figure 1). We had joint care with haematology team during PC consultations initially. After assessment and titration of medications, her pain was well controlled with morphine, appetite improved with megestrol acetate while pruritus reduced with pregabalin. The numerical rating of pain and pruritus scores were improved from 7 to 3 and 8 to 2 respectively after one week of PC consultation subsequently. With better understanding of her disease and the nature of PC service, she was then transferred to our unit for more comprehensive care.
Our PC ward had already equipped with those necessary medications and transfusion requirements for caring haematology cancer patients during their end-of-life (EOL) (6,7). As such, supportive transfusion was maintained while the frequency of blood taking was reduced gradually as far as her anaemia symptom was not affected and there was no major bleeding. Her blood count was controlled with short courses of oral chemotherapy. After short period of stay in our unit, she was better adjusted with less focus on regular daily blood taking but more focus on symptom control and quality of life.
Our team nurse, social worker and clinical psychologist continued to provide psychosocial care to this patient. She felt our nurses were skillful in handling BMT patients after 2 weeks stay in our unit. In addition, she could engage herself with online activities including physical exercise, movies, and mahjong. She had adopted the attitude of “achieving victory by hanging on till the end” while holding on to glimmer of hope and miracle happening someday. She could transform ‘hope for cure’ to hope for a ‘better quality of life’ and more short term wishes and goals, like arranging home leave. Instead of asking for disease treatment, she would rather wish to do more exercise as to maintain her physical condition in our ward and, more importantly, hope to join her children marriage if possible. In her last days of life, she finally participated in her daughter marriage because advancement of the event. She was well prepared for the wedding and highly appreciated this occasion as she could finally enjoy the ‘Chinese Bridal Cakes’.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
This case report showed that SICP could successfully transit the BMT patient from transplant unit to PC and subsequently hospice. The core clinical tool of SIC guide is a seven-item structure that assists physicians discuss prognosis and extract key information to support future decision making and care. This includes disease awareness, decision-making choices, objectives and worries, perspectives on trade-offs and functional impairment, and caregiver engagement (8). It was designed by Ariadne Labs as a system-level intervention to enhance communication skills training, coaching, and system modifications that enable the implementation and use of clinical conversation tools. Its goal is to increase the prevalence, timing, and quality of ACP in serious illness (8). In a randomized clinical trial of SIC intervention in advanced cancer patients, behavioral nudges to clinicians and a machine learning-based behavioral intervention increased SICs and decreased EOL systemic therapy, but did not affect other EOL outcomes for cancer outpatients (9). These findings imply that behavioral cues and machine learning can result in long-term enhancements in the provision of cancer care. In another study of SICP for elderly AML and MDS patients (10), it revealed that SICP could give these patients some chances to discuss their values with their care team and may help oncologists match patient care to patient values. SIC also applied to individuals with end stage renal failures who are receiving dialysis may be open to clinician-led structured serious illness talks. Future discussions with dialysis patients about major illnesses can be guided by the themes found (11).
It has been observed in patients with advanced haematological malignancies are more likely to receive intensive treatments near the EOL and are less commonly referred to PC programs than those with solid tumours (7). The implementation of PC interventions into malignant hematology/BMT unit is more challenging due to issues with the emerging novel treatments and a lack of understanding between patients’ families and healthcare professionals regarding disease trajectory and prognosis. This will be more complicated in transplant patients when dealing their EOL issues (12).
In fact, she had grave prognosis and suffered from significant symptoms. However, she could not accept when first knowing her diagnosis of relapse, thus unable for any ACP discussion nor to transfer to hospice care. The next question is how to bridge the service gap for transplant patients and break the communication barriers, before having ACP for this group of patients. In the first step, we must have to set up an appropriate setting for better communication in SIC. Physicians may not have adequate time to prepare BMT patients and their families to meet so that they can explain their medical condition and make plans for the future due to a variety of factors (e.g., hectic work schedules, lack of training). Families and their friends would be able to formulate questions and attend a meeting if permission was granted and a meeting was arranged in beforehand. In addition, it could convey an important and serious message to them. This kind of model will be the initial way of working as collaborative partnership that emphasizes the relationship among the hematologist, PC team and patients with their families to build common understanding and trust (5).
Physicians are sometimes unable to introduce the difficult discussions like poor prognosis and EOL issues (13). However, some of them might refer their patient and families to PC given that they understand this service is beneficial (14). In our case, the haematologist had affirmed the patient/families’ concern that the worsening symptom burden may be related to the disease progression. The patient was also sought for consent before the haematologist introduced the PC team to help with treatment, especially with pain and symptom management, ACP, and communication-related difficulties.
