
Acute pancreatitis caused by gastric balloon: a case report
Highlight box
Key findings
• In this report, we report a case of gastric balloon pancreatitis, which is a rare complication after intragastric balloon (IGB) insertion.
What is known and what is new?
• The diagnosis is based on laboratory and imaging tests, and on exclusion of other causes of pancreatitis. There have only been 39 cases with gastric balloon pancreatitis published so far, however, the prevalence may be higher.
• Many cases may probably remain undetected due to lack of specific symptoms.
What is the implication, and what should change now?
• Lipase/amylase levels should be measured and adequate imaging should be performed in patients with IGB and relevant abdominal pain as not to misinterpret the symptoms as gastric distension or oesophagitis.
Introduction
Obesity is increasing worldwide causing relevant moralities and morbidities. Intragastric balloon (IGB) insertion is a safe and effective method commonly used as a bridging therapy prior bariatric surgery, but also as a primary weight loss strategy in case of failed dietary changes, lifestyle modification and medical therapy. Implanting a balloon device in the stomach helps with weight loss by generating a sense of fullness and reducing the volume available for food (1). A weight reduction of approximately 15–20% of total body weight can be reached (2).
The method is considered to have a low morbidity and mortality; however diverse complications may occur. Mild side effects such as nausea, abdominal pain and gastroesophageal reflux are not uncommon after insertion, but also some life-threatening complications including ulceration, perforation and bowel obstruction have been reported (3). Pancreatitis due to IGB insertion is a rare complication, 39 cases have been published so far. We present this article in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-23-171/rc).
Case presentation
A 28-year-old female patient with a body mass index (BMI) of 28.3 kg/m2 presented to our emergency department with a sudden onset of upper abdominal pain with a duration of 2 hours. The balloon (Spatz3 Adjustable Balloon System; Spatz FGIA, Great Neck, NY, USA) was inserted and filled with 500 mL saline 9 months earlier in another country. Her BMI was 35.5 kg/m2 before the balloon treatment, she has reached a total body weight reduction of 20 kg. On a 4-month follow-up, the balloon was well tolerated and the patient didn’t experience any weight loss plateau, so there was no endoscopic balloon adjustment performed. Her medical history was otherwise unremarkable, alcohol consumption was denied, and she was on no medications. On physical examination, the patient was afebrile and hemodynamically stable. The abdominal palpation revealed severe tenderness at the epigastric and left hypochondric regions. Initial laboratory workup showed no abnormalities. 12 hours later, however, a leukocytosis (12.3×109/L), slightly elevated C-reactive protein level (22 mg/dL) and lactate dehydrogenase (LDH) (290 U/L) could be detected, and both lipase (423 U/L) and amylase (204 U/L) levels were over 3× above the normal range. Triglyceride, cholesterol, immunoglobulin G4 (IgG4) and calcium levels were normal.
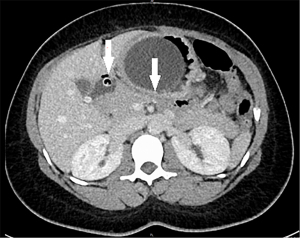
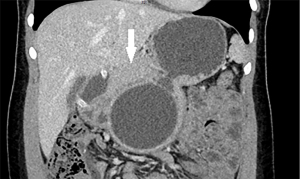
An abdominal ultrasound on admission was negative for cholelithiasis, sludge in the gall bladder, as well as for common bile duct (CBD) or intrahepatic bile duct dilatation. In regard to the severe abdominal pain and tenderness, an urgent intravenous contrast enhanced abdominal computed tomography (CT) was performed to exclude gastric perforation or bowel obstruction. The balloon could be seen slightly compressing the body of the pancreas without any pancreatic duct dilatation, the catheter of the balloon showed to be dislodged into the duodenum. There was no inhomogeneity of the pancreatic parenchyma or pancreatic fluid collection visible. No CBD or intrahepatic bile duct dilation could be detected, supporting the ultrasound findings. Other major complications such as perforation or relevant gastric ulceration could also be excluded (Figures 1-3).

