
Case report of crusted scabies, brief review of its pathophysiology and latest data
Highlight box
Key findings
• Crusted scabies can have a great impact on a patient’s appearance and quality of life.
• Many cases of crusted scabies remain undiagnosed for a long time in developed countries.
What is known and what is new?
• Crusted scabies is typically met in patients with immunosuppression, sensory impairment dermal diseases, or physical immobilization.
• Dermoscopy plays a crucial role in precise scabies detection, without the use of a scalpel.
• Host immune responses to crusted scabies is different than to ordinary scabies.
• New studies in Austria refer to cases of scabies resistant to topical permethrin use.
What is the implication, and what should change now?
• Detailed clinical, dermatoscopical, and sometimes histological, examination of a patient with pruritus is needed, in order to detect the underlying cause.
• We highlight the need for more structured guidelines concerning crusted scabies management and record of a possible resistance to widely prescribed and over-the-counter medication.
Introduction
Scabies is a highly contagious infectious skin disease provoked by the ectoparasite Sarcoptes scabiei varietas hominis (1). Its name derives from the Greek words ‘sarx’ meaning body tissue, ‘koptein’ related to incise and Latin word ‘scabere’, explaining small cuts (1).
According to the World Health Organization, scabies is considered a neglected tropical disease and its prevalence amounts to 100,000,000 cases worldwide (2). Scabies is especially prevalent in Latin America and Pacific area, while Europe records fewer cases (2).
In Greece, its incidence is considered extremely low (3). Recently Louka et al. based on Greek National Public Health Organization registry data, claimed scabies as the most common infectious disease in health care centers among refugees and asylum seekers with an increasing proportional morbidity index in Greece (4). Geographical location of Greece, at the crossroads of Europe, Asia, and Africa may play a key role reasonably (4).
Scabies may present in various forms, although the most-commonly-observed forms include classical scabies and crusted scabies (5). Both are caused by the same parasite, but total mite burden differs (5). Classical scabies is estimated to be caused by less than 15 mites, whereas crusted scabies is hallmarked by high numbers of mites (5).
S. scabiei may affect all people, regardless of social or economic status, with outbreaks frequently in overcrowded places, e.g., nursing homes, asylums, refugee camps or prisons (6). Crusted scabies is more frequent among patients with severe comorbidities; diabetes mellitus, malnutrition or mental-physical-sensory nerve deficits (6). Additionally, immunosuppression is a strong predisposing factor; especially in human immunodeficiency virus/acquired immunodeficiency syndrome, hematologic/oncologic patients or in iatrogenic immune disturbances, e.g., long-term cortisol treatment or immunomodulatory drugs (6,7).
Herein, we present a quite peculiar case of crusted scabies in an elderly patient living in a nursing home in Greece, with a persistent disturbing history of pruritus over 4 months. All latest data in crusted scabies diagnosis, management, and treatment options are discussed. We present this article in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-23-125/rc).
Case presentation
An 86-year-old woman was admitted to our emergency room department with a urinary tract infection. The patient lived in a nursing home residence. She had a medical history of hypertension and diabetes mellitus. Uncompensated cirrhosis on grounds of non-alcoholic steatohepatitis was her main comorbidity.
Due to her impaired consciousness level, she was urgently administered ceftriaxone as empiric infection treatment, which continued according to urine culture results.
The patient regained consciousness and complained of extreme pruritus, especially nocturnal, especially at night for the last 4 months. She was offered in the meantime, several emollients, keratolytic creams, and anti-histamines, with no resolution in itch.
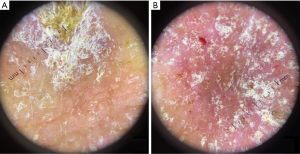
Her clinical examination revealed large erythematous, hyperkeratotic, scaly plaques on the head, eyebrows, chest, trunk, and upper extremities (Figure 1). Subsequent dermoscopy revealed hemorrhage, crusts, and white-yellow scales (Figure 2).
