
First case report of ruptured giant expanding breast oil cyst
Highlight box
Key findings
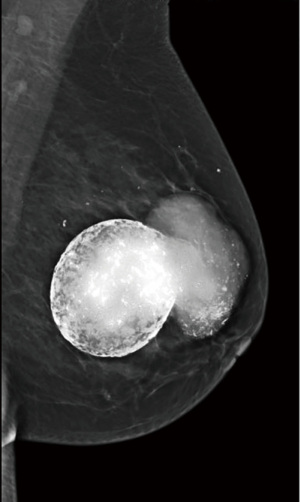
• A peripherally calcified mass with adjacent extruded fatty necrotic material was discovered on mammogram.
• Giant rim calcified oil cyst with single outpouching on a mammogram is a sign of imminent rupture.
What is known and what is new?
• Fat necrosis is commonly seen in breast trauma and sometimes presents as oil cyst. A mammographic appearance of peripherally calcified cystic mass is pathognomonic for fat necrosis.
• The fragile wall of a rare giant oil cyst is susceptible to disruption. Imaging evidence of its imminent and actual rupture is not described in literature.
What is the implication, and what should change now?
• Differential diagnosis of an expanding breast lump should include a ruptured oil cyst.
• Patients with a large oil cyst should be informed about a possibility of cyst rupture and offered a preventative treatment. Fine needle aspiration is the effective treatment for an oil cyst.
Introduction
Background
Breast fat necrosis is a benign inflammatory process of aseptic fat saponification caused by a common trauma or iatrogenic injury to the breast tissue (1). Breast ultrasound and mammography are the primary modalities in diagnosing fat necrosis. Magnetic resonance imaging (MRI) can be utilized for questionable cases of fat necrosis (1,2). Variations in its imaging presentations are attributed to the different stages of the pathogenesis being imaged and the extent of pathological change that occurs during each stage of the process (3,4). The initial hyperacute phase of fat necrosis starts with destruction of adipocytes and damage to the microcirculation which triggers vasoconstriction and leads to fluid transudation. During this stage, ultrasound may reveal increased echogenicity due to edema of breast fat. Subacute phase of fat necrosis is characterized by ongoing destruction of fat cells, decomposition of triglycerides and calcium mediated saponification of fatty acids. Fatty remnants then form vacuoles and are surrounded by lymphocytes and histiocytes which start the reparative process leading to the scar tissue formation. During this day-to-month phase, fat necrosis can present in a variety of forms on imaging. Under the ideal circumstances, a round radiolucent thin-walled mass—an oil cyst—is seen on mammography (4-6). A corollary anechoic cyst with subtle wall nodularity is seen on ultrasound (4-6). On the other end of the spectrum, if there is excessive scarring, the presentation can be more ominous and appear as an irregular spiculated mass with a few interspersed lucent areas on mammogram. The ultrasound morphology can also simulate malignancy since it can present as a solid irregular mass or complex mass with mural nodules or echogenic bands. The majority of mammographic and sonographic presentations is a combination of the aforementioned extreme features of the subacute phase and thus present a great diagnostic challenge requiring a biopsy to exclude malignancy (1,2,7). During the late phase, 1–2 years after fat necrosis started, predominantly peripheral curvilinear stippled calcification develops along with thickened fibrotic wall around cystic masses of disintegrated fat. Posterior shadowing is often seen on ultrasound which may be alarming in the absence of the typical mammographic benign morphology of the oil cyst (5,6). Appearance of the peripherally calcified cystic mass on mammogram is pathognomonic for fat necrosis.
Rationale and knowledge gap
To our best knowledge, rupture of the giant oil cyst has never been reported. Yet, it should be included on the list of differential diagnoses along with hematoma, infection, or neoplasm. When a patient presents with the expanding breast lump, clinicians should be aware of the potential oil cyst rupture and its features. The other important clinical relevance of the case is related to demonstration of the dramatic consequences of not treating the large oil cyst or at least informing the patient of its possible rupture. As a result, presentation of the expanding breast mass posed a diagnostic challenge for us initially since we were unaware of the patient’s history. The patient suffered from anxiety and inconvenience which could have been prevented with a simple and readily available preventative treatment.
