Intraoperative chylous leak diagnosis by preoperative oral administration of ice cream: a case report
Highlight box
Key findings
• Chylous leakage due to lymphatic vessel injury in the chest wall is rare but may cause postoperative chylothoraces.
• Preoperative oral administration of dairy products contributed to prevention of postoperative chylothorax.
What is known and what is new?
• Preoperative oral administration of dairy products is widely recognized as a useful method for identifying site of chylous leakage during surgery for chylothoraces.
• Preoperative scheduled oral administration of dairy products for initial surgery is also useful for intraoperatively detecting lymphatic vessel injuries in cases wherein chylothorax is of high concern.
What is the implication, and what should change now?
• Although infrequent, chylothoraces due to lymphatic vessel injury in the chest wall should be kept in mind.
• There are still many unknown aspects of lymphatic flow in the chest wall, recommending that data be collected on such cases.
Introduction
Background
Chylothorax is an intractable postoperative complication of thoracic surgery (1). This complication is generally caused by injury to the thoracic duct itself or its branches (2), with an incidence of 1.4–1.8% after pulmonary resections with mediastinal lymph node dissections (3,4) and 1–9% after esophagectomies (1). Once a chylothorax develops, additional treatments such as dietary therapy, pleurodesis, lymphatic embolization, and re-operation are required, resulting in prolonged hospitalization (1). Hence, avoiding chylothoraces is important in initial surgery.
Rationale and knowledge gap
Rare cases of chylothoraces due to injury to lymph vessels in the chest wall have been reported (5,6). Although preoperative oral administration of dairy products is widely recognized as a useful method for identifying site of chylous leakage during surgery for chylothoraces (7-10), patients who undergo surgery, excluding those with chylothoraces, fast overnight (1). All cases of chylothoraces due to injury to lymphatic vessels in the chest wall have been reported as postoperative complications (5,6), suggesting that identifying and repairing chylous leakage points intraoperatively during the initial surgery is very difficult.
Objective
Herein, we report a surgical case of a middle mediastinal tumor that was suspected to be a thoracic duct cyst or an intrathoracic lymphangioma. In this case, the surgical procedure was performed after the scheduled oral administration of dairy products. Chylous leakage in the chest wall was intraoperatively detected and successfully repaired during the initial surgery, avoiding a postoperative chylothorax. We present this case in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-23-126/rc).
Case presentation
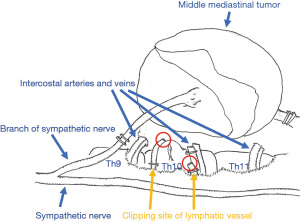
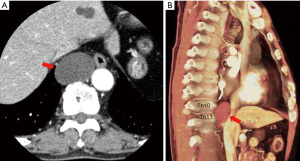
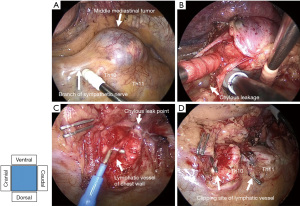
The patient was a 68-year-old male with a history of Graves’ disease, hypertension, reflux esophagitis, and depression. Computed tomography (CT) was performed to examine the cause of the patient’s loss of appetite, detecting a middle mediastinal tumor. A CT follow-up revealed that the tumor was enlarging. Therefore, the patient was referred to our hospital for surgical treatment. A CT scan at our hospital showed a 4.5-cm cystic lesion in contact with the esophagus and descending aorta on the ventral side of the vertebral body (Th10 to Th11 level), which was suspected to be a thoracic duct cyst or an intrathoracic lymphangioma based on imaging findings (11,12) (Figure 1A,1B). We were highly concerned about the development of a chylothorax since both types of tumors originate from lymphatic vessels. Hence, vanilla ice cream (110 mL) containing 15% of milk fat (Häagen-DazsTM, Tokyo, Japan) was administered orally 1 hour before entering the operating room to intraoperatively detect chylous leakage in case of injury to the major lymphatic vessels. The middle mediastinal tumor originated from a branch of the sympathetic nerve (Figure 2A) and was not connected to the lymphatic vessels, including the thoracic duct. The tumor was removed thoracoscopically. However, chylous leakage was identified in the injured lymphatic vessel of the chest wall (Figure 2B,2C). Since the thoracic duct was not intraoperatively identified, the injured lymphatic vessel was not the thoracic duct itself. The injured lymphatic vessel was repaired by clipping the leak points cranially and caudally (Figure 2D). The surgical scheme is shown in Figure 3. The operative time was 125 minutes, and the estimated blood loss was 80 mL. The tumor was histologically diagnosed as a schwannoma with cystic degeneration. Preoperative CT images and the surgical procedure are shown in Video 1.
The patient resumed eating on the day of the surgery, and the chest tube drainage fluid was not chylous. The chest drainage tube was removed on postoperative day 2, and the patient was discharged on postoperative day 5 without postoperative complications. At the 1-year follow-up, no chylothorax was observed.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and accompanying images and video. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Key findings
A male patient with a suspected thoracic duct cyst or an intrathoracic lymphangioma underwent surgery after preoperative oral administration of dairy products. Although the tumor was neurogenic with cystic degeneration, chylous leakage due to injury to the lymphatic vessel in the chest wall was detected and repaired during the initial surgery. No postoperative chylothorax was observed.
Strengths and limitations
The strength of this report is that the initial surgery for a mediastinal tumor, which was suspected to be a thoracic duct cyst or an intrathoracic lymphangioma, was performed after oral administration of dairy products, and the development of postoperative chylothorax due to lymphatic vessel injury in the chest wall could be prevented. Therefore, preoperative oral administration of dairy products was verified to be a useful method not only at the time of re-operation for postoperative chylothoraces but also at the time of initial surgery. In addition, a limitation of this report is that there are still many unknown aspects of lymphatic flow in the chest wall.