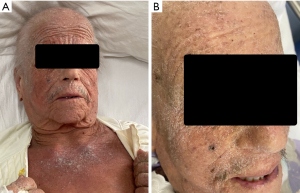
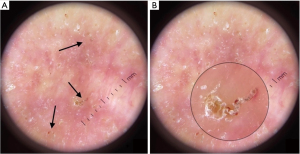
The dorsal hands area presented massive hyperkeratosis with yellow and gray scales and a thick crust; creating a characteristic image reminiscent of sand (“built-up sand appearance”) (Figure 3). Extreme areas of hyperkeratosis on palms and soles were also distinct (palmoplantar keratoderma), with skin fissures in the interdigital areas (Figures 3,4). On the scalp, the patient had hyperkeratosis and quite a few hairs, which were brittle and weak; explaining the mentioned hair loss due to itching. The patient’s nails were thickened and discolored. Numerous small erythematous papules and wavy threadlike burrows of gray color were also noticed on the back, chest, and abdominal area (Figure 5).



Based on the above records, the differential diagnosis included crusted scabies, pruritus due to cirrhosis, seborrheic dermatitis, psoriasis, peripheral T-cell lymphomas, and recalcitrant allergic dermatitis.
Thorough dermoscopic evaluation revealed the “delta-wing jets with contrail” sign and S shape burrows, which correlate to S. scabiei, their burrows, and eggs laid. The mite burden was impressive, with three mites being seen within a single magnification field (Figure 6).
Therefore, a crusted scabies diagnosis was highly likely. Her blood examination, post-infection resolve, stated white blood cells within the normal range 7.59×103/µL, but with significant eosinophilia 14.8% (1.12×103/µL).
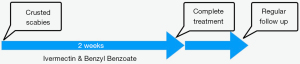
The patient was transferred to an isolated room where her personal items and textiles were sterilized. The nursing staff followed all necessary protective measures when caring for the patient. All close contacts were administered ivermectin prophylactically.
The patient was treated with both benzyl benzoate (BB) lotion 25% on the whole skin surface and 12 mg of ivermectin (200 µg/kg) systemically on days 1, 2, 8, 9 and 15. An ointment with 5% salicylic acid mixed with petrolatum, was also applied twice daily. The patient complained about a severe burning sensation, post-first treatment application which was gradually bearable. Post-first days of medication, a significant pruritus improvement with no new papules emerged was recorded. Two weeks after, the patient was completely itch-relieved and the skin regained normal smoothness. Hyperkeratotic scales on the trunk, scalp, and extremities were completely gone, as well as, palmoplantar keratoderma (Figure 7). The patient, when discharged, had a consultation for a regular dermatological follow-up (Figure 8).

All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Scabies is a common infectious disease, that derives from a high proliferation of Sarcoptes scabiei varietas hominis on human skin (8). The clinical presentation of scabies can adopt a spectrum of clinical manifestations, depending on patient’s medical history, age, epidemiologic data, and skin mites burden (8). These forms include ‘ordinary scabies”, “well-groomed scabies”, “scabies incognito”, “infantile scabies”, “neonatal scabies”, “nodular scabies” and “crusted scabies” (8).
Crusted scabies is a rare diagnostic entity, linked with extreme proliferation of S. scabiei (9). Crusted scabies is also referred to as “Norwegian Scabies”, a reminder of Danielsen and Boeck who first reported a scabies case in a patient with leprosy in Norway (10).
S. scabiei can cause both classical and crusted scabies (11). Life cycle lasts 9–15 days including 4 main forms: eggs, larvae, nymphs, and adult (12). Female parasites produce proteolytic enzymes that facilitate stratum corneum degradation, creating the characteristic burrows, where pregnant female spend their life, laying their eggs (11,13). Then, larvae migrate into the superficial epidermis, where evolved into nymphs gradually (13). Finally, they arrive in skin wrinkles and hair follicles, becoming adult mites; reproducing and start life cycles (13).
When a healthy human is parasite affected, both immunological and mechanical reactions lead to scabies eradication (13). In case of mechanisms damage, a loss of the equilibrium is provoked, leading to hyper-infection of scabies (13). These risk factors include immunosuppression, and major chronic illnesses (13).
Crusted scabies first presentation may differ from classical scabies cases.
Crusted scabies may show a gradual onset of symptoms (14). The eruptions are characterized by thick hyperkeratotic plaques locally or diffusely distributed on an erythematous background (13,14). Brown, yellow, and gray crusts are also commonly observed in hand, feet, head, and neck regions (11,13).