Objective
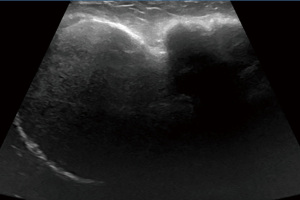
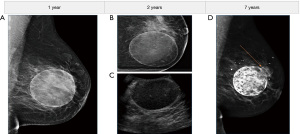
Left breast ultrasound demonstrated a giant, partially visualized, complex avascular mass composed of two interconnected parts: the isoechoic/hypoechoic circumscribed avascular mass with a thick calcified wall and the posterior shadowing which transitioned into the hypoechoic mass with partially circumscribed and partially indistinct margins (Figure 1). This presentation was non-specific. However, demonstration of the peripherally calcified round mass with adjacent extruded necrotic fatty material on the mammogram was pathognomonic for a ruptured giant oil cyst (Figure 2). Subsequently, the prior images revealed a history of one giant oil cyst. A year after the accident, mammogram showed a round lucent mass with thin rim consistent with the early oil cyst (Figure 3A). The subsequent year mammogram redemonstrated stable appearance of the oil cyst (Figure 3B). The same year left breast ultrasound demonstrated an anechoic oval mass with internal echoes, short echogenic bands, and peripheral nodularity keeping with the oil cyst (Figure 3C). A mammogram that was completed 7 years after the accident revealed the mature rim calcified oil cyst measuring approximately 7.0 cm × 6.0 cm × 6.4 cm with the single outpouching with a thin rim (Figure 3D). A present mammogram, approximately 5 years later, revealed the oil cyst rupture which led to the current patient’s presentation. This manuscript is written in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-22-46/rc).
Case presentation
A 51-year-old woman presented to a breast clinic with complaint of the painless left breast lump. She first noticed the lump 12 years ago shortly after the car accident. According to the patient, she suffered some bruises and swelling of her left breast as a consequence of a seatbelt injury. A few weeks after the car accident, the painless lump developed in the patient’s inner left breast. Except for a slight hardening of the breast in the last few years, the lump remained stable until 4 months ago when it began to increase in size. Patient did not complain of pain but was concerned about the growing lump. She was reassured of the benign nature of her condition and explained that the ruptured oil cyst and its extruded content would undergo natural degeneration and evolution within the breast. According to the American Cancer Society, fat necrosis does not increase the risk of breast cancer. The patient was clinically stable without any signs of infection or bleeding and, therefore, did not require an immediate active management or the hospital admission. She did suffer a mild left breast asymmetry and was offered a referral to a cosmetic surgeon for further evaluation and possible correction. The patient, however, elected not to seek a recommended medical care.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Key findings
Demonstration of the pathognomonic features of an oil cyst on the mammogram as a peripherally calcified round mass with adjacent extruded fatty necrotic material was a key finding at the presentation. Finding of the giant rim calcified oil cyst with a single outpouching was crucial in alerting the provider of its imminent rupture.
Strengths and limitations
We encountered the patient for the first time when she had already presented with the ruptured oil cyst. The initial diagnosis of the posttraumatic oil cyst and the following stages of its development were completed at the different facility. As a result, we did not participate in all stages of the patient’s management, diagnosis, and follow-up. Instead we used the prior imaging to retrospectively follow the unique sequelae of fat necrosis. In addition, neither preventative nor restorative/cosmetic management of the giant oil cyst was performed for this patient. These conditions constitute the main limitations of the study. However, we retroactively witnessed and described the natural (although incomplete) course of the giant oil cyst development for the first time. The findings of this case should help clinicians to diagnose and manage the potential complications that may be presented with a case of expanding breast mass. A timely follow-up and well-informed patient are essential to preventative management to avoid the giant cyst rupture.
