
Non-recurrent laryngeal nerve injury associated with an aberrant right subclavian artery: a case report
Highlight box
Key findings
• Aberrant right subclavian arteries (ARSAs) are closely associated and can be used to indirectly predict the presence of a right non-recurrent laryngeal nerve (NRLN).
• A left sided surgical approach is equivalent in risk to a right sided approach and can reduce the risk of a recurrent laryngeal nerve (RLN) injury in the context of a right sided NRLN.
What is known and what is new?
• A NRLN significantly raises the risk of a nerve injury.
• The presence of a NRLN can be incidentally picked-up preoperatively by identifying associated aberrant vasculature (such as an ARSA) on routine preoperative imaging.
What is the implication, and what should change now?
• Identification of an ARSA on preoperative imaging should prompt a left sided surgical approach to avoid injury to a right NRLN.
Introduction
Recurrent laryngeal nerve (RLN) injury is a well-known complication of surgery in the neck. The RLNs innervate all of the intrinsic muscles of the larynx (except for the cricothyroid muscles), as well as providing sensation to the larynx below the level of the vocal folds. Injury to the nerve may cause hoarseness due to temporary or permanent vocal cord paralysis and have a profound impact on a patient’s quality of life (1,2).
A direct or non-recurrent laryngeal nerve (NRLN) is a rare embryologically-derived variant of the RLN first described by George William Stedman in 1823. The non-recurrent variant exits directly from the vagus nerve to supply the larynx without looping down around the subclavian artery (3). NRLNs arise almost exclusively on the right side and are closely associated with vascular anomalies of the aortic arch, such as an aberrant right subclavian artery (ARSA) (4).
The anomalous anatomy of NRLNs has been well described as a serious risk factor for iatrogenic nerve injury (2), as the nerve’s path crosses the surgical field of typical anterior approaches to the cervical spine (5). Due to its vulnerability, undetected NRLNs can result in a sixfold increase in rates of intraoperative nerve injuries during thyroid surgery (6). Although the incidence of NRLNs remain rare at 0.8–2.2% of the population (7), the identification of a NRLN is very clinically relevant for surgeons, as early recognition of its presence and appropriate changes to surgical approach can save the nerve from potential injury. We present this case in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-23-65/rc).
Case presentation
A 61-year-old gentleman was referred by his family doctor with a history of radiating left arm pain and paraesthesia consistent with C6 +/− C7 radiculopathy. He had a neck disability index of 36%. A magnetic resonance imaging (MRI) scan was performed which showed evidence of multi-level cervical spondylosis, with marked foraminal stenosis at C5/6 and C6/7 on the left-hand side (Figure 1A).
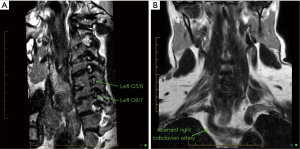
The patient was initially trialled with conservative management, including a targeted C6 nerve root injection. However, the patient failed conservative treatment, and surgical management was pursued: a C5/6 and C6/7 anterior cervical discectomy and fusion. Incidental note was made on the preoperative MRI report of an ARSA following a retro-oesophageal path (Figure 1B).
Surgery was performed using a right sided cervical approach. The approach was technically challenging owing to a short, thick neck; however, the procedure was successfully completed without apparent complications. The right RLN was not visualised during the operation.
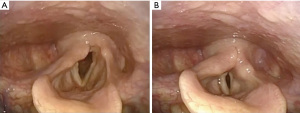
Post-operatively the patient woke with marked dysphonia. He was referred for an otorhinolaryngology (ORL) opinion. Laryngoscopy revealed immobility of the right vocal fold (Figure 2), most likely due to vocal fold paralysis owing to a right NRLN palsy. The patient underwent a right vocal fold injection laryngoplasty with a temporary injectable (hyaluronic acid) with immediate improvement in his voice. The patient’s voice recovered and remained asymptomatic after 1-year post-injection laryngoplasty.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
The presence of a NRLN significantly raises the risk of a nerve injury. However, the aberrant vasculature associated with a NRLN can be visualised on preoperative imaging and therefore should be used to modify the surgical approach to reduce the chance of nerve injury.
