
Cross-circulation thrombectomy for acute middle cerebral artery occlusion through a posterior communicating artery: a case report
Highlight box
Key findings
• Cross-circulation stroke treatment may be beneficial in cases with chronic occlusion or complex vascular anatomies.
What is known and what is new?
• Two concurrent of acute large vessel occlusion in two circulation systems is rare and associated with poor clinical outcomes.
• Cross-circulation treatment may be beneficial in cases with ipsilateral chronic occlusions or anatomical constraints.
What is the implication, and what should change now?
• Evaluation the cerebral collateral before revascularization in chronic occlusion.
• Initial diagnostic angiography and digital subtraction angiography are important to select the appropriate approach to lesion.
Introduction
The efficacy of endovascular treatments for acute ischemic stroke has been substantiated by several recent randomized clinical trials, and endovascular intervention received the strongest level I recommendation in recent American Heart Association/American Stroke Association guidelines (1,2). However, complex vascular anatomy and chronic lesions involving extracranial or intracranial vessels may make classical anterograde approaches through parent vessels challenging. Cross-circulation approaches, in which the primary catheterization of a target artery occurs from the contralateral side or the opposite cerebral circulation, can provide alternative pathways to allow for successful recanalization in difficult cases. It helped save time, enhance the efficiency, and improve the clinical prognosis of the patient. However, cross-circulation approaches are also associated with potential risks, such as long procedure times (puncture to recanalization), hemorrhagic complications, and thromboembolic events in unaffected arterial territories (2-5). We report a clinical case of acute ischemic stroke in two simultaneous circulation systems due to the occlusion of intracranial arteries that was resolved by a cross-circulation mechanical thrombectomy procedure. We present this case in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-22-80/rc).
Case presentation
Patient information
A 67-year-old woman with a history of uncontrolled hypertension, dyslipidemia, type 2 diabetes mellitus, and coronary artery disease without any prior neurological history presented to the emergency department within 3 hours of developing stupor, dysphasia, and weakness of the left side.
Clinical findings
The patient was stuporous, with a Glasgow coma scale (GCS) score of 9. The patient’s vital signs were stable, including blood pressure of 160/90 mmHg and a regular heart rate. Examination revealed Broca’s aphasia, left hemiparesis (muscle strength =1/5), left hemidysesthesia, central facial palsy, and equally round pupils reactive to light. The National Institute of Health Stroke Scale (NIHSS) score was 20, and no abnormalities were identified in any other organs by the relevant clinical, para-clinical and laboratory findings.
Diagnostic assessment
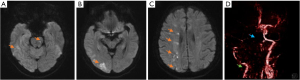
Brain magnetic resonance imaging (MRI) and magnetic resonance angiography showed multiple infarctions in the basilar artery, right posterior cerebral artery, and right middle cerebral artery (MCA) territories, and occlusions of the right internal carotid artery and basilar artery (Figure 1).
Electrocardiogram (ECG) showed a regular sinus rhythm of 100 beats per minute.
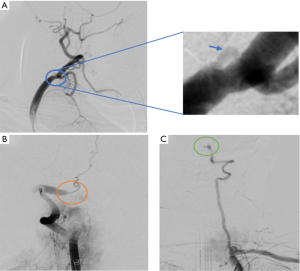
The patient was taken to the angio-suite to receive an angiogram and endovascular intervention. The angiogram revealed a carotid stump at the right carotid (6), a hypoplastic left vertebral artery with V4 segment occlusion, and an acute occlusion of the V4 segment of the right vertebral artery (Figure 2).
Therapeutic interventions
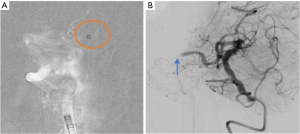
A Neuron Max 088 guide catheter (Penumbra Inc., Alameda, CA, USA) was placed in the V2 segment of the right vertebral artery. Through the guide catheter, we inserted a coaxial system consisting of a Sofia Plus aspiration catheter (Microvention), a Headway 21 microcatheter (Microvention Inc., Aliso Viejo, CA, USA), and a Hybrid014D microwire (Balt, Montmorency, France) to approach the vertebrobasilar artery thrombosis. The Sofia Plus aspiration catheter was connected to a 50-mL syringe to apply negative pressure two times. The follow-up angiogram revealed the complete recanalization of the vertebrobasilar artery, but the occlusion of the right MCA-M1 segment was observed (Figure 3).