During the joint meeting with PC team, haematologist and patient/family, it is important to gauge the patient understanding of the own disease status and the current management, particularly in the changes in the medical condition or in the face of difficult news (13). It would go beyond acknowledging the patient/family in regard to the patient condition; it sets the backbone and look for (I) the feelings of the patients/families; (II) their concerns and (III) the accuracy of their information. In this situation, the patient and her family had taken into account the information the hematologist had given at the time of the relapse. Recognizing the severity of the recurrence, they carefully observed the patient’s reaction to treatment, any change in symptoms, or behavior. This would also give opportunities to express their worries regarding the relapsed disease while still hoping the haematological cancer to be cured.
In a complex and continuing process, mutual communication plays a crucial role in assessing understanding (15). If there are major symptoms or they struggle with acceptance, this can be addressed in a joint meeting. By asking more questions, the haematology team will learn significant facts to share with the patient and other medical teams.
It is essential to determine how much information the patient and his or her family want to know about medical conditions, particularly the prognosis, and how much information they receive. Giving short, concise, and honest information to patients/families would be useful (14). SIC usually consist of words that patients might find useful, such as prognosis, uncertainty or change in symptoms (15). When adapting the guide for BMT patients, this will give a structural and smoother approach for the transition of these patients to PC team and subsequently to hospice. The transition PC model would provide the care needs including change of patient symptom burden and psychosocial care support.
There is a misperception that if patients or families are offered a poor prognosis and advised to begin ACP, they will lose hope (2). Even in the face of a major illness, individuals typically still maintain their faith, and sharing facts does not impair their sense of hope (14). The clinician (in-charge of SIC) may respond to their feelings by listening. In order to conform with the patient’s hope, accept their fears, and then move forward together, the SIC guide suggests the clinician to adopt their wish, worry, and wonder approach (5).
Improving both patient and family psychosocial care would be important (16). Exploration of their concerns will assist clinicians grasp what people are thinking and provide a platform for support. A coordinated care that can respond quickly and plans for foreseeable anxieties and concerns could also lessen the sense of helplessness and alienation experienced by patients and their families.
Because these BMT patients usually stayed in hematology unit during their EOL care, in-patient PC consultation would provide timely and effective on-site symptom control and psychosocial care (17). Apart from these, the transfusion requirement and some of the medications (e.g., chemotherapy) indicated for BMT patients would be continued even stepping down to PC ward. Thus, the medication knowledge including the adverse reactions of these medications including chemotherapy or target therapy (Table 2) should be known to PC team with proper training and education. It is gratifying to observe that this patient benefited from PC treatment in various ways, including her symptoms improving, emotional stability, muscle power being preserved, and hope being restored since she longed to attend her daughter’s wedding. In this case, SIC can be regarded as a tool to facilitate better communication and so lead to faster and smoother transition to PC and subsequently hospice care. The use of chemotherapy (e.g., vidaza) also had important palliative roles including for symptom control, maintaining patient’s mobility and quality of life (18). This case report is limited by inadequate assessment of physical, mental, and spiritual aspects of patients. More detailed and structural assessment of using SIC is necessary in the future (19).
