
Severe primary hypothyroidism and ovarian hyperstimulation syndrome in a spontaneous pregnancy: a case report
Highlight box
Key findings
• This case elucidates a unique association between severe hypothyroidism and ovarian hyperstimulation syndrome (OHSS) without in vitro fertilization (IVF) procedures.
What is known and what is new?
• Hypothyroidism, known as low thyroid hormone levels, is a common endocrine problem, especially in women, and OHSS is a rare, well-known medical syndrome that usually happens during IVF.
• The case study introduces a rare scenario in which OHSS occurs spontaneously in a pregnant woman with severe primary hypothyroidism. The study suggests a potential pathophysiological mechanism connecting elevated levels of thyroid-stimulating hormone in hypothyroidism to ovarian stimulation.
What is the implication, and what should change now?
• The case report contributes to new insights into spontaneous OHSS in severe hypothyroidism, shedding light on a potential pathophysiological link and emphasizing the importance of individualized patient care. These findings open further research into this less common but clinically significant scenario.
Introduction
Hypothyroidism is one of the most prevalent endocrine disorders in women. In severe cases, it may manifest with myxedema or, in uncommon cases, with the development of ovarian hyperstimulation syndrome (OHSS). OHSS is the most severe and potentially life-threatening iatrogenic complication associated with ovulation induction, occurring in 0.6% to 1.4% of in vitro fertilization (IVF) treatments (1). Few cases of isolated hypothyroidism leading to ovarian hyperstimulation in adult women have been recorded in the medical literature (2-9). Polycystic ovarian syndrome, molar pregnancy, and pituitary gonadotroph adenomas have also been linked to OHSS. This syndrome is characterized by ovarian enlargement, multiple follicular cysts, and acute fluid shifts from the intravascular to extravascular space due to hyperpermeability of the vessels, leading to hypovolemia and hemoconcentration (10). Depending on the signs, symptoms, laboratory test results, and ultrasound findings, it can be classified as mild, moderate, severe, or life-threatening. Due to the complexity of the cysts and their association with elevated tumor markers, this condition can be challenging to diagnose as it can mimic a tumor (11). We present this case in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-23-13/rc).
Case presentation
A 22-year-old Caucasian woman with 4 weeks of amenorrhea and abdominal pain was admitted to the emergency department (ED). The patient was being treated for hypothyroidism with 200 mcg of levothyroxine once daily; however, she decided to discontinue the medication 1 month prior. She reached menarche at age 11; her cycles were irregular, and her last unplanned pregnancy at age 18 years was complicated by acute respiratory distress syndrome due to septic shock, requiring hospitalization and surveillance in an intensive care unit. She had no gynecological pathology and had never received IVF treatment. She did not use any form of contraception. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
The physical examination revealed the presence of mobile adnexal masses.
Thyroid-stimulating hormone (TSH) was 515 IU/mL (reference range, 0.4–4 IU/mL), free thyroxine (fT4) was undetectable (reference range, 0.7–1.8 ng/dL), and cancer antigen-125 (CA-125) was 1,045 U/mL (reference range, 0–10 U/mL). Increased hematocrit, hypoproteinemia, electrolyte abnormalities (hyponatremia, hyperkaliemia), as well as slightly elevated liver enzymes and creatinine levels were detected in blood tests.
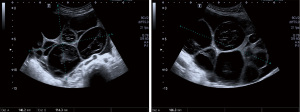
Gynecological ultrasound revealed a single fetus with regular cardiac activity with a gestational age of 9 weeks and 2 days; the ovaries had enlarged dimensions (right: 15 cm × 14 cm × 16.6 cm and left: 15 cm × 8.2 cm × 18.3 cm) with a significant amount of ascitic fluid in the Morrison’s space and left flank (Figure 1).
Transthoracic echocardiogram revealed a mild mitral valve prolapse and circumferential pericardial effusion without any evidence of hemodynamic compromise.
The patient did not know she has pregnant.