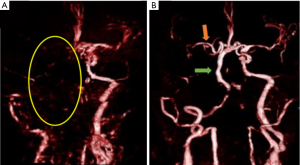
Using a coaxial system consisting of a Sofia Pus aspiration catheter, a Headway 21 microcatheter, and a Hybrid014D microwire, the right posterior communicating artery (PCoA) (2.1 mm diameter) was used to approach the right MCA-M3 segment. A CatchV35 stent (Balt) was introduced through the microcatheter and fully deployed across the occluded right MCA. Within 5 minutes of stent placement, the Sofia Plus aspiration catheter was advanced to the proximal M1 segment of the right MCA and connected to the suction system. The stent and microcatheter were slowly pulled back with the Sofia Plus, and then the coaxial system was completely withdrawn from the patient’s body through the 8F guide catheter. A large red thrombus was retrieved with a single pass. The follow-up angiogram revealed the complete recanalization of the vertebrobasilar artery and the right MCA, assessed as thrombolysis in cerebral infarction (TICI) stage III (Figure 4). The detailed time intervals from symptoms onset to successful recanalization were mentioned in Table 1.

Table 1
| Actual time of treatment (military time) | Time intervals |
|---|---|
| Symptom onset—09:00 | Door to neurologist—0 minute |
| Arrival at the ED—12:00 | Door to MRI first slice—26 minutes |
| Head MRI—12:26 | Door to groin puncture—80 minutes |
| Arrival at the INR—13:05 | Door to recanalization—160 minutes |
| Groin puncture—13:20 | Symptom onset to recanalization—340 minutes |
| Recanalization—14:40 |
ED, emergency department; MRI, magnetic resonance imaging; INR, interventional neuroradiologist.
Follow-up and outcome
At 24 hours after the intervention, head MRI showed the complete recanalization of the vertebrobasilar artery and right MCA artery, with no evidence of embolization in any new territories (Figure 5).
At discharge, 10 days after stroke onset, the patient’s symptoms improved, with a GCS score of 15. The patient continued to display dysarthria, left facial droop, and weakness of the left side (muscle strength 3/5), with an NIHSS score of 10.
At the 3-month follow-up, the patient displayed near-complete recovery, with mild left facial droop, muscle strength on the left side of 4/5, an NIHSS score of 4, and a modified Rankin Scale score of 2.
All procedures performed in this study were in accordance with the ethical standards of the institutional and national research committees and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
In our case report, the patient presented with chronic occlusion of the right internal carotid artery and acute occlusion of the right vertebrobasilar artery. Infarctions in the right MCA can be caused by a thrombus released from an occluded vertebrobasilar artery that blocks the right MCA; atherosclerotic plaque detached from the occluded internal carotid artery stump that blocks the right MCA; or hemodynamic insufficiency caused by a chronic carotid occlusion resulting in poor collateral supply.
We decided to revascularize the vertebrobasilar artery because untreated obstructions of the vertebrobasilar arteries are associated with a mortality rate greater than 80% (7). After the complete recanalization of the vertebrobasilar artery, we noted the continued occlusion of the right MCA. We had to choose between an anterograde endovascular approach through the chronic right carotid occlusion or a cross-circulation approach through the right PCoA.
We examined the PCoA and found that it had a diameter of 2.1 mm, making it suitable for the passage of the clot retriever system consisting of the Sofia Plus aspiration catheter, the Headway 21 microcatheter, and the CatchV35 stent retriever. Therefore, approaching the right MCA through the PCoA would save time, enhance efficiency, and improve the clinical prognosis of the patient but having some potential risk such as hemorrhagic or thromboembolic complications. A cross-circulation thrombectomy was performed successfully with no complications and good outcomes.
