
Lesson of urgent bilateral lobar lung transplantation for acute fibrinous and organizing pneumonia: a case report
Highlight box
Key findings
• Urgent bilateral lobar lung transplantation is feasible for acute fibrinous and organizing pneumonia (AFOP).
What is known and what is new?
• AFOP is commonly treated by medicine. Lung transplantation has been employed for acute respiratory distress syndrome (ARDS) including AFOP;
• Bilateral lobar lung transplantation can be applied for AFOP.
What is the implication, and what should change now?
• Urgent bilateral lobar lung transplantation may be an alternative for ARDS. This case offers a rationale for improving criteria of lung transplantation in future, especially for ARDS.
Introduction
Acute fibrinous and organizing pneumonia (AFOP) is a histopathologic pattern characterized by the formation of intra-alveolar plugs of the fibrin deposition (1). AFOP is considered a composite of diffuse alveolar damage, cryptogenic organizing pneumonia, and eosinophilic pneumonia (2), and is classified into acute and subacute types. Its occurrence is rare, mainly reported in the US and China (3-6). The dominant symptoms are respiratory insufficiency, cough, and fever. AFOP is related to an idiopathic cause or autoimmune disease, drug use, infection, cancer, or transplantation (6). Existing data did not report the correlation between AFOP and demographics. According to the American Thoracic Society and the European Respiratory Society, AFOP is highly likely to be diagnosed by a non-surgical approach followed by a surgical biopsy (7). However, there is a lack of consensus on treatment for AFOP.
Urgent lung transplantation for AFOP has been reported as an alternative treatment for selected patients (8,9). No evidence shows that lobar lung transplantation is applied in an urgent situation such as AFOP.
Therefore, we present our lesson in treating a young female patient with AFOP by urgent lobar lung transplantation. We present this case in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-22-88/rc).
Case presentation
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
A 33-year-old female patient reported fever, cough, and dyspnoea four days before admission without any comorbidity. After admission, hypoxemia happened and needed high-flow nasal cannula therapy with empiric antimicrobial therapy [steroids (methylprednisolone 1.5 mg/kg/day) and broad-spectrum antibiotics]. Processed pulmonary consolidation in the left upper lobe was considered with regard to computed tomography scan. Moreover, percutaneous lung biopsies of the left upper lobe were taken. Histologically, the alveolar spaces were filled with fibrin balls and fibroblastic tissue without hyaline membranes and eosinophils. Therefore, AFOP can be diagnosed (10), and she was transferred to the intensive care unit (ICU). The patient received broad-spectrum antibiotics, high-dose steroids (methylprednisolone 10 mg/kg/day), and high-dose immunoglobulins (2 g/kg/5 days). Subsequently, respiratory failure occurred with required orotracheal intubation and mechanical ventilation (MV). Invasive ventilation cannot significantly improve respiratory insufficiency. In addition, echocardiography showed normal biventricular function with no valve, septal defects, and pulmonary hypertension. However, she worsened and was referred to venovenous (V-V) extracorporeal membrane oxygenation (ECMO) support. Plus, the “lung rest approach” in MV was set.
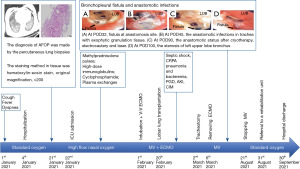
However, pulmonary function did not improve within 2-week protective MV strategies with V-V ECMO support. We thus threw out a multidisciplinary team (MDT) discussion with the lung transplantation group in our institution. The patient was referred to the lung transplant emergency waiting list once informed consent was obtained. On the 20th day of the ECMO application, a donor lung was achieved from a female brain-dead patient due to trauma, who had 165 cm of height and 78 kg of weight without smoking cession. Bilateral lobar lung transplantation (including left upper lobe, right upper lobe, and right middle lobe) was thus the best choice since the size of donor lung was larger than the receiver chest. The clamshell incision was used with the V-V ECMO. Tacrolimus and methylprednisolone were applied in induction therapy. Main post-transplantation complications included carbapenem-resistant Pseudomonas aeruginosa pneumonia, exophytic granulation tissue with inflammation, anastomotic stenosis in the trachea (nearly sealing the airway), bronchopleural fistulae (happened on post-transplantation day 32), anastomotic infections in the trachea, septic shock, bacteraemia, reperfusion syndrome, primary graft dysfunction [grade 3 (11)], severe renal failure with dialysis and critical illness myopathy. The patient condition after transplantation deteriorated rapidly in the short term. Hence, timely aggressive broad-spectrum therapy was referred based on the results of the microbiological examination. Additionally, prophylactic antifungal and antiviral therapy was applied, as well as renal replacement therapy for renal failure. Regarding the occurrence of inflammation and, subsequently, fistulae in the area of the left bronchial anastomosis, we applied percutaneous drainage and airway debridement (cryotherapy, electrocautery, and laser to remove granulation tissue, and bronchoscopic balloon dilatation). The patient remained under immunosuppression and respiratory rehabilitation. Eventually, we weaned ECMO on the post-transplantation 14th day and MV on the post-transplantation 6th month. Furthermore, we conducted the tracheostomy for this patient on the post-transplantation 12th day. The patient was discharged from the general thoracic surgery unit in a month.
