
Prurigo pigmentosa post-bariatric surgery: a case report
Highlight box
Key findings
• Prurigo pigmentosa (PP) presented as a pruritic papulovesicular rash on the abdomen, chest, and back 3 weeks following bariatric surgery.
• The rash resolved after treatment with minocycline.
• There was no history of ketogenic diet consumption.
What is known and what is new?
• There is an association between PP and the consumption of a ketogenic diet.
• This case suggests another association with bariatric surgery.
What is the implication and what should change now?
• Awareness should be raised among physicians, gastroenterologists specifically, regarding the association between PP and bariatric surgery.
• More research is needed to fully understand the pathophysiology behind PP and its association with bariatric surgery.
Introduction
Prurigo pigmentosa (PP) is an inflammatory skin condition that was first described by Nagashima in 1971 (1). The presentation of the disease depends on the staging. The first stage of the disease is characterized by urticarial papules and plaques that form a gross reticular pattern (2). The pathological hallmark of this stage is a perivascular infiltrate of polymorphonuclear cells (2-4). In the next stage of the disease, vesicles appear and the rash becomes papulovesicular in nature (2). Pathologically, this stage is characterized by spongiosis and necrotic keratinocytes (2-4). The third and last stage of the disease exhibits pigmented macules in a reticular configuration (2). The histologic manifestations of the late stage are a lymphocytic infiltrate and melanophages in the papillary dermis (2-4). The rash usually resolves with post-inflammatory hyperpigmentation. The condition usually affects the trunk, the neck, and the chest. The disease was initially thought to be limited to people of Asian descent (particularly Japanese); however, recent cases are emerging from all around the world. There is evident female gender predominance in reported cases. PP has been strongly associated with ketosis. Conditions and circumstances that may result in ketosis have also been reported. Such instances include ketogenic diet, primary biliary cirrhosis, and bariatric surgery (2,5-9). The definitive pathogenesis and etiology are unknown; however, a proposed theory suggests that PP is a reactive inflammatory condition involving bacterial folliculitis (10). The first line treatment for PP is minocycline. Other treatment options include macrolides, doxycycline, and dapsone (2). We present this case in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-23-45/rc).
Case presentation
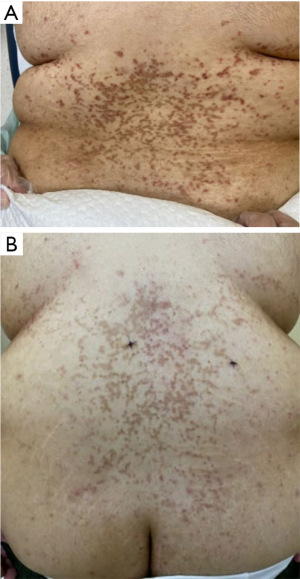
A 25-year-old ethnically Saudi morbidly obese male patient with history of irritable bowel syndrome (IBS) presented to our dermatology clinic at King Fahad Medical City in Riyadh 21 days after undergoing elective bariatric surgery complaining of a new onset rash that has been present for the last 3 days. The rash appeared 18 days after the surgery and was pruritic in nature. Upon further questioning, the patient denied adherence to a ketogenic diet and stated that the only form of medication he had been receiving was occasional Gabapentin as needed for his IBS. On examination, multiple erythematous papulovesicles in a reticular configuration were observed over the trunk, upper abdomen, and chest (Figure 1A,1B). The differential diagnoses at that time included PP and drug induced eruption.

Two punch skin biopsies were obtained from the lumbar back during the visit, and the patient was started on topical clobetasol propionate ointment and 80 mg of modified release oral minocycline. Pathologically, punch skin biopsies showed focal interface reaction and scattered necrotic keratinocytes (Figure 2A). Hair follicles were dilated and filled with bacteria (Figure 2B,2C), and a mildly acanthotic dermis was observed. Perivascular lymphocytes, eosinophils, and extravasated red blood cells were also noted in the superficial dermis (Figure 2D). There was no evidence of intraepidermal neutrophilic infiltrate.

The patient presented for his follow up appointment 2 weeks after the initial visit with complete resolution of the rash. He reported adherence to the medication regimen and resolution of pruritus. Upon examination, post-inflammatory hyperpigmentation in a reticular pattern was observed over the trunk, upper abdomen, and chest (Figures 3,4). Hydroquinone 4% cream was prescribed to treat the post-inflammatory hyperpigmentation.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
PP, or Nagashima disease, is an erythematous papulovesicular inflammatory dermatosis that classically appears following a period of ketosis. Most cases of PP present following dietary modifications, with the “keto diet” being the most notorious to cause PP. It has also been linked to systemic conditions such as Helicobacter pylori (H. pylori) infection (11), Still’s disease (12), Sjögren’s syndrome (5), and atopy (13). The rash usually manifests as pruritic papules and plaques that form a reticular pattern overlying the back, the chest, and the abdomen. After the initial discovery of the disease in Japan in 1971, new cases were being reported strictly in Japan and the disease was thought to be limited to those of Japanese ancestry. Nowadays, PP cases are being reported from all around the world, including cases of PP that appeared following bariatric surgery for weight loss without ketogenic dietary modification. As of 2021, 369 patients with an established diagnosis of PP have been identified from 24 different countries (14). To our knowledge, only 4 cases of PP have been reported following bariatric surgery (6-9). All four cases were females aged 40 or younger. In most cases, the rash resolved after consumption of a balanced diet.