Intravenous fluid replacement was carried out as recommended in current guidelines. For analgesia were 2×20 mg morphine hydrochloride and 3×1 g metamizole administered intravenously in the first 24 hours. Although the symptoms improved significantly for the second day, we decided for the endoscopic removal of the balloon. Thereafter, the patient showed further fast clinical recovery with the normalization of laboratory parameters in 4 days after admission. We repeated the abdominal ultrasound scan on the third day, which showed no abnormality of the pancreas or the peripancreatic region, so that we could assess a mild form of pancreatitis according to the revised Atlanta criteria. During a follow-up of 12 months no other episode of pancreatitis occurred, routine laboratory tests and ultrasound 6 weeks after discharge were also without any pathologic findings.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
IGB therapy has been used since 1985 as an effective minimally invasive technique in the treatment of obesity. Acute pancreatitis is a rare complication of the method. The first case was reported in 2008 by Mohammed et al. (4), followed by 20 other publications (5-24) (Table 1), mainly with 1 or 2 cases and some case series with 4–10 patients. In last few years, there have been significantly more balloon pancreatitis cases published than before. There may be a higher prevalence, many cases may probably remain undetected due to lack of specific symptoms and without performing laboratory and imaging tests. Upper abdominal pain in patients with IGB is a nonspecific symptom, mainly caused by gastroesophageal reflux or gastric outlet obstruction. In the case of our patient, the first laboratory test was performed 2 hours after the onset of the abdominal pain, showing no abnormalities. Repeated blood analysis 12 hours later led us to the diagnosis of pancreatitis. Cross-sectional imaging with contrast enhancement is crucial to assess the severity of the pancreatitis and to exclude other complications such as balloon migration or perforation. In most of the published cases, the pancreatitis appeared in a mild edematous form. In some patients, the balloon could be left on site and it came to a quick clinical and biochemical recovery under a conservative treatment. In the case of our patient, we could also observe a fast relief of the abdominal pain, but regard to the ongoing balloon treatment period of 9 months, and in order to prevent a next episode of pancreatitis, we decided the removal of the device.
Table 1
| 1st author | Title of publication | Year of publication | Number of cases |
|---|---|---|---|
| Mohammed AE (4) | Acute pancreatitis complicating intragastric balloon insertion | 2008 | 1 |
| Shelton E (5) | Education and Imaging. Gastrointestinal: balloon pancreatitis | 2012 | 1 |
| Vongsuvanh R (6) | Acute necrotizing pancreatitis, gastric ischemia, and portal venous gas complicating intragastric balloon placement | 2012 | 1 |
| Geffrier C (7) | Acute “balloon pancreatitis” | 2014 | 1 |
| Navajas-Laboa M (8) | Intragastric balloon and epigastric pain: beware of the pancreas | 2015 | 1 |
| Öztürk A (9) | A case of duodenal obstruction and pancreatitis due to intragastric balloon | 2015 | 1 |
| Selfa Muñoz A (10) | Acute pancreatitis associated with the intragastric balloon | 2016 | 1 |
| Issa I (11) | Acute pancreatitis caused by intragastric balloon: A case report | 2016 | 1 |
| Said F (12) | Pancreatitis and intragastric balloon insertion | 2016 | 1 |
| Aljiffry M (13) | Acute pancreatitis: a complication of intragastric balloon | 2017 | 4 |
| Gore N (14) | Pancreatitis from intra-gastric balloon insertion: Case report and literature review | 2018 | 1 |
| Alsohaibani FI (15) | Acute Pancreatitis as a Complication of Intragastric Balloons: a Case Series | 2019 | 10 |
| Barrichello S (16) | Acute pancreatitis due to intragastric balloon hyperinflation | 2020 | 1 |