The specific patient trajectory is shown in Figure 1.
Within over 1 year follow-up, the patient is survival without readmissions due to any relevant complications and returns to normal daily life and social activity.
Discussion
AFOP was first reported in 2002 by Beasley (1). It always leads to morbidities mainly related to respiratory failure, thereby introducing multiple organic dysfunction and death. Present treatments are proposed to reduce respiratory function injury for patients with AFOP. However, the outcomes of these treatments may be unsatisfiable. To our case report, urgent lobar lung transplantation may be an alternative strategy for curing AFOP.
Systematic and comprehensive literature searching was conducted in MEDLINE by terms “lung transplantation” and “acute fibrinous and organizing pneumonia”. Only two case-report articles have reported that lung transplantation can be applied in the treatment of AFOP. In 2015, Renaud-Picard and colleagues presented that a young male patient with AFOP following double lung transplantation (1st) for cystic fibrosis was successfully rescued by an emergency bilateral lung transplantation (2nd) (9). AFOP can be considered a novel form of chronic lung allograft dysfunction as previous reports (1), but lung transplantation may be available to treat this morbidity. In 2020, Campisi and colleagues added two cases of evidence of the possible benefits of urgent lung transplantation for AFOP (8). Within 1 year of follow-up, these two patients live well with optimal graft function and no sign of rejection in lung function tests and radiological examination. Similarly, we reported that urgent lobar lung transplantation could be indicated to a female adult with AFOP based on a MDT (including clinicians from the department of thoracic surgery, respiratory, neurology, anaesthesia, nurse, ICU, and rehabilitation).
Our centre commences lung transplantation early but does not perform it routinely. So, this case is interesting but challenging for us, especially for treating complications after transplantation. Regarding our other impressive lessons, the acute syndrome “AFOP” resulting in respiratory failure can be classified as a form of acute respiratory distress syndrome (ARDS). Urgent transplantation for ARDS has been identified (12-14). ARDS during the coronavirus disease 2019 (COVID-19) pandemic became even more a new indication for transplantation in well-selected patients. It is very important to select the best cases. Although lung transplantation is a key treatment option for patients with certain well-defined chronic end-stage lung diseases, there is not any consensus about its application for patients with AFOP. Especially, our case was a healthy person without any comorbidity before admission. In addition, patients with no urgent lung transplantation should have good airway management without prolonged use of palliative, paralytic, glucocorticoid and ECMO applications, thereby not reducing the incidence of complications and increasing the length of stay. Therefore, in the future, we need to consider several points: (I) what would be the treatment strategies for AFOP? (II) When is the best time for patients with AFOP to undergo urgent lung transplantation? (III) Prolonged ECMO (>14 days) for adult respiratory failure is associated with reduced long-term survival (9). But patients with AFOP must use ECMO. Hence, we should focus more on improving the management of ECMO and MV to improve outcomes.
Additionally, our patient experienced a series of complications during the post-transplantation period. We think it may depend on improving current peri-transplantation treatment, including the technique of pulmonary transplantation, via a multimodal and multidisciplinary approach like an enhanced recovery after surgery recommendations in liver transplantation (15).
