
Rupture of thymoma due to recurrent tumor hemorrhage: a case report
Highlight box
Key findings
• This report describes a case wherein recurrent hemorrhage of the tumor resulted in the rupture of a thymoma.
What is known and what is new?
• Mediastinal tumors are usually discovered incidentally on chest radiography. However, rupture of a thymoma is rare.
• The pathological findings revealed the mechanism of the rupture of the tumor. An increase in the intratumoral pressure due to recurrent hemorrhaging and weakening and thinning of the tumor wall due to chronic inflammation and necrosis may have resulted in the rupture.
What is the implication, and what should change now?
• The intratumoral pressure increased due to recurrent and repeated hemorrhaging within the tumor. In addition, chronic inflammation and necrosis weakened the tumor wall. These changes contributed to the subsequent rupture of the thymoma.
Introduction
A thymoma is the most common anterior mediastinal tumor in adults, accounting for 20% of all anterior mediastinal tumors (1). The tumors are usually diagnosed incidentally on chest radiographs. Rupture of a thymoma is rare, and due to its rarity, the mechanism of rupture is unclear. Here we report a case of thymoma that ruptured due to an increase in the intratumoral pressure caused by recurrent hemorrhaging within the tumor. We present this case in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-23-44/rc).
Case presentation
A 70-year-old woman presented 2 days prior persistent right chest and shoulder pain. She had a history of hypertension. The respiratory status was stable. Enhanced computed tomography (CT) of the chest revealed the presence of a mass occupying the anterior mediastinum and a right pleural effusion. The interior of the tumor was unenhanced and partially hyper-absorbed, exhibiting necrosis and hemorrhaging. The pleural effusion Hounsfield unit (HU) was 40, suggesting hemorrhaging within the tumor (Figure 1). Hematological examinations revealed neutrophilic leukocytosis and elevated C-reactive protein levels. The carbohydrate antigen-125 (CA-125) and cytokeratin 19 fragment (CYFRA) levels were elevated, and the alpha-fetoprotein (AFP), human chronic gonadotropin (hCG), and anti-acetylcholine receptor antibody levels were within the normal range. Judging from the frequency at that time, the mass was diagnosed as an anterior mediastinum tumor, in particular, a ruptured/bleeding teratoma. The elevated levels of inflammatory markers and the presence of tumor necrosis on CT were suggestive of infection. Therefore, as the general status of the patient was stable and she initially received antibiotic therapy, an improvement in the inflammatory marker levels was observed with antibiotic therapy.

A surgical resection was performed 10 days after admission. The patient was placed in a dorsal position under general anesthesia. Median sternotomy revealed a tumor extending from the mediastinum to the right thoracic cavity. A bloody pleural effusion was confirmed. Since the adhesion was strong and tumor invasion was suspected, the tumor was completely resected by combining a partial resection of the right middle and lower lobes with the pericardium. Although the pleural fluid was not collected intraoperatively for cytological examinations, we judged that a gross R0 resection was achieved.
No complications occurred postoperatively and the patient was discharged from the hospital on postoperative day 14. The patient was followed up without any adjuvant therapy and has remained recurrence-free for 1 year postoperatively.
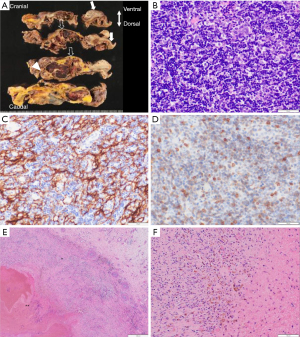
Grossly, the tumor was a 65 mm × 60 mm × 30 mm mass that contained blood clot and necrotic material with extensive adhesion to the resected lung. Microscopically, it comprised a thymoma and a thymic cyst. Hematoxylin-eosin staining revealed thick cyst walls with fibrosis, necrosis, hemosiderosis, and hemorrhaging. These findings suggested that recurrent hemorrhaging and inflammation had occurred within the tumor.
The solid components of the tumor comprised epithelial cells that had proliferated mixed with lymphocytes. The epithelial component had a highlighted mesh-pattern by cytokeratin AE1-AE3 immunostaining. These findings were suggestive of a type B2 thymoma. No tumor cells were observed in the resected lung or pericardium. The pathological diagnosis was a type B2 thymoma (World Health Organization 2020 classification), Masaoka Stage II, pT2N0M0 Stage II (Union for International Cancer Control eighth edition) (Figure 2).