The patient was admitted to the hospital and initiated on levothyroxine 100 mcg, enoxaparin 40 mg subcutaneously, and furosemide 40 mg daily due to severe hypothyroidism resulting in spontaneous OHSS accompanied by peritoneal and pericardial effusions. This treatment plan was implemented in response to the patient’s elevated risk of thrombosis.
After 1 week of treatment, symptomatic relief was observed, as well as a reduction in the size of the pericardial effusion detected by echocardiography, a decrease in TSH levels (150 IU/mL), and an increase in fT4. The dose of levothyroxine was gradually increased to 200 mcg, and CA-125 values, ovarian dimensions, and peritoneal fluid decreased.
Risks of preeclampsia, anemia, miscarriage, low birth weight and stillbirth, congestive heart failure, and cretinism were communicated to the patient. With the assistance of her multidisciplinary medical team and the ethics council, she decided to voluntarily terminate the pregnancy at 10 weeks of gestation, the legal limit in Portugal for an abortion. This procedure was performed using mifepristone and misoprostol, under medical supervision. No complications occurred during or after the procedure.
The patient was discharged after spending 2 weeks in the hospital. A new echocardiogram revealed a decrease in pericardial effusion volume.
Before discharge, we discussed the necessity of therapeutic adherence with the patient, and she was asked if she planned to initiate a contraceptive method; she denied this intention.
Three months after discharge, a gynecological ultrasound revealed a reduction in the size of the ovarian cysts and a normalization of TSH levels.
Discussion
The pathophysiological mechanism of OHSS is not fully understood. It appears to be dependent on exposure of the ovaries to beta-human chorionic gonadotropin (b-HCG), which induces the production and release of vasoactive substances (like vascular endothelium growth factor, renin-angiotensin, several pro-inflammatory cytokines, and endothelin-1). These substances increase the permeability of capillaries, resulting in the extravasation of fluid from the intravascular space into the extravascular space and its accumulation in the peritoneal, pleural, and pericardial cavities. This process results in hypovolemia and hemoconcentration, which interfere with renal filtration and excretion by promoting hypercoagulability (2).
The pathophysiology association between OHSS and hypothyroidism is still unknown and requires further study. TSH, follicle-stimulating hormone (FSH), and luteinizing hormone (LH) all have well-known alpha chains. The high levels of TSH observed in hypothyroidism and their cross-reactivity with certain gonadotropins appears to increase the concentration of FSH and LH, thereby causing hyperstimulation of the ovaries. Rotmensch and Scommegna (6) hypothesized that estriol is formed via a 16-hydroxylation pathway as opposed to the 2-hydroxylation path prevalent in hypothyroid patients. Replacing estradiol with estriol would significantly increase ovarian stimulation due to a reduction in feedback regulation (12,13).
Multiple bilateral multilocular cysts, peritoneal and pericardial effusions, and elevated TSH levels helped establish the diagnosis of spontaneous OHSS in our patient, who had no history of IVF treatments. The differential diagnosis also considered the possibility of neoplasia. Low carcinoembryonic antigen (CEA) values and high estrogen concentrations (greater than 6,000 pg/mL) were consistent with the diagnosis of OHSS. Moreover, simple, multiple, homogeneous, thin-walled, and bilateral cysts indicate a benign clinical condition (14).
Thyroid dysfunction is the second most prevalent endocrine disorder affecting women of reproductive age, following hypothyroidism. In the first trimester of pregnancy, the fetus’s development depends on thyroid hormones. There is an increase in maternal T4 during this time, which is transferred to the fetus and converted into T3. This hormone is required for neuronal development, including myelination, regulation of cell migration in the cortex, cerebellum, hippocampus, and neuronal differentiation (15,16). Undiagnosed or untreated hypothyroidism in pregnant women is associated with an increased risk of miscarriage, premature delivery, placental abruption, intrauterine growth restriction, gestational hypertension, low birth weight, and a deficit in fetal neurocognitive development (13,14).
A systematic review examined the relationship between hypothyroidism and ovarian stimulation syndrome in patients with spontaneous pregnancies unrelated to exogenous gonadotropin induction. In July 2023, a search of PubMed and Medline yielded eight cases from 1998 to 2023 (3,4,13,17-23).