Recently Niode et al. reported neglected cases of crusted scabies with a peculiar clinical image of crusts manifestation in a patient’s hand, called a “built-up sand” appearance (11). In addition, thick crusts create a “rocky surface” image in a patient’s palm, resulted by crust division in deep fissures (11). These two distinct macroscopic findings, were noted in our case; not crusted scabies pathognomonic, but they guided the clinician’s diagnostic survey.
Crusted scabies cases can also develop nail abnormalities, involving plate’s thickness, color, or morphology (13). Crusted scabies cases may not present with pruritus necessarily (13,15). Pruritus loss may be partially explained by lack of immunological response in immunocompromised patients, but further validation of this scenario is needed (13). In rare cases, crusted scabies presented with enlarged lymph nodes (13). The eosinophilia or elevated IgE levels described in crusted scabies, are due to parasitic infection (13). Only Sluzevich et al. have published 2 persistent cases, as first laboratory sign in patients investigated for keratin disorders, who concluded to have crusted scabies diagnosis (16).
Crusted scabies may confuse physicians on their first clinical presentation. Differential diagnosis might include psoriasis, dermatitis, eczema, palmoplantar keratoderma, or even cutaneous T-cell lymphomas (erythrodermic mycosis fungoides/Sézary syndrome) (11).
Crusted scabies diagnosis shares the same tests as classical scabies (14). Lack of specific protocols for scabies diagnosis leads to inconsistencies among clinicians. Specifically, the gold standard method of histologic confirmation of scabies is invasive and offers low sensitivity index (17). Nowadays, extensive dermoscopy use has raised an important question of its efficacy in early scabies mite identification. All relevant published studies comparing dermoscopy with other diagnostic methods robustly highlight dermoscopy having high efficacy in scabies diagnosis (8,18).
Based on all above, International Alliance for Control of Scabies, in 2020 established specific consensus criteria for scabies detection (17). These include 3 confidence levels (A, B, C), referring to confirmed, clinical, and suspected scabies respectively (17).
According to 2020 consensus criteria, dermoscopy alone can confirm scabies diagnosis (level A), as a direct visualization of a scabies mite with a magnification of ×10, requiring a whole-body examination (17).
A typical dermoscopic image of female scabies includes a pigmented triangle (“delta wing jet”), which correlates to the face, chest, and front legs of the mite followed by the semi-translucent body of the mite.
Also, female scabies mites dig the epidermis in order to lay their eggs, creating an intracorneal burrow of a characteristic S shape (19,20). The presence of mite along with the tunnel is typically described as “jet with contrail” (21). Along the sides of burrows, several endarkened spheres might be observed, which correlate to the eggs of scabies mites or “mini triangle sign”, which refers to growing mites inside the eggs (21). Also, in the superficial start of the burrows, many cases describe a “V” shaped scale (19). In our case, scabies diagnosis was easily established, as in dermoscopy we clearly observed the mites, their burrows, as well as their eggs.
All cases of scabies infection, share the same dermoscopic pattern. However, in crusted scabies cases, clinicians may observe high numbers of mite populations, even in a small area (22). To our astonishment, we saw only 3 mites in one dermoscopic image in our case.
In microscopy, histopathologists see the mites in burrows, digging within the stratum corneum, as observed in patients with classical scabies (14,23). However, cases of crusted scabies are characterized by high amounts of mites, along with massive hyperkeratosis, orthokeratosis and parakeratosis in the adjacent area (14,23). Epidermis forms a psoriasiform pattern and can present with excessive granulation (14,23). Feces can be observed along burrows, as brown granules (23). Spongiosis, spongiform pustules and neutrophilic abscesses may also be observed (23). Coarse collagen bundles and dilated capillaries are typically seen in the upper layer of the dermis (23). Also, massive inflammatory infiltrates are seen around vessels or in the papillary dermis (23). The majority of which include eosinophils, although plasma cells and neutrophils have also been described (14,23).
In patients with crusted scabies, extravasation of serum and red blood cells is commonly seen in the stratum corneum (23). This phenomenon leads to the coloration of the white scale seen in crusted scabies into yellow or brown and the presence of scattered small clots in dermoscopy (24).