The pooled review of 12 studies describing 23 trans-circulation thrombectomy cases identified the most common occlusion locations as MCA occlusions in tandem with internal carotid artery occlusions (69.6%) and mid basilar artery occlusions in tandem with bilateral vertebral artery occlusions (17.4%). The anterior communicating artery and PCoA were used in the treatment approaches for 12 (52.2%) and 10 (43.5%) cases, respectively, and one patient required a combined approach. Available follow-up data included 20 clinical and 18 radiographic assessments. After a mean follow-up of 4.1 months, 18 of 20 (90%) patients achieved favorable functional outcomes (modified Rankin Scores of 0–2), and 13 of these 18 (72.2%) cases experienced successful recanalization (4).
A number of authors have reported their experiences with posterior-to-anterior circulation thrombectomy. Hui et al. described the first reported posterior-to-anterior circulation approach for the thrombectomy of a right MCA thrombus using the Penumbra system (8). Kim et al. presented the first case of a posterior-to-anterior circulation right MCA thrombectomy using a stent Trevo XP retriever (Stryker Corporation, Kalamazoo, MI, USA) (9). However, these approaches have some potential risks such as the long procedure time (puncture to recanalization) and hemorrhagic complications or thromboembolic events in unaffected arterial territories, so cross-circulation thrombectomy is only performed when anterograde approach fail or is not possible. In our case, we performed a posterior-to-anterior circulation thrombectomy using the Solumbra technique. In addition, no reports have described the use of a CatchV35 stent retriever in a cross-circulation thrombectomy approach.
Conclusions
Cross-circulation treatment may be beneficial in cases with ipsilateral chronic occlusions or anatomical constraints. Newly developed microwires, microcatheters, and clot-retrieval devices have allowed improvements in the recanalization rates with decreased complications. Larger studies remain necessary to evaluate the safety and efficacy of this approach.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-22-80/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-22-80/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and national research committees and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2019;50:e344-418. [Crossref] [PubMed]
- Chung Y, Bae Y, Hong CE, et al. Hyperattenuations on flat-panel computed tomography after successful recanalization of mechanical thrombectomy for anterior circulation occlusion. Quant Imaging Med Surg 2022;12:1051-62. [Crossref] [PubMed]
- Gill HL, Siracuse JJ, Parrack IK, et al. Complications of the endovascular management of acute ischemic stroke. Vasc Health Risk Manag 2014;10:675-81. [Crossref] [PubMed]
- Roa JA, Maud A, Jabbour P, et al. Transcirculation Approach for Mechanical Thrombectomy in Acute Ischemic Stroke: A Multicenter Study and Review of the Literature. Front Neurol 2020;11:347. [Crossref] [PubMed]
- Roa JA, Ortega-Gutierrez S, Martinez-Galdamez M, et al. Transcirculation Approach for Endovascular Embolization of Intracranial Aneurysms, Arteriovenous Malformations, and Dural Fistulas: A Multicenter Study. World Neurosurg 2020;134:e1015-27. [Crossref] [PubMed]
- Myrcha P, Gloviczki P. A systematic review of endovascular treatment for chronic total occlusion of the internal carotid artery. Ann Transl Med 2021;9:1203. [Crossref] [PubMed]
- Nouh A, Remke J, Ruland S. Ischemic posterior circulation stroke: a review of anatomy, clinical presentations, diagnosis, and current management. Front Neurol 2014;5:30. [Crossref] [PubMed]
- Hui FK, Narayanan S, Cawley CM. Posterior-to-anterior circulation access using the Penumbra Stroke System for mechanical thrombectomy of a right middle cerebral artery thrombus. World Neurosurg 2010;73:17-21. [Crossref] [PubMed]
- Kim SK, Baek BH, Heo TW, et al. Successful Cross-circulation Stent-Retriever Embolectomy Through Posterior Communicating Artery for Acute MCA Occlusion by Using Trevo XP ProVue. Neurointervention 2016;11:55-8. [Crossref] [PubMed]
Cite this article as: Linh DH, Cuong TC, Giang NL, Thang LM, Duc NM. Cross-circulation thrombectomy for acute middle cerebral artery occlusion through a posterior communicating artery: a case report. AME Case Rep 2023;7:27.