Anatomy of the RLN
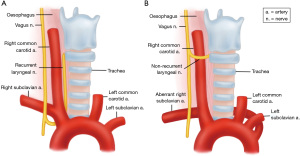
Normally, the RLN exits the vagus nerve at the root of the neck and loops posteriorly around the right subclavian artery on the right; and through the aortic arch at the level of the ligamentum arteriosum on the left, before coursing superiorly in the tracheoesophageal groove until it reaches the cricothyroid junction and enters the larynx (1,7). A typical anterior surgical approach to the cervical spine would involve an incision medial to the sternocleidomastoid muscle where the RLN, running deep in the tracheoesophageal groove, would not be exposed (5).
Embryological origins of a NRLN and ARSA
Embryologically, a right sided NRLN usually results from partial regression of the fourth pharyngeal arch during embryological development (8). Of the paired primitive arches, the fourth arch becomes the subclavian artery on the right and the aortic arch on the left. As the embryo develops and the thoracic organs descend, the nerves loop around their associated arch structures and assume their natural recurrent courses (4).
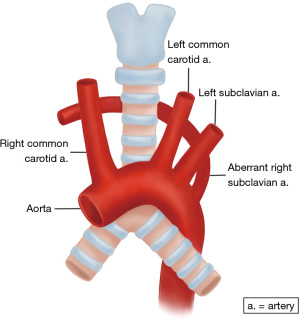
Regression of the arch results in the absence of the brachiocephalic artery and the development of an ARSA, where the artery arises directly from the aortic arch downstream to the left subclavian artery and then crosses the midline posterior to the oesophagus (1) (Figure 3). While the retro-oesophageal route is the most common (80%), some cases have been reported of the artery following an inter-oesophagotracheal (15%), or pretracheal course (5%) (9). An ARSA is also known as the arteria lusoria (derived from Latin for ‘freak of nature’) and is the most common vascular anomaly of the aortic arch, occurring in 0.5–2% of individuals (10).
This atypical vascular pattern of the right subclavian artery permits the cephalad migration of the right RLN (4). The nerve is allowed to migrate freely in the neck as the fetus grows longitudinally (8), and thus has a much more direct path across the neck to the larynx (Figure 4).
Therefore, the existence of an ARSA is a strong indicator of the presence of a right sided NRLN. An ARSA was present in 86.7% of NRLN cases in a meta-analysis by Henry et al. (11). A subsequent systematic review showed an even higher incidence, with 97% of right sided NRLNs being accompanied by an ARSA (7).
The review by Bakalinis et al. (7) also identified three cases of left sided NRLNs (2.9% of all NRLNs identified), which were all associated with a right sided aortic arch and/or situs inversus. NRLNs on the left side are extremely rare and have always been reported accompanied by significant vascular pathologies such as situs inversus (8).
NRLNs are quite rare in the general population, having a reported incidence of 0.3–0.8% on the right and 0.004% on the left side (12), although incidences on the right side have been reported as high as 2.2% (7) and 6% (13).
The existence of a NRLN without the associated vascular anomalies is very rare and has no clear embryological explanation (8). Tateda et al. (14) described one patient with a right NRLN without any detectable vascular anomalies, where intraoperative neuromonitoring (IOMN) was used to identify the nerve and careful dissection was performed to mobilise it out of the surgical field.
Preoperative identification of a NRLN
Given that NRLNs are almost always associated with aberrant vasculature (4), preoperative imaging of the great vessels can indirectly predict the presence of a NRLN (7). Ultrasound can detect an ARSA by the absence of the “Y sign” of the brachiocephalic artery, while computerised tomography (CT) or MRI scans can detect the “hook-like” course of ARSA as it crosses the midline (15). Screening for ARSAs or other vascular anomalies can be done via the preoperative CT or MRI scans routinely performed before all cervical spinal procedures.