Both classical and crusted scabies cases are provoked by the same parasite. The wide spectrum of disease’s manifestations had always been a mystery. Researchers’ explanation is supported by an established remarkable difference in inflammatory cell response and chemokine production; proved in relevant studies of clarifying immune-implied mechanisms among classical and crusted scabies infections.
Classical scabies theoretically activates mainly Th1 inflammatory response via high production of Th1-related cytokines (IFN-γ, IL-2, and TNF-α) (5). Also, elevated levels of IL-10 have been recorded, which are linked with immunosuppressive effects (5). In the site of the mite infection, infiltrations of mostly CD4+ T lymphocytes, eosinophils and macrophages have been recorded, without any remarkable blood count test abnormalities (5).
On the contrary, crusted scabies is linked with Th2 cell-mediated response and high production of Th2 cytokines (IL-4, IL-5, and IL-13), Th17 cytokines (IL-17, IL23), and decreased IL-10 (5,25). Skin infection areas are characterized by high concentrations of cytotoxic T-cells, γδ+ cells, eosinophils, and only a few macrophages (5). Laboratory tests, indicative of the elevated eosinophils and γδ T cells are commonly noted (5). Proof of this immune-related motivation was a cohort study of 78 patients with crusted scabies, presented by Roberts et al. The researchers notified increased levels of IgG, IgE, and IgA in the bloodstream, hinting at the underneath immune response reaction to the infectious disease (9).
Yang et al. have rigorously shown that IL-4, one of Th2 cytokines, plays a pivotal role in activating keratinocyte proliferation (26). This interesting finding may further explain hyperkeratosis clinical manifestation in crusted scabies patients meaningfully (9,11).
Of notice, the role of IL-17 in crusted scabies manifestation, since IL-17 is widely engaged in the pathogenesis of psoriasis (27). In this direction, Liu et al. made a respectful effort to measure IL-17 production in areas of infection in crusted scabies patients (25). These findings captivated researchers trying to clarify any possible connection underneath these two discrete diseases. Liu et al. published a nationwide cohort study, proving patients with scabies to be at higher risk of psoriasis (28).
Literature surveillance reveals trial efforts to identify predictive markers of crusted scabies severity. El-Aal et al. conducted a cross-sectional study, proving a high positive correlation between blood IgE levels and crusted scabies severity (29). Hence, the scientists claimed a probable negative correlation between IL-10 and disease severity (29).
The severity of crusted scabies is an important factor of disease prognosis, since crusted scabies when untreated may lead to high fatality rates, mainly due to secondary complications (11). Comorbidities of patients with crusted scabies may also deteriorate patient’s prognosis (30).
All treatment options for scabies aim either to kill parasites (“acaricidal”) or its eggs (“ovicidal”) (13). Medication can be applied on patient’s skin as a cream or can be administered systemically (13). General principles of scabies management include topical application of substances, e.g., BB, permethrin or oral administration of ivermectin (13). BB and permethrin have both an acaricidal and ovicidal role, whereas ivermectin eradicates only hatched mites (13).
Permethrin was considered for many years to be the first classical scabies treatment option with high efficacy and patients’ compliance (13,31,32). However, in 2020 Meyersburg et al. conducted a single-center study, in which they observed lower cure rates for permethrin-treated classical scabies than they expected, hinting new populations of mites in Austria with resistance to permethrin (31).
BB and oral ivermectin are other common treatment options, promising excellent outcomes in classical scabies cases (13). Fortunately, a randomized study, published in 2023, comparing these two regimens, concluded that both are equally efficient and be used as a first-line treatment option safely (33).
Patients with crusted scabies, suffer from excessive amounts of mites on their skin and should be treated with both topical and systemic agents (13,34). The recommended anti-scabietic regimens are permethrin cream or BB lotion in combination with oral ivermectin (13,34). Permethrin 5% cream or BB 5% lotion should be administered every day for 1 week, followed by two times per week until cure (34). Alternatively, BB 25% lotion can be applied on days 1, 2, 8, 9 and 15 (11). Ivermectin tablets should be administered on days 1, 2, 8, 9 and 15 in a dose of 200 mcg/kg (11,13). Recalcitrant or extensively infected cases may require additional treatment cycles (34). Concomitant topical use of keratolytic agents such as salicylic acid or urea and moisturizers are recommended to remove crusts and scale (13,34).
