Thoracic aortic aneurysm in an adolescent with intraoperative discovery of contained rupture: a case report
Highlight box
Key findings
• Adolescent thoracic aortic aneurysms may be prone to rupture prior to indications for surgery.
What is known and what is new?
• Criteria for adult aortic aneurysm surgical indications continues to evolve with decreasing size threshold. There are several known obstacles to establishing criteria in children and adolescents.
• This case provides a clinical example of why it is important to establish criteria for adolescent aortic aneurysm operative indications.
What is the implication, and what should change now?
• Definitive guidelines should be established beyond size criteria for adolescents with thoracic ascending aortic aneurysms in order to decrease the risk of rupture.
Introduction
Background
In 2022, the American Heart Association updated aortic disease management guidelines. The most notable change was lowering the threshold for thoracic ascending aortic aneurysm size to 5.0 from 5.5 cm (1).
Rationale and knowledge gap
As recommendations in adults become more refined, criteria for surgical intervention in childhood/adolescence in association with inheritable syndromes remains less established (2). Complicating clinical decision-making is the increased evidence of genetic predisposition to aortic dissection at diameters <5.0 cm (3).
Objective
Our adolescent case presentation, based on an unexpected intraoperative finding of contained aortic rupture with a unicuspid aortic valve (AV), highlights the challenge of determining precisely when to proceed with aortic root replacement in this patient population. We present this case in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-23-163/rc).
Case presentation
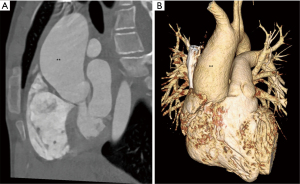
A 15-year-old, 57 kg male with known valvar aortic stenosis, unicuspid AV, dilated aortic root and thoracic aortic aneurysm (TAA) presented for routine follow-up. He had an episode of chest pain 1 year prior, which self-resolved. There was no relevant family history of congenital heart disease or connective tissue disease. Transthoracic echocardiogram (TTE) demonstrated a unicuspid AV with stable moderate stenosis (peak gradient, 67 mmHg), mild regurgitation, normal left ventricle (LV) size and function, and ascending aorta 39 mm (z-score, >6). The aortic dimensions increased over time: 3 mm/2 years. On computed tomographic angiography (CTA), the mid-ascending aorta measured 41 mm (z-score, >8), severely aneurysmal, with proximal ascending aorta 32 mm (Figure 1). Given the size and progression of the aorta, he was referred for surgical repair. After discussion of valve and root replacement options with the family, the decision was made to proceed with a mechanical valve.
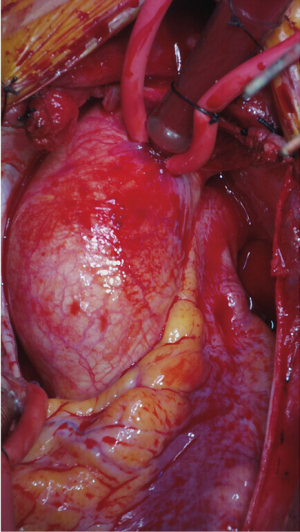
The patient underwent an aortic root replacement using mechanical AV composite graft 21 mm with coronary artery reimplantation (modified Bentall) and ascending hemiarch replacement (24 mm graft) under deep hypothermic circulatory arrest (DHCA) with retrograde cerebral perfusion (Figure 2, Video 1). Routine monitoring was performed with an arterial/central line, foley, and electroencephalogram/somatosensory evoked potentials. Median sternotomy and central cannulation were performed. Cardioplegia was administered into the aortic root. Upon transection of the aorta, an old hematoma was visible along the medial, posterior aspect near the main pulmonary artery. There was a small intimal tear, suggesting a contained, remote perforation. The AV was functionally unicuspid/bicuspid and not repairable (Figure 3). Total bypass time was 154 minutes, cross-clamp time 117 minutes, with DHCA 13 minutes. The patient tolerated the procedure well. Post-bypass echo demonstrated good valve function with no perivalvar leak and excellent cardiac function.