All cases occurred in females, and the mean age at diagnosis ranged from 22 to 35 years, with a standard deviation of 4.9 years. The patients were associated with singleton pregnancies and were diagnosed between 7 and 13 weeks, or 10 4.1 weeks, of gestation. This is consistent with the findings that OHSS is more likely to be detected between the 8th and 14th week of pregnancy than iatrogenic OHSS, which tends to occur between the 3rd and 8th week of gestation.
All patients with abnormal thyroid function and elevated TSH levels received levothyroxine replacement therapy. In two instances, echographic (20) and laparoscopic (17) excision of the cysts was required due to their insufficient regression with treatment. In seven cases, delivery was conceivable; in only one case, the patient chose to have an abortion (4). This case report aims to demonstrate the rarity of this condition and the causal connection between hypothyroidism and ovarian hyperstimulation, as suggested by the consistent regression of ovarian tumors following the initiation of thyroid hormone replacement therapy. In addition, this study aims to contribute to a greater comprehension of this pathological process.
Our patient had been diagnosed with hypothyroidism since she was 18 years old; however, she took the medication inconsistently. She was informed of all associated risks with this pregnancy. Although there are records in the literature of pregnancies with severe OHSS that progressed to the third trimester without complications (2-5), in the presence of an unplanned and unintended pregnancy, the patient preferred to exercise her personal and legal right to terminate the pregnancy.
OHSS is a self-limiting condition. The treatment should be restrained, and symptom centered. For women with uncontrolled hypothyroidism, the primary treatment options include thyroid hormone replacement with TSH monitoring, paracentesis for patients with significant ascites, thoracentesis for those with pleural effusion, and prophylaxis against thromboembolism. In severe cases, however, patients unfit for symptomatic treatment should undergo surgery (10-12), particularly those with an ovarian cyst with a twisted pedicle or a ruptured ovary. In this instance, the patient was administered levothyroxine.
Conclusions
In conclusion, this case study illustrates the rare but important occurrence of spontaneous OHSS in the context of severe hypothyroidism during pregnancy. It emphasizes the need for clinical vigilance, early diagnosis, and comprehensive care in managing such cases, as well as the significance of thyroid management in pregnancy. Additionally, it suggests potential avenues for future research in this field.
In cases of hypothyroidism, pregnancy should be avoided until euthyroidism is achieved with replacement therapy, and it is essential to adhere to thyroid replacement therapy, emphasizing the need for therapeutic adherence.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-23-13/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-23-13/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDeri
References
- Francisco C, Júlio C, Pinto G, et al. Ovarian hyperstimulation syndrome in a spontaneous pregnancy. Acta Med Port 2011;24:635-8. [PubMed]
- Alqurashi RM, Alsuwat SA, Yamani MA, et al. Onset of Spontaneous Ovarian Hyperstimulation Syndrome in the Third Trimester: Case Report. Cureus 2022;14:e20940. [Crossref] [PubMed]
- Alzebidi JA, Almushri K, Elmoheen R. Spontaneous Ovarian Hyperstimulation Syndrome Associated With Primary Hypothyroidism. Cureus 2023;15:e33247. [Crossref] [PubMed]
- Lussiana C, Guani B, Restagno G, et al. Ovarian hyper-stimulation syndrome after spontaneous conception. Gynecol Endocrinol 2009;25:455-9. [Crossref] [PubMed]