| Halpern B (17) | Extrinsic compression of pancreactic duct by intragastric balloon treatment and its potential to cause acute pancreatitis: two case reports and clinical discussion | 2020 | 2 |
| Alqabandi O (18) | Intragastric balloon insertion and pancreatitis: Case series | 2020 | 5 |
| Abdulghaffar S (19) | Acute pancreatitis as a late complication of intra-gastric balloon insertion | 2021 | 1 |
| Schwingel J (20) | Acute Pancreatitis Following Insertion of a Gastric Balloon-an Unusual Cause | 2021 | 1 |
| Al Ghadeer HA (21) | Acute pancreatitis as a complication of intragastric balloon | 2021 | 2 |
| Chirinos Vega JA (22) | Intra-gastric balloon associated with acute pancreatitis | 2022 | 1 |
| Akiki L (23) | Acute Pancreatitis as a Complication of an Intragastric Balloon | 2023 | 1 |
| Al Refai F (24) | Acute Pancreatitis Secondary to Intragastric Balloon: A Case Report and Literature Review | 2023 | 1 |
We suppose an association between the balloon insertion and the acute pancreatitis. A possible pathogenesis for the inflammation may be a direct compression and traumatic effect on the pancreas by the balloon. However, in some other publications (9,13,21) was the dislodgement of the catheter into the duodenum—like in the case of our patient—also mentioned as a possible causal factor due to an obstruction/compression of the Papilla.
This report has some limitations to determine the strength of association between gastric balloon insertion and pancreatitis. Endoscopic ultrasound (EUS) was not performed to exclude microlithiasis of the CBD, however, at absence of gallbladder stones/sludge, normal CBD diameter and normal cholestatic parameters, a biliary cause is rather unlikely. Magnetic resonance cholangiopancreatography (MRCP) was not performed for pancreas divisum, and we didn’t use genetic testing to exclude an autoimmune etiology.
Conclusions
Acute pancreatitis associated with IGB insertion is a rare complication, the incidence is probably underreported. We suggest measuring lipase/amylase levels besides routine laboratory tests and performing adequate imaging in patients with IGB and relevant abdominal pain as not to misinterpret the symptoms as gastric distension or oesophagitis. Further research and analysis of more reported cases is needed to identify potential risk factors (balloon type, size, shape, volume) to possibly prevent this complication.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-23-171/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-23-171/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-23-171/coif). The authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Peker Y, Coskun H, Bozkurt S, et al. Comparison of results of laparoscopic gastric banding and consecutive intragastric balloon application at 18 months: a clinical prospective study. J Laparoendosc Adv Surg Tech A 2011;21:471-5. [Crossref] [PubMed]
- Imaz I, Martínez-Cervell C, García-Alvarez EE, et al. Safety and effectiveness of the intragastric balloon for obesity. A meta-analysis. Obes Surg 2008;18:841-6. [Crossref] [PubMed]
- Yorke E, Switzer NJ, Reso A, et al. Intragastric Balloon for Management of Severe Obesity: a Systematic Review. Obes Surg 2016;26:2248-54. [Crossref] [PubMed]
- Mohammed AE, Benmousa A. Acute pancreatitis complicating intragastric balloon insertion. Case Rep Gastroenterol 2008;2:291-5. [Crossref] [PubMed]
- Shelton E, Froomes P, Fink MA. Education and Imaging. Gastrointestinal: balloon pancreatitis. J Gastroenterol Hepatol 2012;27:986. [Crossref] [PubMed]
- Vongsuvanh R, Pleass H, van der Poorten D. Acute necrotizing pancreatitis, gastric ischemia, and portal venous gas complicating intragastric balloon placement. Endoscopy 2012;44 Suppl 2 UCTN:E383-4.
- Geffrier C, Samaha E, Duboc H. Acute "balloon pancreatitis". Endoscopy 2014;46 Suppl 1 UCTN:E383.