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Mediastinal tumors are usually asymptomatic tumors that are discovered incidentally on chest radiographs (2). Rupture of teratoma occurs rarely (3). A rupture of a thymoma is extremely rare. According to previous case reports, most patients with ruptures thymoma experience sudden chest pain or dyspnea (4,5), accompanied by bleeding from the tumor and demonstrated a hemothorax. That was induced and required an emergency surgical resection (6,7).
In the present case, the patient presented with sudden-onset of right chest and shoulder pain. The high HU on CT and intraoperative right bloody pleural effusion suggested bleeding and rupture of the tumor. Since infection of the tumor was suspected, antibiotic therapy was initiated first. An elective surgery instead of emergent surgery was performed as the general status of the patient was stable.
Chest radiography revealed that the right pleural effusion had not increased over time, indicating that the hemorrhaging was temporary and hemostasis had been achieved. The pathological findings revealed the mechanism of the rupture of the tumor. Hemorrhaging, fibrosis, necrosis and hemosiderosis were observed within the tumor.
Based on these findings, we hypothesized that the following factors may have contributed to the rupture. First, recurrent hemorrhaging and inflammation had occurred within the tumor, resulting in fibrosis and hemosiderosis during the chronic phase. Consequently, the intratumoral pressure may have increased, which could have been the main cause of the thymoma rupture. Second, chronic inflammation and necrosis may have led to weakening of the surrounding wall and cyst wall, resulting in the rupture of the thymoma. In present case, part of the tumor consisted of the cyst wall which may easily rupture under the circumstances of hemorrhage or inflammation (8).
The reasons for the rupture of thymoma remain obscure due to its rarity.
According to the previous studies, an enlargement of the thymoma (6) and intratumoral hemorrhaging (9) were possible factors for the rupture of thymoma. In the present case, recurrent hemorrhaging and inflammation and necrosis were considered to have contributed to the rupture of the thymoma.
Our case report presents the mechanism of the rupture of thymoma from pathological findings.
Conclusions
We here reported a case of ruptured thymoma. Based on the findings of our case, it can be considered that the recurrent and repeated hemorrhaging of the tumor may have increased the intratumoral pressure and chronic inflammation and necrosis weakened tumor wall. These changes contributed to the subsequent rupture.
Acknowledgments
We thank Dr. John Martin for his proofreading. We would like to thank Editage for English language editing.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-23-44/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-23-44/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-23-44/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Thomas CR, Wright CD, Loehrer PJ. Thymoma: state of the art. J Clin Oncol 1999;17:2280-9. [Crossref] [PubMed]
- Strollo DC, Rosado de Christenson ML, Jett JR. Primary mediastinal tumors. Part 1: tumors of the anterior mediastinum. Chest 1997;112:511-22. [Crossref] [PubMed]
- Tavares JG, Baptista B, Gonçalves B, et al. Mediastinum Teratoma Rupture: A Rare Manifestation. Eur J Case Rep Intern Med 2019;6:001022. [Crossref] [PubMed]
- Sinyagovskiy P, Abdalla M, Raja A, et al. Spontaneous rupture of thymoma. Respir Med Case Rep 2019;26:56-8. [Crossref] [PubMed]
- Templeton PA, Vainright JR, Rodriguez A, et al. Mediastinal tumors presenting as spontaneous hemothorax, simulating aortic dissection. Chest 1988;93:828-30. [Crossref] [PubMed]
- Santoprete S, Ragusa M, Urbani M, et al. Shock induced by spontaneous rupture of a giant thymoma. Ann Thorac Surg 2007;83:1526-8. [Crossref] [PubMed]
- Hokka D, Ogawa H, Tane S, et al. Ruptured thymoma causing a hemothorax: A case report. Oncol Lett 2015;10:1810-2. [Crossref] [PubMed]
- Tsuda K, Yoshida I, Ohshima K, et al. Ruptured thymic cysts with mediastinal hemorrhage and hemothorax--a case report and reviews of the literature. Nihon Kyobu Geka Gakkai Zasshi 1997;45:1654-9.
- Fukuse T, Matsukura T, Nakamura A, et al. Mediastinal hematoma due to thymoma hemorrhage--a case report. Nihon Kyobu Geka Gakkai Zasshi 1991;39:930-4.
Cite this article as: Uebayashi A, Ema T, Oiwa H, Yasuda K, Matsubara O, Funai K. Rupture of thymoma due to recurrent tumor hemorrhage: a case report. AME Case Rep 2023;7:23.