Changes to surgical approach in context of NRLNs
Utilising preoperative imaging can inform an appropriate surgical approach to help reduce the risk of nerve damage. Attempts to mitigate the risk of nerve injuries have resulted in rising uses of IONM as an adjunct to the gold standard of visual nerve identification (16). Donatini et al. (13) described a standardized method of IONM to identify and preserve NRLNs throughout thyroid operations; neuro-monitoring was achieved by utilising neural integrity monitor (NIM) endotracheal tubes lined with surface electrodes to detect electromyographic (EMG) signals from the vocal folds. Vagus nerve stimulation was then performed both proximally and distally to the inferior thyroid artery, with absence of EMG signals upon distal stimulation being suggestive of a high/early branching RLN (i.e., a NRLN). This would prompt a careful dissection of the NRLN around the carotid region, with further confirmation of the nerve performed via direct neurostimulation of the suspected nerve. IONM can be divided into two generations: non-continuous and continuous monitoring, the latter of which can allow for real-time monitoring of EMG signals throughout procedures (17), with loss of signal confirming an injury to the nerve.
Despite recent wide-spread adoption especially in thyroid procedures, the actual protective benefit of IONM use on RLN injuries remained controversial; some large studies have found decreased rates of nerve injuries, while others showed an insignificant effect. More recent meta-analyses such as Bai & Chen (17) have shown that IONM does plays a role in preventing both transient and permanent nerve injury compared to conventional visualisation, especially in patients undergoing bilateral thyroidectomies. This benefit still persisted after sensitivity analysis (17). However, IONM remains a complex multi-step process requiring specialised equipment and a steep learning curve, with a potential prolonging of required surgical time (16). However, it has been reported that the implementation of IONM does not actually increase the costs of a thyroid surgical procedure (13).
Given that NRLNs arise almost exclusively on the right side (4), a potentially simpler alternative solution is to perform the operation on the left side, away from the NRLN once its associated vasculature has been confirmed on imaging.
The decision on which side of the neck to make the incision for anterior cervical spinal surgery is derived from multiple factors, including the surgeon’s training, dominant hand, level of proposed surgery, and patient history of prior neck surgery. A review by Beutler et al. (18) concluded that there did not appear to be a significant correlation or association between the side of approach and risk of RLN injury. In the case of standard anatomy, they suggested that the surgeon may safely approach from the side of personal preference and experience. This was echoed by Kilburg et al. (19), who found that the side of approach had no significant impact on RLN injury incidence. Individual risk assessment of each patient was recommended, and risk of injury in the presence of a right sided NRLN has been used to justify the routine choice of a left sided incision and approach for anterior cervical surgery (18).