- Navajas-Laboa M, Bridet L, Orive-Calzada A, et al. Intragastric balloon and epigastric pain: beware of the pancreas. Turk J Gastroenterol 2015;26:87-8. [Crossref] [PubMed]
- Öztürk A, Yavuz Y, Atalay T. A Case of Duodenal Obstruction and Pancreatitis Due to Intragastric Balloon. Balkan Med J 2015;32:323-6. [Crossref] [PubMed]
- Selfa Muñoz A, Calzado Baeza SF, Palomeque Jiménez A, et al. Acute pancreatitis associated with the intragastric balloon. Gastroenterol Hepatol 2016;39:603-4. [PubMed]
- Issa I, Taha A, Azar C. Acute pancreatitis caused by intragastric balloon: A case report. Obes Res Clin Pract 2016;10:340-3. [Crossref] [PubMed]
- Said F, Robert S, Mansour EK. Pancreatitis and intragastric balloon insertion. Surg Obes Relat Dis 2016;12:e33-4. [Crossref] [PubMed]
- Aljiffry M, Habib R, Kotbi E, et al. Acute Pancreatitis: A Complication of Intragastric Balloon. Surg Laparosc Endosc Percutan Tech 2017;27:456-9. [Crossref] [PubMed]
- Gore N, Ravindran P, Chan DL, et al. Pancreatitis from intra-gastric balloon insertion: Case report and literature review. Int J Surg Case Rep 2018;45:79-82. [Crossref] [PubMed]
- Alsohaibani FI, Alkasab M, Abufarhaneh EH, et al. Acute Pancreatitis as a Complication of Intragastric Balloons: a Case Series. Obes Surg 2019;29:1694-6. [Crossref] [PubMed]
- Barrichello S, de Moura DTH, Hoff AC, et al. Acute pancreatitis due to intragastric balloon hyperinflation (with video). Gastrointest Endosc 2020;91:1207-9. [Crossref] [PubMed]
- Halpern B, Paulin Sorbello M, Telles Libanori H, et al. Extrinsic compression of pancreactic duct by intragastric balloon treatment and its potential to cause acute pancreatitis: two case reports and clinical discussion. Obes Res Clin Pract 2020;14:191-3. [Crossref] [PubMed]
- Alqabandi O, Almutawa Y, AlTarrah D, et al. Intragastric balloon insertion and pancreatitis: Case series. Int J Surg Case Rep 2020;74:263-7. [Crossref] [PubMed]
- Abdulghaffar S, Badrawi N, Gowda SK, et al. Acute pancreatitis as a late complication of intra-gastric balloon insertion. J Surg Case Rep 2021;2021:rjab139. [Crossref] [PubMed]
- Schwingel J, Hüttinger S, Lutz M. Acute Pancreatitis Following Insertion of a Gastric Balloon-an Unusual Cause. Dtsch Arztebl Int 2021;118:846. [Crossref] [PubMed]
- Al Ghadeer HA, AlFuraikh BF, AlMusalmi AM, et al. Acute Pancreatitis as a Complication of Intragastric Balloon. Cureus 2021;13:e16710. [Crossref] [PubMed]
- Chirinos Vega JA, Cabrera-Hinojosa D. Intra-gastric balloon associated with acute pancreatitis. Rev Gastroenterol Peru 2022;42:183-7. [Crossref] [PubMed]
- Akiki L, Alomary A. Acute Pancreatitis as a Complication of an Intragastric Balloon. Cureus 2023;15:e38094. [Crossref] [PubMed]
- Al Refai F, Khalil SK, Khalil SK, et al. Acute Pancreatitis Secondary to Intragastric Balloon: A Case Report and Literature Review. Cureus 2023;15:e45230. [Crossref] [PubMed]
Cite this article as: Gyimesi G, Widmer F, Sulz MC. Acute pancreatitis caused by gastric balloon: a case report. AME Case Rep 2024;8:45.