Conclusions
The case demonstrates the feasibility of bilateral lobar lung transplantation in patients with AFOP, especially in an urgent situation. But we call for strengthened evidence or clinical practice to confirm its effectiveness.
Acknowledgments
The authors thank Guangzhou Medical University Institution of Respiratory Disease, Clinicians in Sichuan Province Hospital and Organ Procurement Organization in Union Hospital of Fujian Medical University for assistance in patient treatment.
Funding: Funding for Top Hospital and Specialty Excellence of Fujian Province and funding for National Key Clinical Specialty (No. 2919-67) supported all processes of this work.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-22-88/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-22-88/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-22-88/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Beasley MB, Franks TJ, Galvin JR, et al. Acute fibrinous and organizing pneumonia: a histological pattern of lung injury and possible variant of diffuse alveolar damage. Arch Pathol Lab Med 2002;126:1064-70. [Crossref] [PubMed]
- Tzouvelekis A, Koutsopoulos A, Oikonomou A, et al. Acute fibrinous and organising pneumonia: a case report and review of the literature. J Med Case Rep 2009;3:74. [Crossref] [PubMed]
- Garcia BA, Goede T, Mohammed TL. Acute Fibrinous Organizing Pneumonia: A Case Report and Literature Review. Curr Probl Diagn Radiol 2015;44:469-71. [Crossref] [PubMed]
- Arnaud D, Surani Z, Vakil A, et al. Acute Fibrinous and Organizing Pneumonia: A Case Report and Review of the Literature. Am J Case Rep 2017;18:1242-6. [Crossref] [PubMed]
- Ning YJ, Ding PS, Ke ZY, et al. Successful steroid treatment for acute fibrinous and organizing pneumonia: A case report. World J Clin Cases 2018;6:1053-8. [Crossref] [PubMed]
- Lee JH, Yum HK, Jamous F, et al. Diagnostic procedures and clinico-radiological findings of acute fibrinous and organizing pneumonia: a systematic review and pooled analysis. Eur Radiol 2021;31:7283-94. [Crossref] [PubMed]
- Travis WD, Costabel U, Hansell DM, et al. An official American Thoracic Society/European Respiratory Society statement: Update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med 2013;188:733-48. [Crossref] [PubMed]
- Campisi A, Dell'Amore A, Bertolaccini L, et al. Urgent lung transplantation in acute fibrinous and organizing pneumonia: a sliding door or a new perspective? Gen Thorac Cardiovasc Surg 2020;68:136-41. [Crossref] [PubMed]
- Renaud-Picard B, Dégot T, Biondini D, et al. Successful lung retransplantation in a patient with acute fibrinous and organizing pneumonia: a case report. Transplant Proc 2015;47:182-5. [Crossref] [PubMed]
- Gomes R, Padrão E, Dabó H, et al. Acute fibrinous and organizing pneumonia: A report of 13 cases in a tertiary university hospital. Medicine (Baltimore) 2016;95:e4073. [Crossref] [PubMed]
- Morrison MI, Pither TL, Fisher AJ. Pathophysiology and classification of primary graft dysfunction after lung transplantation. J Thorac Dis 2017;9:4084-97. [Crossref] [PubMed]
- Bharat A, Hoetzenecker K. Lung Transplantation for Acute Respiratory Distress Syndrome. Thorac Surg Clin 2022;32:135-42. [Crossref] [PubMed]
- Hoetzenecker K, Schwarz S, Keshavjee S, et al. Lung transplantation for acute respiratory distress syndrome. J Thorac Cardiovasc Surg 2023;165:1596-601. [Crossref] [PubMed]
- Frick AE, Gan CT, Vos R, et al. Lung transplantation for acute respiratory distress syndrome: A multicenter experience. Am J Transplant 2022;22:144-53. [Crossref] [PubMed]
- Brustia R, Monsel A, Skurzak S, et al. Guidelines for Perioperative Care for Liver Transplantation: Enhanced Recovery After Surgery (ERAS) Recommendations. Transplantation 2022;106:552-61. [Crossref] [PubMed]
Cite this article as: Ye B, Chen C, Huang L, Chen J, Weng Q, Wu W. Lesson of urgent bilateral lobar lung transplantation for acute fibrinous and organizing pneumonia: a case report. AME Case Rep 2023;7:44.