Conclusions
We present the case of a patient who had a right NRLN with associated ARSA, who sustained a nerve injury owing to an anterior cervical discectomy and fusion procedure. Given our experience with this case, identification of vascular anomalies associated with NRLNs on preoperative imaging should prompt a left sided approach to avoid a nerve injury during surgery.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-23-65/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-23-65/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-23-65/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lee YK, Yang W, Ghedia R, et al. Non-recurrent laryngeal nerve and aberrant subclavian artery in thyroidectomy. BMJ Case Rep 2022;15:e251374. [Crossref] [PubMed]
- Morais M, Capela-Costa J, Matos-Lima L, et al. Nonrecurrent Laryngeal Nerve and Associated Anatomical Variations: The Art of Prediction. Eur Thyroid J 2015;4:234-8. [Crossref] [PubMed]
- Stedman GW. A Singular Distribution of Some of the Nerves and Arteries in the Neck, and the Top of the Thorax. Edinb Med Surg J 1823;19:564-5. [PubMed]
- Coady MA, Adler F, Davila JJ, et al. Nonrecurrent laryngeal nerve during carotid artery surgery: case report and literature review. J Vasc Surg 2000;32:192-6. [Crossref] [PubMed]
- Ladeira Craveiro V, Osler P, Rocco JW, et al. A Left Nonrecurrent Inferior Laryngeal Nerve in a Patient with Vascular and Atlantoaxial Abnormalities: A Case Report. JBJS Case Connect 2014;4:e120. [Crossref] [PubMed]
- Toniato A, Mazzarotto R, Piotto A, et al. Identification of the nonrecurrent laryngeal nerve during thyroid surgery: 20-year experience. World J Surg 2004;28:659-61. [Crossref] [PubMed]
- Bakalinis E, Makris I, Demesticha T, et al. Non-Recurrent Laryngeal Nerve and Concurrent Vascular Variants: A Review. Acta Med Acad 2018;47:186-92. [Crossref] [PubMed]
- Wang Y, Ji Q, Li D, et al. Preoperative CT diagnosis of right nonrecurrent inferior laryngeal nerve. Head Neck 2011;33:232-8. [Crossref] [PubMed]
- Dupuis C, Ponte C, Remy J, et al. Aberrant sub-clavicular arteries in children (20 cases). Arch Fr Pediatr 1970;27:917-35. [PubMed]
- Brauner E, Lapidot M, Kremer R, et al. Aberrant right subclavian artery- suggested mechanism for esophageal foreign body impaction: Case report. World J Emerg Surg 2011;6:12. [Crossref] [PubMed]
- Henry BM, Sanna S, Graves MJ, et al. The Non-Recurrent Laryngeal Nerve: a meta-analysis and clinical considerations. PeerJ 2017;5:e3012. [Crossref] [PubMed]
- Mahmodlou R, Aghasi MR, Sepehrvand N. Identifying the Non-recurrent Laryngeal Nerve: Preventing a Major Risk of Morbidity During Thyroidectomy. Int J Prev Med 2013;4:237-40. [PubMed]
- Donatini G, Carnaille B, Dionigi G. Increased detection of non-recurrent inferior laryngeal nerve (NRLN) during thyroid surgery using systematic intraoperative neuromonitoring (IONM). World J Surg 2013;37:91-3. [Crossref] [PubMed]
- Tateda M, Hasegawa J, Sagai S, et al. Nonrecurrent inferior laryngeal nerve without vascular anomaly as a genuine entity. Tohoku J Exp Med 2008;216:133-7. [Crossref] [PubMed]
- Polednak AP. Anatomical variation in the right non-recurrent laryngeal nerve reported from studies using pre-operative arterial imaging. Surg Radiol Anat 2019;41:943-9. [Crossref] [PubMed]
- Randolph GW, Dralle HInternational Intraoperative Monitoring Study Group. Electrophysiologic recurrent laryngeal nerve monitoring during thyroid and parathyroid surgery: international standards guideline statement. Laryngoscope 2011;121:S1-16. [Crossref] [PubMed]
- Bai B, Chen W. Protective Effects of Intraoperative Nerve Monitoring (IONM) for Recurrent Laryngeal Nerve Injury in Thyroidectomy: Meta-analysis. Sci Rep 2018;8:7761. [Crossref] [PubMed]
- Beutler WJ, Sweeney CA, Connolly PJ. Recurrent laryngeal nerve injury with anterior cervical spine surgery risk with laterality of surgical approach. Spine (Phila Pa 1976) 2001;26:1337-42. [Crossref] [PubMed]
- Kilburg C, Sullivan HG, Mathiason MA. Effect of approach side during anterior cervical discectomy and fusion on the incidence of recurrent laryngeal nerve injury. J Neurosurg Spine 2006;4:273-7. [Crossref] [PubMed]
Cite this article as: Li JW, Vokes D, Heppner P. Non-recurrent laryngeal nerve injury associated with an aberrant right subclavian artery: a case report. AME Case Rep 2024;8:6.