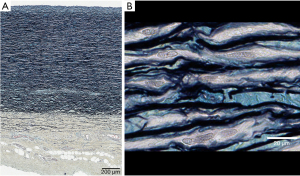
Post-operatively, there were no major complications. He was started on heparin for bridging therapy to coumadin [international normalized ratio goal 2–3]. He was discharged on post-operative day 11. On 6-month follow-up, his mechanical valve is well functioning with mild regurgitation laterally, most likely due to washing jets. A representative slide of the aortic tissue demonstrates normal histology in terms of wall thickness and organization (Figure 4). There is no evidence of myxoid degeneration or elastic fiber degradation. Genetic analysis resulted in a heterozygous missense variant of uncertain significance in PTPN11. This mutation is typically associated with Noonan syndrome and not known to be associated with aortopathy (4).
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient’s parent for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Key findings
This case highlights multiple important factors when considering surgical repair for TAA in adolescents: atypical genetic syndromes, association with bicuspid AV (BAV), size <4.0 cm, and intraoperative contained rupture.
Strengths and limitations
As an isolated case report, there are limitations to generalizability of this specific case. And, given the unknown timeframe for when the patient experienced the contained aortic rupture, it is still unclear at exactly what size the aorta was at the time of rupture. We also did not have advanced imaging such as four-dimensional (4-D) flow magnetic resonance imaging (MRI). However, this intraoperative finding gives a unique clinical example of establishing improved criteria beyond size for evaluating adolescents with dilated ascending aortas.
Comparison with similar research
In evaluating BAV adult patients, a higher proportion require operative intervention at a younger age, presented with a smaller aorta (4.6 cm) and more rapid rate of growth (1.9 mm/year), compared to TAA without BAV (5). BAV is also associated with childhood TAA; it is unclear whether this predisposes to dissection at smaller diameters prior to adulthood (2). BAV genetic mutations could become a surrogate marker for early, progressive TAA. The intricate relationship between genetic mutations, aortic dissection, and aorta sizes continues to be explored (3).
Specifically, in regards to younger male adult BAV patients, AV size and function may be a poor surrogate for intrinsic aortic properties (6). The loss of elastic fibers with aortic wall stiffness can be diagnosed irrespective of aortic wall dilation. This was observed in patients with no or mild AV impairment. Usage of serial echographic measurements may allow earlier identification and guide medical/surgical intervention of potentially modifiable risk factors. These observations continue to establish that only aortic size in younger patients may be an inadequate parameter to address what changes are occurring in the aortic wall in BAV patients that can predispose to rupture.
Although connective tissue disease such as Marfan syndrome and Loeys-Dietz syndrome are known to have an association with TAA leading patients to early dissection/rupture, this represents the minority of patients [i.e., Marfan disease only constitutes 5% of TAA patients (7)]. There is still much to learn about the true inheritability of aortopathy beyond connective tissue disorders. At the Yale Aortic Institute, Elefteriades (7), with mapping almost 500 family trees for TAA patients, discovered that at least 21% have at least one family member with a known TAA. These positive findings in familial relatives also demonstrated a higher growth rate and earlier age of presentation. It is likely that the pattern of inheritance is predominantly autosomal dominant, but more research will need to be done in order to elucidate the precise rate and method of inheritance.
Explanation of findings
Current guidance regarding intervention in adult TAA, based on size, also continues to change (1). Additionally, 4-D flow MRI measures different parameters in the ascending aorta with BAV to increase the dimensions of understanding beyond only 2-D size criteria (8). This newer imaging modality measures peak velocity, ascending aortic root z-scores, and regional wall shear stress, which may offer insight into predictors of growing aortas (9). Even more exciting is the ability to measure flow patterns after surgical interventions which may guide choice of prosthesis or design—for example, eccentric flow patterns in BAV patients were seen after tissue valve implantation, but not with mechanical valves (8). Also, in 4-D flow MRIs in pediatric patients with BAV, there was a correlation between ascending aortic root z-scores (3.12±2.62 vs. 3.59±2.76, P<0.05) and baseline peak velocity as a predictor of ascending aortic root dilation (9).
