
Ingestion of kinetic sand leading to intussusception and bowel obstruction in a child: a case report
Highlight box
Key findings
• Ingestion of kinetic sand, though marketed as a non-toxic toy, can lead to intussusception, bowel obstruction, bowel necrosis, and bowel perforation.
What is known and what is new?
• Parent information labels state that this product is nontoxic, and packaging displays a choking hazard due to its small parts. Currently, there are no reports on the severity of gastrointestinal distress caused by kinetic sand ingestion.
• We outline the workup and management of the first reported case of bowel obstruction due to small and large bowel intussusceptions caused by ingestion of kinetic sand.
What is the implication, and what should change now?
• Small and large bowel obstructions can lead to life-threatening consequences. This report raises awareness of the side effects of kinetic sand ingestion in hopes of improving marketing content and protecting children in the future.
Introduction
Kinetic sand, also known as magic sand or hydrophobic sand, is marketed as a play sand for children above the age of three years old (1). First referenced in 1915, kinetic sand was originally described as wax-coated sand (1). The modern composition for kinetic sand is 98% ultra-fine sand and 2% polydimethylsiloxane (i.e., silicone oil), which provides its hydrophobic properties (1). This moldable sand comes in play kits with themes that range from construction sites to food kits like ice cream treats, and select sands are scented to complement the theme. While parent information labels state that this product is nontoxic, the packaging displays a choking hazard due to its small parts. Currently, there are no reports on the side effects of kinetic sand ingestion, or the degree of gastrointestinal distress caused by its ingestion. We present the first reported case of kinetic sand ingestion causing bowel obstruction from both small and large bowel intussusception. The goal of this report is to raise awareness to the potential dangers and sequela of ingestion of kinetic sand and to describe the medical management of bowel obstruction secondary to kinetic sand ingestion. We present this case in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-23-37/rc).
Case presentation
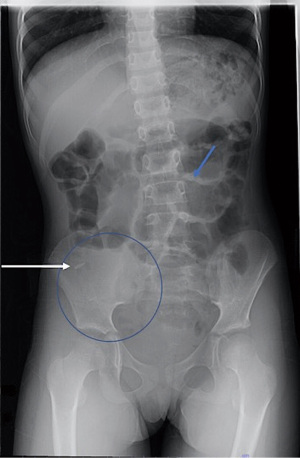
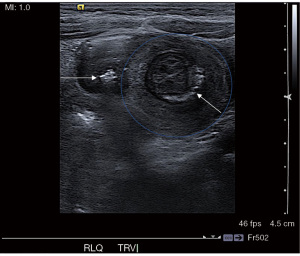
A young girl with a past medical history of autism, trichotillomania, and pica presented to our hospital as a transfer for two days of abdominal pain and non-bloody bilious emesis. Two days prior to presentation, she ingested an unknown quantity of kinetic sand. The following morning, she woke up in distress complaining of generalized abdominal pain. That afternoon, she had four episodes of bilious emesis, prompting presentation to her local emergency department. Initial workup included complete blood count, abdominal X-ray, and abdominal ultrasound (US) with plain films (Figure 1). Initial white cell count was 19.6×109 cells/L. The abdominal US showed an ileocolic intussusception with dense debris—consistent with sand—in the intussuscipiens (Figure 2). The abdominal X-ray showed gas paucity in the right lower quadrant, as expected with the presumed diagnosis of ileocolic intussusception. She was transferred to our facility for further management.
Upon presentation, the patient was afebrile and normotensive. She was not in acute distress and denied nausea or recent emesis but endorsed diffuse abdominal pain with movement. A detailed history was unable to be obtained given the patient’s age; additionally, minimal information was provided by her guardian, so the patient’s last bowel movement was unknown. On physical exam, her abdomen exhibited mild distention with tympany. She had abdominal pain with light and deep palpation without peritoneal signs, such as guarding or pain with gentle shaking of the bed. The remainder of her physical exam was unremarkable, with the exception of right temporal thinning of hair due to reported trichotillomania. After physical exam, she was made nil per os and maintenance intravenous fluids were initiated.