Comparison with similar research
Fat necrosis and its many presentations, including an oil cyst, have been extensively described in the literature (1-8). Yet, research relative to the giant oil cysts and the complications associated with their presentations is scarce. To that end, we located a single case report that described the giant expanding fat necrosis which presented as an expanding mass (8). The subsequent imaging and biopsy of the fat necrosis revealed the necrosis’ subacute maturation stage of development without calcifications. We, in contrast, witnessed rupture of the giant calcified oil cyst. To our best knowledge, this complication and its presentation have never been reported in the literature and hence preclude a direct comparison to other case studies.
Explanations of findings
The patient in our case presented with an expanding breast lump. In the absence of history of recent trauma and without immediately available prior imaging, this expanding breast lump was unlikely to be caused by fat necrosis. Although not previously reported, possibility of the disruption of the fragile calcified wall of the giant oil cyst seems to be quite likely. Spillage of the necrotic fatty material into the breast tissue after the giant oil cyst rupture was responsible for a dramatic clinical presentation.
Implications and actions needed
Clinicians should be aware of the potential complications of the giant oil cyst and include it into the differential diagnosis of an expanding breast lump. Patients with a large oil cyst should also be informed about a possibility of the cyst’s rupture and suggested the preventative treatment options. A simple fine needle cyst aspiration is the most common and effective treatment of an oil cyst. Surgical excision is reserved for the recurrent cases or when it is cosmetically desirable. When the necrotic fatty tissue spills outside of the cyst, there is no effective management to consider.
Conclusions
Trauma to a woman’s breast can lead to formation of a large oil cyst which can remain present for years, peripherally calcify, and is susceptible to rupture. Clinicians should be aware of this potential complication and include it into the differential diagnosis of an expanding breast lump. Diagnostic mammogram is a study of choice and demonstrates benign pathognomonic features of an oil cyst. Patients with a large oil cyst should be informed about a possibility of the cyst rupture and recommended the preventative treatment options. A simple fine needle aspiration is the most common and effective treatment of an oil cyst.
Acknowledgments
We would like to acknowledge Justin Wei, MD, Department Chair of Radiology, Riverside Community Hospital, for his expert advice and administrative support of the project. We also would like to acknowledge Khrystyna Bednarchyk, EdD, Nova Southeastern University, for her contribution to the manuscript preparation and final format review.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-22-46/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-22-46/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-22-46/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Chan PYL, Wong T, Chau CM, et al. Fat necrosis in the breast: a multimodality imaging review of its natural course with different aetiologies. Clin Radiol 2023;78:323-32. [Crossref] [PubMed]
- Tayyab SJ, Adrada BE, Rauch GM, et al. A pictorial review: multimodality imaging of benign and suspicious features of fat necrosis in the breast. Br J Radiol 2018;91:20180213. [Crossref] [PubMed]
- Ganau S, Tortajada L, Escribano F, et al. The great mimicker: fat necrosis of the breast--magnetic resonance mammography approach. Curr Probl Diagn Radiol 2009;38:189-97. [Crossref] [PubMed]
- Saidian L, Lee SJ, Mahoney MC. Multimodality imaging of fat necrosis of the breast. Contemp Diagn Radiol 2017;40:7-8. [Crossref]
- Hogge JP, Robinson RE, Magnant CM, et al. The mammographic spectrum of fat necrosis of the breast. Radiographics 1995;15:1347-56. [Crossref] [PubMed]
- Soo MS, Kornguth PJ, Hertzberg BS. Fat necrosis in the breast: sonographic features. Radiology 1998;206:261-9. [Crossref] [PubMed]
- Kerridge WD, Kryvenko ON, Thompson A, et al. Fat Necrosis of the Breast: A Pictorial Review of the Mammographic, Ultrasound, CT, and MRI Findings with Histopathologic Correlation. Radiol Res Pract 2015;2015:613139. [Crossref] [PubMed]
- Tuncbilek N, Sezer A, Altaner S, et al. Nontraumatic giant fat necrosis of the breast presenting as a rapidly growing tumor. Prague Med Rep 2011;112:50-5. [PubMed]
Cite this article as: Popovych O, Mousa M, Bhanu S. First case report of ruptured giant expanding breast oil cyst. AME Case Rep 2024;8:3.