Implications and actions needed
Our patient’s genetic results demonstrate a need for further testing in order to better understand the natural history and clinical implications for congenital aortic diseases. The complex relationship between genetic heritability, aortic pathology, aortic rupture/dissection, and aorta size continues to be studied with further research necessary (3,6).
As 4-D flow MRI imaging becomes more advanced, this allows us to increase surveillance and understanding of the aorta at local/regional levels of wall stress (8). Especially for pediatric patients, this non-invasive imaging that provides increased dimensionality for further understanding of the aorta is exciting. Larger patient volumes and studying different regional populations with ascending aortic disease will allow generalizability of these results.
Currently, indications for surgery in ascending aortic disease are limited by absolute size and rate of growth in adult patients. Some alternative ideas to categorize age-adjusted risk include z-scores, rate of growth, or a calculation of aortic root to descending aorta ratio. Ultimately, creating a mathematical model to predict a patient’s risk of rupture would be the ideal tool. Our intraoperative findings of a contained rupture suggest that offering surgery earlier in this patient would have been appropriate. In the future, a similar 15-year-old patient with aortic morphology should have improved guidelines with data to indicate an earlier indication for surgery in order to prevent rupture.
Conclusions
In summary, definitive guidance for optimal timing of surgery for TAA and BAV in childhood/adolescence remains deficient. Obstacles to identifying appropriate criteria and eligible patients include lower volume, lack of availability of genetic sequencing, and variability in clinical presentation. As guidelines develop to include more aortic parameters (8,9), biomarkers, tissue biorepositories, genetic mutations, and environmental factors for dissection (7) the treatment of TAA in childhood/adolescence will continue to improve.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-23-163/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-23-163/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-23-163/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient’s parent (patient is a minor) for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Writing Committee Members. 2022 ACC/AHA Guideline for the Diagnosis and Management of Aortic Disease: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol 2022;80:e223-393. [PubMed]
- Zanotti G, Vricella L, Cameron D. Thoracic aortic aneurysm syndrome in children. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 2008;11-21. [Crossref] [PubMed]
- Ostberg NP, Zafar MA, Ziganshin BA, et al. The Genetics of Thoracic Aortic Aneurysms and Dissection: A Clinical Perspective. Biomolecules 2020;10:182. [Crossref] [PubMed]
- Linglart L, Gelb BD. Congenital heart defects in Noonan syndrome: Diagnosis, management, and treatment. Am J Med Genet C Semin Med Genet 2020;184:73-80. [Crossref] [PubMed]
- Borger MA, Fedak PWM, Stephens EH, et al. The American Association for Thoracic Surgery consensus guidelines on bicuspid aortic valve-related aortopathy: Full online-only version. J Thorac Cardiovasc Surg 2018;156:e41-74. [Crossref] [PubMed]
- Nistri S, Grande-Allen J, Noale M, et al. Aortic elasticity and size in bicuspid aortic valve syndrome. Eur Heart J 2008;29:472-9. [Crossref] [PubMed]
- Elefteriades JA, Farkas EA. Thoracic aortic aneurysm clinically pertinent controversies and uncertainties. J Am Coll Cardiol 2010;55:841-57. [Crossref] [PubMed]
- Cave DGW, Panayiotou H, Bissell MM. Hemodynamic Profiles Before and After Surgery in Bicuspid Aortic Valve Disease-A Systematic Review of the Literature. Front Cardiovasc Med 2021;8:629227. [Crossref] [PubMed]
- Rose MJ, Rigsby CK, Berhane H, et al. 4-D flow MRI aortic 3-D hemodynamics and wall shear stress remain stable over short-term follow-up in pediatric and young adult patients with bicuspid aortic valve. Pediatr Radiol 2019;49:57-67. [Crossref] [PubMed]
Cite this article as: Lee ME, Boules H, Steele J, Asnes J, Assi R. Thoracic aortic aneurysm in an adolescent with intraoperative discovery of contained rupture: a case report. AME Case Rep 2024;8:36.