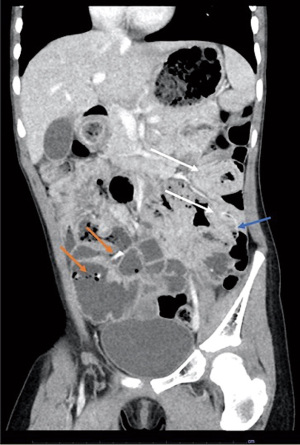
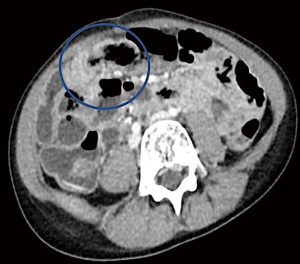
A computed tomography (CT) scan of the abdomen and pelvis with intravenous contrast showed multiple prominent air and fluid-filled bowel loops throughout the abdomen. Findings were concerning for both ileo-ileal, ileo-colonic, and colo-colonic intussusception involving the distal transverse/proximal descending colon (Figures 3,4). Given confirmation on imaging, reduction of the ileo-colic intussusception via fluoroscopic contrast enema was performed. A pediatric rectal tube was inserted and approximately 360 cc of diluted gastrografin was injected directly into the colon by gravity. This study found that the contrast was freely flowing throughout the entire colon with easy reflux into the terminal ileum, indicating successful reduction of a minor ileo-colonic intussusception or spontaneous resolution prior to this procedure (Figure 5).

The patient was admitted and made nil per os. The following day, a supine abdominal X-ray showed opacification of the entire colon with residual contrast of normal caliber consistent with nonobstructive bowel gas pattern. The patient’s abdominal pain continued to improve on physical exam, and her diet slowly advanced. She began to pass flatus and have regular bowel movements. Of note, the initial bowel movements had visible kinetic sand documented by nursing that resolved in 24 hours after reduction enema. After complete clearance of visible kinetic sand in the patient’s stool and continued regular bowel movements, maintenance IV fluid was stopped, and she was deemed stable for discharge on hospital day 2 after initial presentation (Figure 6).

All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient’s legal guardian for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Intussusception is one of the most common causes of intestinal obstruction in infants and young children (2,3). It is described as the invagination of one segment of bowel into an adjacent segment. Our patient was found to have ileo-ileal intussusceptions in addition to an ileo-colonic intussusception. Ileo-ileal intussusceptions in healthy children are common incidental findings on imaging and are typically self-resolving. However, ileo-colonic and colo-colonic intussusceptions are more concerning and typically require intervention. In the pediatric population, the majority of cases are idiopathic and occur between three months and three years of age. The smaller percentage affecting older children is more often linked to a pathologic lead point that is either due to anatomic variations or infectious etiologies (4,5). While diagnostic options include plain films, US, computed sonography, and fluoroscopy (e.g., contrast enema), US has been the gold standard for diagnosis (2,4). Accepted treatment options of ileo-colonic intussusceptions are retrograde hydrostatic or pneumatic enema under fluoroscopic control. Studies have shown that both are adequate interventions for reduction (6,7). The advantage of hydrostatic enemas with contrast is the ability to both diagnose and visualize the reduction post-intervention. Our institution’s protocol outlines use of hydrostatic enema with diluted gastrografin for pediatric patients with ileo-colonic intussusception. While the ileo-ileal intussusceptions were expected to resolve without intervention, the finding of ileo-colonic and colo-colonic intussusceptions warrant intervention.
We report the first case of intussusception and bowel obstruction following kinetic sand ingestion and describe the medical management. Although known in the veterinarian literature that ingestions of sand by dogs can lead to life threatening bowel obstruction, no cases of intestinal obstruction after sand ingestion have been documented in the pediatric literature (8). Kinetic sand is marketed as a non-toxic, moldable, sensory toy. It comes in a range of colors and is often sold in a playset that has a specific theme. While some themes are centered around building sandcastles, there is a subsection of playsets dedicated solely to recreating a variety of snack and dessert options. These food-based playsets are enhanced by scents, such as watermelon, berries, chocolate, vanilla, and strawberry. Like many toys manufactured for children, kinetic sand packaging displays a choking hazard label that warns against ingestion due to small parts for children under three years old. This choking hazard is standard for many children’s toys after the 2008 Consumer Product Safety Improvement Act was passed that required a choking hazard label on any children’s toy that contains small parts, small balls, marbles, and latex balloons (9). Despite the passing of this act, kinetic sand labels do not contain warnings regarding other potentially dangerous consequences of kinetic sand ingestion.