It is not uncommon for patients to enter a state of ketosis following bariatric surgery (7). Thus, the presence of a pruritic eruption after bariatric surgery in our case warranted the use of punch biopsies. Even though the patient did not adhere to a specific diet; the physiological inability to consume a well-balanced diet during the early post-operative course following bariatric surgery could have predisposed him to ketosis. A genetic predisposition involving an increased expression of ICAM-1 and HLA-DR4 has been reported in some cases (13). However, such testing has not been performed in our case. The pruritus in PP can be very severe, and in some cases, it can be resistant to topical corticosteroid therapy and oral antihistamine therapy. This can serve as a diagnostic clue (15). Empiric antibiotic treatment with an oral tetracycline such as minocycline or dapsone is indicated in such cases to control the symptoms and treat possible folliculitis (2,10). Minocycline monotherapy is the most commonly prescribed form of treatment (14). However, the classic treatment involves an antibiotic in addition to cessation of ketogenic diet or resolution of ketosis, which usually results in successful resolution of the rash. In some cases, a balanced diet and cessation of a ketogenic diet can result in the resolution of the rash without the use of an antibiotic (3). In our case, we believe that both the antibiotic treatment as well as the gradual improvement in the patient’s diet resulted in the resolution of the rash. A study involving 32 patients with PP showed that 66% of subjects had evidence of bacterial colonies in hair follicles upon microscopic examination, which was present in our patient as well (10). The presence of necrotic keratinocytes on our patient’s biopsy indicates that the disease was in its second stage prior to treatment. The resolution with hyperpigmentation correlates with the late stage of the disease during which melanophages are present in the papillary dermis (2). Hydroquinone remains the mainstay treatment for post-inflammatory hyperpigmentation (16).
Patient perspective
Not knowing what was causing the rash was stressful for me. I felt relieved after learning about the condition, and even more relieved after the itchiness stopped, and the rash was gone. I am happy with the result, and I experienced no side effects. This journey motivated me to maintain a balanced diet.
Conclusions
Theoretically, the typical PP patient is a young adult female from Eastern Asia who has been adherent to a ketogenic diet. In contrast, we report a case of a Saudi male who did no dietary modifications, but underwent bariatric surgery. Treatment with minocycline resulted in successful complete resolution.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-23-45/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-23-45/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-23-45/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. The identity of the patient has been kept anonymous and photos of the patient did not include any identifying details. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Nagashima M. A peculiar pruriginous dermatosis with gross reticular pigmentation. Jpn J Dermatol 1971;81:38-9.
- Beutler BD, Cohen PR, Lee RA. Prurigo Pigmentosa: Literature Review. Am J Clin Dermatol 2015;16:533-43. [Crossref] [PubMed]
- Wong M, Lee E, Wu Y, et al. Treatment of Prurigo Pigmentosa with Diet Modification: A Medical Case Study. Hawaii J Med Public Health 2018;77:114-7. [PubMed]
- Oh YJ, Lee MH. Prurigo pigmentosa: a clinicopathologic study of 16 cases. J Eur Acad Dermatol Venereol 2012;26:1149-53. [Crossref] [PubMed]
- Togawa Y, Shinkai H, Utani A. Prurigo pigmentosa in a patient with primary biliary cirrhosis and Sjögren syndrome. J Dermatol 2004;31:815-9. [Crossref] [PubMed]
- Al-Dawsari NA, Al-Essa A, Shahab R, et al. Prurigo pigmentosa following laparoscopic gastric sleeve. Dermatol Online J 2019;25:13030/qt2b20c2w8.
- Alkhouri F, Alkhouri S, Potts GA. Prurigo Pigmentosa Following a Keto Diet and Bariatric Surgery. Cureus 2022;14:e24307. [Crossref] [PubMed]
- Alsebayel MM, Ghobara YA, Al-Issa A. Facial Prurigo Pigmentosa After Bariatric Surgery. Cureus 2020;12:e6909. [PubMed]
- Abbass M, Abiad F, Abbas O. Prurigo Pigmentosa After Bariatric Surgery. JAMA Dermatol 2015;151:796-7. [Crossref] [PubMed]
- Kafle SU, Swe SM, Hsiao PF, et al. Folliculitis in prurigo pigmentosa: a proposed pathogenesis based on clinical and pathological observation. J Cutan Pathol 2017;44:20-7. [Crossref] [PubMed]
- Erbagci Z. Prurigo pigmentosa in association with Helicobacter pylori infection in a Caucasian Turkish woman. Acta Derm Venereol 2002;82:302-3. [Crossref] [PubMed]
- Muthalaly AS, Bradish J, Sampson R, et al. Prurigo pigmentosa as an atypical persistent plaque-like skin rash in adult-onset Still's disease: Case report and literature review. Int J Clin Rheumtol 2013;8:521. [Crossref]
- Cota C, Donati P, Amantea A. Prurigo pigmentosa associated with an atopic diathesis in a 13-year-old girl. Pediatr Dermatol 2007;24:277-9. [Crossref] [PubMed]
- Mufti A, Mirali S, Abduelmula A, et al. Clinical manifestations and treatment outcomes in prurigo pigmentosa (Nagashima disease): A systematic review of the literature. JAAD Int 2021;3:79-87. [Crossref] [PubMed]
- Aerts O, Dendooven E, Siozopoulou V. Dieting Resulting in Prurigo Pigmentosa ("Keto Rash"). J Allergy Clin Immunol Pract 2021;9:4149-50. [Crossref] [PubMed]
- Davis EC, Callender VD. Postinflammatory hyperpigmentation: a review of the epidemiology, clinical features, and treatment options in skin of color. J Clin Aesthet Dermatol 2010;3:20-31. [PubMed]
Cite this article as: Jazzar Y, Shadid AM, Beidas T, Aldosari BM, Alhumidi A. Prurigo pigmentosa post-bariatric surgery: a case report. AME Case Rep 2023;7:43.