It is noticeable that even contacts without any suspicious symptoms should be treated with anti-scabietic treatment (13). Guidelines suggest that even a single dosage of topical permethrin or oral ivermectin is effective (13).
Except for the classic treatment options, many clinical trials are in progress promising clear and realistic answers concerning new treatment options with easier patient compliance (13). Unfortunately, the scarcity of crusted scabies cases is an important obstacle, we need to overcome so as to draw statistically important conclusions for global control measures against the impact of scabies on human populations.
Conclusions
Crusted scabies is considered a neglected disease, with very few cases recorded, especially in high- and middle-income countries. Unfortunately, such findings have led to crusted scabies underdiagnosis, forcing patients to experience chronic disturbing symptoms and tremendously deteriorating their quality of life. Newer diagnostic tools including non-invasive dermoscopy or, even sometimes, a biopsy of the skin should always be part of our everyday clinical practice, as they can play a pivotal role in the diagnostic process.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-23-125/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-23-125/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-23-125/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Matthews A, Le B, Amaral S, et al. Prevalence of scabies and impetigo in school-age children in Timor-Leste. Parasit Vectors 2021;14:156. [Crossref] [PubMed]
- Romani L, Steer AC, Whitfeld MJ, et al. Prevalence of scabies and impetigo worldwide: a systematic review. Lancet Infect Dis 2015;15:960-7. [Crossref] [PubMed]
- Rigatos GA, Kappos-Rigatou I. Letter: Scabies in Greece. Arch Dermatol 1976;112:1466. [Crossref] [PubMed]
- Louka C, Logothetis E, Engelman D, et al. Scabies epidemiology in health care centers for refugees and asylum seekers in Greece. PLoS Negl Trop Dis 2022;16:e0010153. [Crossref] [PubMed]
- Bhat SA, Mounsey KE, Liu X, et al. Host immune responses to the itch mite, Sarcoptes scabiei, in humans. Parasit Vectors 2017;10:385. [Crossref] [PubMed]
- Meraz Soto JM, Alvarado Motte RA, Ramírez Carrillo P, et al. Crusted Hyperkeratotic Scabies: A Case Report. Cureus 2023;15:e34520. [PubMed]
- Olamiju B, Leventhal JS, Vesely MD. Crusted Scabies Presenting as Erythroderma in a Patient With Iatrogenic Immunosuppression for Treatment of Granulomatosis With Polyangiitis. Cutis 2023;111:E44-7. [Crossref] [PubMed]
- Li FZ, Chen S. Diagnostic Accuracy of Dermoscopy for Scabies. Korean J Parasitol 2020;58:669-74. [Crossref] [PubMed]
- Roberts LJ, Huffam SE, Walton SF, et al. Crusted scabies: clinical and immunological findings in seventy-eight patients and a review of the literature. J Infect 2005;50:375-81. [Crossref] [PubMed]
- Palaniappan V, Gopinath H, Kaliaperumal K. Crusted Scabies. Am J Trop Med Hyg 2021;104:787-8. [Crossref] [PubMed]
- Niode NJ, Adji A, Gazpers S, et al. Crusted Scabies, a Neglected Tropical Disease: Case Series and Literature Review. Infect Dis Rep 2022;14:479-91. [Crossref] [PubMed]
- Arlian LG, Vyszenski-Moher DL. Life cycle of Sarcoptes scabiei var. canis. J Parasitol 1988;74:427-30. [Crossref] [PubMed]
- Sunderkötter C, Wohlrab J, Hamm H. Scabies: Epidemiology, Diagnosis, and Treatment. Dtsch Arztebl Int 2021;118:695-704. [PubMed]
- Kutlu NS, Turan E, Erdemir A, et al. Eleven years of itching: a case report of crusted scabies. Cutis 2014;94:86-8, 95. [PubMed]
- Merad Y. Unexpected crusted scabies in an elderly woman without any immunosuppression. BMJ Case Rep 2021;14:e242310. [Crossref] [PubMed]
- Sluzevich JC, Sheth AP, Lucky AW. Persistent eosinophilia as a presenting sign of scabies in patients with disorders of keratinization. Arch Dermatol 2007;143:670-3. [Crossref] [PubMed]
- Engelman D, Yoshizumi J, Hay RJ, et al. The 2020 International Alliance for the Control of Scabies Consensus Criteria for the Diagnosis of Scabies. Br J Dermatol 2020;183:808-20. [Crossref] [PubMed]
- Park JH, Kim CW, Kim SS. The diagnostic accuracy of dermoscopy for scabies. Ann Dermatol 2012;24:194-9. [Crossref] [PubMed]
- Yoshizumi J, Harada T. 'Wake sign': an important clue for the diagnosis of scabies. Clin Exp Dermatol 2009;34:711-4. [Crossref] [PubMed]
- Fox G. Diagnosis of scabies by dermoscopy. BMJ Case Rep 2009;2009:bcr06.2008.0279.