Table 2
| Adverse events | Azacitidine | Venetoclax | Carfilzomib | Lenalidomide | Melphalan | Cyclophosphamide | Vorinostat | Elotuzumab | Steroid |
|---|---|---|---|---|---|---|---|---|---|
| Anaemia | x | x | x | x | x | x | x | x | |
| Neutropenia | x | x | x | x | x | x | x | x | |
| fatigue | x | x | x | ||||||
| Nausea | x | x | x | x | x | x | x | ||
| Diarrhea | x | x | x | x | x | x | x | x | |
| Constipation | x | ||||||||
| Pain (abdominal) | x | ||||||||
| Hyperglycemia | x | x | x | ||||||
| Rash | x | x | x | ||||||
| Edema | x | x | x | x | |||||
| Mood disorder | x |
Conclusions
This case report showed that the BMT patient had difficulty in accepting the relapse of her haematological disease, with the main focus on disease treatment and blood parameters initially. SIC with early PC engagement would be important for her smooth transition to hospice. Despite her condition being gradually deteriorated, her grief could be largely resolved as most of the wishes fulfilled.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-22-77/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-22-77/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Periyakoil VS, Neri E, Fong A, et al. Do unto others: doctors' personal end-of-life resuscitation preferences and their attitudes toward advance directives. PLoS One 2014;9:e98246. [Crossref] [PubMed]
- Halpern SD, Loewenstein G, Volpp KG, et al. Default options in advance directives influence how patients set goals for end-of-life care. Health Aff (Millwood) 2013;32:408-17. [Crossref] [PubMed]
- Chung RY, Wong EL, Kiang N, et al. Knowledge, Attitudes, and Preferences of Advance Decisions, End-of-Life Care, and Place of Care and Death in Hong Kong. A Population-Based Telephone Survey of 1067 Adults. J Am Med Dir Assoc 2017;18:367.e19-27. [Crossref] [PubMed]
- Chan KY, Chiu HY, Yap DYH, et al. Impact of structured advance care planning program on patients' wish items and healthcare utilization. Ann Palliat Med 2021;10:1421-30. [Crossref] [PubMed]
- van Breemen C, Johnston J, Carwana M, et al. Serious Illness Conversations in Pediatrics: A Case Review. Children (Basel) 2020;7:102. [Crossref] [PubMed]
- Chan KY, Gill H, Chan TSY, et al. Early integrated palliative care for haematology cancer patients-the impact on symptom burden in Hong Kong. Ann Palliat Med 2021;10:6316-24. [Crossref] [PubMed]
- Chan KY, Gill HSH, Chan TSY, et al. Impact of integrated palliative care in acute and aggressive medical care for patients with advanced haematological malignancies: a retrospective matched case-control study. Lancet Oncol 2022;23:S10. [Crossref]
- Bernacki R, Hutchings M, Vick J, et al. Development of the Serious Illness Care Program: a randomised controlled trial of a palliative care communication intervention. BMJ Open 2015;5:e009032. [Crossref] [PubMed]
- Manz CR, Zhang Y, Chen K, et al. Long-term Effect of Machine Learning-Triggered Behavioral Nudges on Serious Illness Conversations and End-of-Life Outcomes Among Patients With Cancer: A Randomized Clinical Trial. JAMA Oncol 2023;9:414-8. [Crossref] [PubMed]
- Locastro M, Sanapala C, Mendler JH, et al. Adaptation of Serious Illness Care Program to be Delivered via Telehealth for Older Patients with Hematologic Malignancy. Blood Adv 2022;bloodadvances.2022008996.
- Mandel EI, Maloney FL, Pertsch NJ, et al. A Pilot Study of the Serious Illness Conversation Guide in a Dialysis Clinic. Am J Hosp Palliat Care 2023; Epub ahead of print. [Crossref] [PubMed]
- Scully BB, Nolley EP, Bush EL. Palliative care in lung transplantation. Ann Palliat Med 2022;11:927-35. [Crossref] [PubMed]
- Sanders JJ, Curtis JR, Tulsky JA. Achieving Goal-Concordant Care: A Conceptual Model and Approach to Measuring Serious Illness Communication and Its Impact. J Palliat Med 2018;21:S17-27. [Crossref] [PubMed]
- Bernacki RE, Block SDAmerican College of Physicians High Value Care Task Force. Communication about serious illness care goals: a review and synthesis of best practices. JAMA Intern Med 2014;174:1994-2003. [Crossref] [PubMed]
- Fleuren N, Depla MFIA, Janssen DJA, et al. Underlying goals of advance care planning (ACP): a qualitative analysis of the literature. BMC Palliat Care 2020;19:27. [Crossref] [PubMed]
- Chan KY, Yip T, Yap DY, et al. Enhanced Psychosocial Support for Caregiver Burden for Patients With Chronic Kidney Failure Choosing Not to Be Treated by Dialysis or Transplantation: A Pilot Randomized Controlled Trial. Am J Kidney Dis 2016;67:585-92. [Crossref] [PubMed]
- Ciemins EL, Blum L, Nunley M, et al. The economic and clinical impact of an inpatient palliative care consultation service: a multifaceted approach. J Palliat Med 2007;10:1347-55. [Crossref] [PubMed]
- Detmar SB, Muller MJ, Schornagel JH, et al. Role of health-related quality of life in palliative chemotherapy treatment decisions. J Clin Oncol 2002;20:1056-62. [Crossref] [PubMed]
- Chan KY, Gill HSH, Yap DYH. Addressing inequity in access to palliative care for patients with non-malignant or benign haematological diseases. Lancet Haematol 2022;9:e473-4. [Crossref] [PubMed]
Cite this article as: Tsang KW, Au HY, Sim JPY, Wong CY, Chan KY. Incorporating transitional palliative care in a bone marrow transplant unit by serious illness conversation: a case report. AME Case Rep 2023;7:20.