The National Capital Poison Center reports that kinetic sand ingestion can cause constipation and, in severe cases, it is possible to cause gastrointestinal obstruction (10). Instances of the latter have not yet been reported in the literature; however, there is a small collection of case reports covering constipation caused by regular sand in animals (11,12). Our patient developed a symptomatic bowel obstruction caused by intussusception secondary to kinetic sand ingestion. We speculate that the sand affected bowel peristalsis and transiently acted as a pathologic lead point facilitating the telescoping of the bowel in various areas of sand collections. Given the realistic nature of its appearance and smell, we suspect that the large amount of sand ingested contributed to the initial obstruction.
Compared to the general pediatric population, our patient is at higher risk for ingesting of indigestible objects due to her history of pica. However, in our opinion, the realistic appearance and scent of this product puts also neurodevelopmentally unchallenged children at risk for ingestion. Ultimately, the management of intussusception in this case was in alignment with the typical standard of care despite ingestion of a foreign body as a lead point. Intussusception secondary to kinetic sand ingestion can be safely managed with hydrostatic enema, and bowel rest. Gastric decompression via oro- or nasogastric tube should be considered in cases with ongoing emesis.
Conclusions
Ingestion of kinetic play sand can lead to bowel obstruction with ileo-colonic intussusception. Intussusception is considered a medical emergency and should be treated as soon as possible before potentially fatal complications occur. Consequences of intussusception range from benign symptoms (such as constipation) to more severe complications, including bowel perforation, peritonitis, bowel necrosis, and sepsis (2,3). Our management protocol included hydrostatic reduction, bowel rest, intravenous hydration, follow-up imaging, and observation in the controlled environment of the hospital. Gastric decompression should be applied in cases of ongoing emesis. The patient was allowed to drink a clear liquid diet once she was pain free and without clinical or radiographic evidence of bowel obstruction. This report serves to raise awareness of potential dangers of kinetic sand ingestion and emphasize that standard management of intussusception via reduction enema is also effective in this clinical scenario.
Acknowledgments
The authors would like to thank Bronson Herr, West Virginia University editor and grant writer, for his editing assistance.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-23-37/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-23-37/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-23-37/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient’s legal guardian for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Popular Mechanics. The Boy Mechanic: Volume II: 1000 Things for Boys to Do. Chicago: Popular Mechanics Press; 1915.
- Edwards EA, Pigg N, Courtier J, et al. Intussusception: past, present and future. Pediatr Radiol 2017;47:1101-8. [Crossref] [PubMed]
- Guo WL, Hu ZC, Tan YL, et al. Risk factors for recurrent intussusception in children: a retrospective cohort study. BMJ Open 2017;7:e018604. [Crossref] [PubMed]
- Plut D, Phillips GS, Johnston PR, et al. Practical Imaging Strategies for Intussusception in Children. AJR Am J Roentgenol 2020;215:1449-63. [Crossref] [PubMed]
- Marsicovetere P, Ivatury SJ, White B, et al. Intestinal Intussusception: Etiology, Diagnosis, and Treatment. Clin Colon Rectal Surg 2017;30:30-9. [Crossref] [PubMed]
- Eraki ME. A comparison of hydrostatic reduction in children with intussusception versus surgery: Single-centre experience. Afr J Paediatr Surg 2017;14:61-4. [Crossref] [PubMed]
- Liu ST, Tang XB, Li H, et al. Ultrasound-guided hydrostatic reduction versus fluoroscopy-guided air reduction for pediatric intussusception: a multi-center, prospective, cohort study. World J Emerg Surg 2021;16:3. [Crossref] [PubMed]
- Moles AD, McGhite A, Schaaf OR, et al. Sand impaction of the small intestine in eight dogs. J Small Anim Pract 2010;51:29-33. [Crossref] [PubMed]
- Consumer Product Safety Improvement Act of 2008. Congress; Aug 14, 2008.
- Liu L. What Happens if my Child Eats Kinetic Sand? National Capitol Poison Center. Available online: https://www.poison.org/articles/what-if-my-child-eats-kinetic-sand-204
- Abutarbush SM, Petrie L. Fatal sand impaction of the spiral colon in a 1-month-old alpaca. Can Vet J 2006;47:683-4. [PubMed]
- Papazoglou LG, Patsikas MN, Papadopoulou P, et al. Intestinal obstruction due to sand in a dog. Vet Rec 2004;155:809. [PubMed]
Cite this article as: Turner A, Sico R, Seifarth FG. Ingestion of kinetic sand leading to intussusception and bowel obstruction in a child: a case report. AME Case Rep 2024;8:13.