Comparison with similar researches
Although injuries to lymphatic vessels in the chest wall rarely cause chylothoraces, all cases have been reported as postoperative complications (5,6). To the best of our knowledge, this is the first report of the detection of chylous leakage in the chest wall during initial surgery for a mediastinal tumor and prevention of a postoperative chylothorax. Past literatures reported that the timing of oral administration of dairy products was from 30 minutes to 3 hours before surgery for chylothorax (7-10). The types of dairy products could vary from ice cream, butter, milk, and cream. Moreover, specific quantity of fat was not basically discussed (7-10). In this case, thoracic surgeons and anesthesiologists discussed these aspects, and fat-rich vanilla ice cream was orally administered 1 hour before surgery. Accumulating reports on the timing of oral administration of dairy products and types of dairy products may provide a clearer indication.
Explanations of findings
The thoracic duct originates from the cisterna chyli at the level of the second lumbar vertebra, ascends in the posterior mediastinum between the aorta and azygos vein, and then flows into the left venous angle at the neck (1). However, the thoracic duct often has anomalous courses: 40–60% flow into the azygos, intercostal, and lumbar veins, and 25–30% branch into multiple ducts at the level of the diaphragm (13). As a result, there are cases of multiple thoracic ducts and others of thoracic ducts running through a vine-like pattern (14,15). Hence, the lymphatic vessel in the chest wall that was injured in this case might have been a branch of the thoracic duct running down the chest wall.
Implications and actions needed
Accumulation of similar case reports may lead to a better understanding of lymphatic flow in the chest wall and reduce the risk of developing chylothorax due to lymphatic vessel injury in the chest wall.
Conclusions
Since chylothorax is an intractable postoperative complication of thoracic surgery, avoiding postoperative chylothoraces is important in the initial surgery. We should keep in mind that injury to the lymphatic vessels in the chest wall complicates chylothoraces, although infrequently reported.
Acknowledgments
We thank Editage (http://www.editage.jp) for the English language editing.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-23-126/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-23-126/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-23-126/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and accompanying images and video. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bender B, Murthy V, Chamberlain RS. The changing management of chylothorax in the modern era. Eur J Cardiothorac Surg 2016;49:18-24. [Crossref] [PubMed]
- Chen C, Wang Z, Hao J, et al. Chylothorax after Lung Cancer Surgery: A Key Factor Influencing Prognosis and Quality of Life. Ann Thorac Cardiovasc Surg 2020;26:303-10. [Crossref] [PubMed]
- Bryant AS, Minnich DJ, Wei B, et al. The incidence and management of postoperative chylothorax after pulmonary resection and thoracic mediastinal lymph node dissection. Ann Thorac Surg 2014;98:232-5; discussion 235-7. [Crossref] [PubMed]
- Yasuura Y, Konno H, Hayakawa T, et al. Chylothorax after pulmonary resection and lymph node dissection for primary lung cancer; retrospective observational study. J Cardiothorac Surg 2022;17:11. [Crossref] [PubMed]
- Ma L, Pu Q, Zhu Y, et al. Chyle leakage in port incision after video-assisted thoracoscopic surgery: case report. J Cardiothorac Surg 2010;5:83. [Crossref] [PubMed]
- Sieczka EM, Harvey JC. Early thoracic duct ligation for postoperative chylothorax. J Surg Oncol 1996;61:56-60. [Crossref] [PubMed]
- Seto K, Kuroda H, Mizuno T, et al. Postoperative chylothorax after pulmonary wedge resection in two patients who underwent radical neck dissection: A case report. Asian J Endosc Surg 2016;9:322-4. [Crossref] [PubMed]
- Furukawa M, Tao H, Tanaka T, et al. Mediastinal chyloma after lung cancer surgery: case report. J Cardiothorac Surg 2016;11:115. [Crossref] [PubMed]
- Shackcloth MJ, Poullis M, Lu J, et al. Preventing of chylothorax after oesophagectomy by routine pre-operative administration of oral cream. Eur J Cardiothorac Surg 2001;20:1035-6. [Crossref] [PubMed]
- Nakamura D, Toishi M, Sakaizawa T, et al. Postoperative chylothorax following lung cancer surgery with an aberrant course of thoracic duct: a case report. J Surg Case Rep 2021;2021:rjab490. [Crossref] [PubMed]
- De Santis M, Martins V, Fonseca AL, et al. Large mediastinal thoracic duct cyst. Interact Cardiovasc Thorac Surg 2010;10:138-9. [Crossref] [PubMed]
- Brown LR, Reiman HM, Rosenow EC 3rd, et al. Intrathoracic lymphangioma. Mayo Clin Proc 1986;61:882-92. [Crossref] [PubMed]
- Brotons ML, Bolca C, Fréchette E, et al. Anatomy and physiology of the thoracic lymphatic system. Thorac Surg Clin 2012;22:139-53. [Crossref] [PubMed]
- Kausel HW, Reeve TS, Stein AA, et al. Anatomic and pathologic studies of the thoracic duct. J Thorac Surg 1957;34:631-41. [Crossref] [PubMed]
- Kim PH, Tsauo J, Shin JH. Lymphatic Interventions for Chylothorax: A Systematic Review and Meta-Analysis. J Vasc Interv Radiol 2018;29:194-202.e4. [Crossref] [PubMed]
Cite this article as: Kawamoto N, Okita R, Okada M, Hayashi M, Inokawa H. Intraoperative chylous leak diagnosis by preoperative oral administration of ice cream: a case report. AME Case Rep 2024;8:8.