- Rastin Z, Ghomian N, Khadem-Rezaiyan M. Severe Ovarian Hyperstimulation Syndrome in A Spontaneous Pregnancy with Normal Singleton Fetus: A Case Report. Iran J Nurs Midwifery Res 2019;24:310-2. [PubMed]
- Rotmensch S, Scommegna A. Spontaneous ovarian hyperstimulation syndrome associated with hypothyroidism. Am J Obstet Gynecol 1989;160:1220-2. [Crossref] [PubMed]
- Rajaram S, Bhaskaran S, Aggarwal P, et al. Spontaneous ovarian hyperstimulation mimicking ovarian neoplasm: A rare complication of hypothyroidism. J Obstet Gynaecol 2015;35:532-3. [Crossref] [PubMed]
- Taher BM, Ghariabeh RA, Jarrah NS, et al. Spontaneous ovarian hyperstimulation syndrome caused by hypothyroidism in an adult. Eur J Obstet Gynecol Reprod Biol 2004;112:107-9. [Crossref] [PubMed]
- Van Voorhis BJ, Neff TW, Syrop CH, et al. Primary hypothyroidism associated with multicystic ovaries and ovarian torsion in an adult. Obstet Gynecol 1994;83:885-7. [PubMed]
- Grossman LC, Michalakis KG, Browne H, et al. The pathophysiology of ovarian hyperstimulation syndrome: an unrecognized compartment syndrome. Fertil Steril 2010;94:1392-8. [Crossref] [PubMed]
- Namavar Jahromi B MD, Parsanezhad ME MD, Shomali Z MD, et al. Ovarian Hyperstimulation Syndrome: A Narrative Review of Its Pathophysiology, Risk Factors, Prevention, Classification, and Management. Iran J Med Sci 2018;43:248-60. [PubMed]
- Lima M, Sousa M, Oliveira C, et al. Ovarian hyperstimulation syndrome: experience of a reproductive medicine center 2005-2011. Acta Med Port 2013;26:24-32. Erratum in: Acta Med Port 2013;26:184. [Crossref] [PubMed]
- Banker M, Garcia-Velasco JA. Revisiting ovarian hyper stimulation syndrome: Towards OHSS free clinic. J Hum Reprod Sci 2015;8:13-7. [Crossref] [PubMed]
- Edwards-Silva RN, Han CS, Hoang Y, et al. Spontaneous ovarian hyperstimulation in a naturally conceived pregnancy with uncontrolled hypothyroidism. Obstet Gynecol 2008;111:498-501. [Crossref] [PubMed]
- Montanelli L, Delbaere A, Di Carlo C, et al. A mutation in the follicle-stimulating hormone receptor as a cause of familial spontaneous ovarian hyperstimulation syndrome. J Clin Endocrinol Metab 2004;89:1255-8. [Crossref]
- Smits G, Govaerts C, Nubourgh I, et al. Lysine 183 and glutamic acid 157 of the TSH receptor: two interacting residues with a key role in determining specificity toward TSH and human CG. Mol Endocrinol 2002;16:722-35. [Crossref] [PubMed]
- Sayasneh A, Ekechi C, Ferrara L, et al. The characteristic ultrasound features of specific types of ovarian pathology Int J Oncol 2015;46:445-58. (review). [Crossref] [PubMed]
- Sahay RK, Nagesh VS. Hypothyroidism in pregnancy. Indian J Endocrinol Metab 2012;16:364-70. [Crossref] [PubMed]
- Delabaere A, Tran X, Jardon K, et al. Spontaneous ovarian hyperstimulation syndrome in a pregnancy with hypothyroidism. Gynecol Obstet Fertil 2011;39:e64-7. [Crossref] [PubMed]
- Cardoso CG, Graça LM, Dias T, et al. Spontaneous ovarian hyperstimulation and primary hypothyroidism with a naturally conceived pregnancy. Obstet Gynecol 1999;93:809-11. [PubMed]
- Sridev S, Barathan S. Case report on spontaneous ovarian hyperstimulation syndrome following natural conception associated with primary hypothyroidism. J Hum Reprod Sci 2013;6:158-61. [Crossref] [PubMed]
- Borna S, Nasery A. Spontaneous ovarian hyperstimulation in a pregnant woman with hypothyroidism. Fertil Steril 2007;88:705.e1-3. [Crossref] [PubMed]
- Nappi RG, Di Naro E, D'Aries AP, et al. Natural pregnancy in hypothyroid woman complicated by spontaneous ovarian hyperstimulation syndrome. Am J Obstet Gynecol 1998;178:610-1. [Crossref] [PubMed]
Cite this article as: Guerra M, Marado D, Silva F, Almeida MC. Severe primary hypothyroidism and ovarian hyperstimulation syndrome in a spontaneous pregnancy: a case report. AME Case Rep 2024;8:26.