- Grover C, Jakhar D. Dermoscopy in the Diagnosis of Scabies. Int J Dermoscop 2017;1:67-8. [Crossref]
- Walton SF, Beroukas D, Roberts-Thomson P, et al. New insights into disease pathogenesis in crusted (Norwegian) scabies: the skin immune response in crusted scabies. Br J Dermatol 2008;158:1247-55. [Crossref] [PubMed]
- Fernandez N, Torres A, Ackerman AB. Pathologic findings in human scabies. Arch Dermatol 1977;113:320-4. [Crossref] [PubMed]
- Navarini AA, Feldmeyer L, Töndury B, et al. The yellow clod sign. Arch Dermatol 2011;147:1350. [Crossref] [PubMed]
- Liu X, Walton SF, Murray HC, et al. Crusted scabies is associated with increased IL-17 secretion by skin T cells. Parasite Immunol 2014;36:594-604. [Crossref] [PubMed]
- Yang Y, Yoo HM, Choi I, et al. Interleukin 4-induced proliferation in normal human keratinocytes is associated with c-myc gene expression and inhibited by genistein. J Invest Dermatol 1996;107:367-72. [Crossref] [PubMed]
- Mosca M, Hong J, Hadeler E, et al. The Role of IL-17 Cytokines in Psoriasis. Immunotargets Ther 2021;10:409-18. [Crossref] [PubMed]
- Liu JM, Lin CY, Chang FW, et al. Increased risk of psoriasis following scabies infection: A nationwide population-based matched-cohort study. J Dermatol 2018;45:302-8. [Crossref] [PubMed]
- Abd El-Aal AA, Hassan MA, Gawdat HI, et al. Immunomodulatory impression of anti and pro-inflammatory cytokines in relation to humoral immunity in human scabies. Int J Immunopathol Pharmacol 2016;29:188-94. [Crossref] [PubMed]
- Hasan T, Krause VL, James C, et al. Crusted scabies; a 2-year prospective study from the Northern Territory of Australia. PLoS Negl Trop Dis 2020;14:e0008994. [Crossref] [PubMed]
- Meyersburg D, Kaiser A, Bauer JW. 'Loss of efficacy of topical 5% permethrin for treating scabies: an Austrian single-center study'. J Dermatolog Treat 2022;33:774-7. [Crossref] [PubMed]
- Hamm H, Beiteke U, Höger PH, et al. Treatment of scabies with 5% permethrin cream: results of a German multicenter study. J Dtsch Dermatol Ges 2006;4:407-13. [Crossref] [PubMed]
- Meyersburg D, Welponer T, Kaiser A, et al. Comparison of topical benzyl benzoate vs. oral ivermectin in treating scabies: A randomized study. J Eur Acad Dermatol Venereol 2023;37:160-5. [Crossref] [PubMed]
- Widaty S, Miranda E, Cornain EF, et al. Scabies: update on treatment and efforts for prevention and control in highly endemic settings. J Infect Dev Ctries 2022;16:244-51. [Crossref] [PubMed]
Cite this article as: Alexandris D, Alevizopoulos N, Nennes P, Basagianni E, Rousou P, Kioupi M, Gerakini F. Case report of crusted scabies, brief review of its pathophysiology and latest data. AME Case Rep 2024;8:30.


