
Retention hyperkeratosis over surgical scar: case report and review of literature
Highlight box
Key findings
• RHK is associated with poor hygiene as we have seen in our patient’s case, it could be prevented by providing
What is known and what is new?
• Manual removal of the hyperkeratotic lesion through trimming and clipping the excess layer of skin is effective method used in management of hyperkeratotic report here about what this manuscript adds.
What is the implication, and what should change now?
• RHK should be more reported.
Introduction
Retention hyperkeratosis (RHK) is a common dermatosis that could be categorized under the big umbrella of hyperkeratosis. It could be simply defined as keratin build-up over the most superficial layer of the skin with no clarified etiology till now but it has been correlated with certain dysfunction in keratinocytes cell cycle that is affected by multiple factors in which we will discuss in this case report of patient who had developed RHK over surgical scar (1-5). Typically, RHK is a mild, benign skin disorder. Our patient developed RHK because of lack of mechanical friction secondary to hir fear of touching his surgical area. This hypothesis is supported by the lack of hyperkeratosis on other parts of his body. Our primary differential diagnosis upon examining the patient included seborrheic keratosis (SK) and viral wart which were ruled out after obtaining full medical history from the patient. We present this article in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-23-28/rc).
Case presentation
A 63-year-old man who has been known to have hypertension, dyslipidemia, ischemic heart disease, and a history of coronary artery bypass surgery presented to our dermatology clinic with an asymptomatic skin lesion over the linear midline sternotomy scar post-coronary artery bypass grafting (post-CABG) that he underwent 8 years ago. A complete skin exam revealed no similar lesions elsewhere. The patient’s history was significant of avoiding touching or cleaning the area as he feared disturbing the healing process of his surgical wound. Thus, due to lack of surgical scar care, a thick layer of skin was formed and described as brown hyperkeratotic plaque. Otherwise, his general hygiene was good. Examination revealed yellow/brownish hyperkeratotic papules coalescing into larger, well-demarcated plaques (Figure 1).
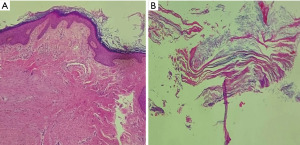
For further investigation, a 4 mm punch biopsy was taken to confirm diagnosis of RHK and rule out other differential diagnoses. Microscopic examination showed extensive hyperkeratosis along with mild acanthosis and dermal fibrosis/scar. There were no evidence of HPV changes, dysplasia or malignancy (Figure 2A,2B).
Based on the clinical picture and supported biopsy findings, the diagnosis of RHK was made.
Treatment and follow-up: the patient chose to have his hyperkeratotic lesion removed manually, which went smoothly as wet gauze with a scalpel blade were used, then it was scrapped with a scraper. The lesion was very soft upon removal and no issues were faced during the process (Figure 3).

Patient was educated and reassured throughout the time he was following up in clinic as to prevent recurrence of hyperkeratotic lesion over his surgical scar again.
This study protocol was reviewed and approved by the IRB Committee at the research center of Prince Sultan Military Medical City (No. 112023). All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Hyperkeratosis could be divided according to its etiology as in hereditary types of hyperkeratosis such as epidermolytic hyperkeratosis or site specific hyperkeratosis like focal acral hyperkeratosis and other non-classified types as well like corn and calluses (1). Hyperkeratosis also can be seen in common dermatosis such as lichen planus and chronic eczema (1).
Throughout the clinical examination of the patient and based on the observation of the morphology of the hyperkeratotic lesion of the patient, SK and common warts were suggested as differential diagnosis along with RHK. SK is a common noncancerous skin condition in elderly that could present in form of tan or brownish papule or plaque which is similar to our patient’s presentation (2). Common warts or viral warts are described as small verrucous or papillomatous lesions (3), even though it might be less likely in this case due to the size and the shape of the lesion; yet it was not rule out completely at first which were ruled out after taking full history. All previously suggested conditions were considered to be different causes of hyperkeratosis (1).
RHK is a common benign skin condition seen by dermatologists frequently, yet a limited number of cases have been reported up to this day. On cellular level for normal skin growth, keratinocytes differentiate from the deepest layer of epidermis (stratum basale) to the most superficial one (stratum corneum) which considered to be the protective layer of the skin (4). Stratum corneum is mostly composed of terminally differentiated keratinocytes, also known as corneocytes (5). In healthy functional skin, corneocytes are shed in regular matter through biological and mechanical factors as part of skin cell turnover (5). As our patient has not been known to have any previous hyperkeratotic lesion throughout his life nor has the same lesion anywhere else other than over his surgical scar, we thought the development of RHK was caused by dysfunctional skin cell turnover would most likely be due to lack of mechanical friction as he feared touching his surgical scar over the previous eight years. A case reported in 2010 by Harris et al. of a patient presenting with RHK over her face to have had similarly developed it due to poor hygiene out of fear of touching her face after being diagnosed with a rare autoimmune endotheliopathy known as Susac syndrome (6).
Hyperkeratosis management differs depending on type, severity, and chronicity. Topical keratolytics containing urea, tretinoin or other ingredients along with emollients is a gold standard method used in most cases of hyperkeratosis. Topical therapy can be accompanied by lifestyle modifications regarding diet or daily habits. Also, manual removal of the hyperkeratotic lesion through trimming and clipping the excess layer of skin is also a common method used in management of hyperkeratosis as we have done with our patient which have cleared it completely in one session (1).
Conclusions
As RHK is one of the most benign skin conditions which is easily manageable by dermatologists that can mimic SK and warts, however, since it is significantly associated with poor hygiene as we have seen in our patient’s case, it could have been prevented by instructing the patient regarding his wound care post-operatively as to not let his fear impact him on the long-term. Our case represents a rare extreme manifestation related to the fear of our patient to clean surgical wounds.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-23-28/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-23-28/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-23-28/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study protocol was reviewed and approved by the IRB Committee at research center of Prince Sultan Military Medical City (No. 112023). All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Elwell R. The management and treatment of hyperkeratosis. Br J Nurs 2017;26:468-70. [Crossref] [PubMed]
- Greco MJ, Bhutta BS. Seborrheic Keratosis. 2023 Feb 9. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2023.
- Witchey DJ, Witchey NB, Roth-Kauffman MM, et al. Plantar Warts: Epidemiology, Pathophysiology, and Clinical Management. J Am Osteopath Assoc 2018;118:92-105. [Crossref] [PubMed]
- Bolognia JL, Jorizzo JL, Rapini RP, et al. Dermatology. 2nd ed. Elsevier, 2008.
- Pierard GE, Goffin V, Hermanns-Le T, et al. Corneocyte desquamation. Int J Mol Med 2000;6:217-21. [PubMed]
- Harris K, Pho LN, Bowen AR. Severe retention hyperkeratosis occurring with Susac syndrome. Dermatol Online J 2010;16:8. [Crossref] [PubMed]
Cite this article as: Alkhayal FA, Alyousef LA. Retention hyperkeratosis over surgical scar: case report and review of literature. AME Case Rep 2023;7:34.



