
Leptomeningeal metastasis of breast cancer during neo-adjuvant chemotherapy in a 38-year-old woman: a case report
Highlight box
Key findings
• Leptomeningeal metastasis (LM) from breast cancer should be given sufficient vigilance and attention at the beginning of the diagnosis and treatment, particularly in triple-negative breast cancer patients who are at high risk.
What is known and what is new?
• LM is a rare but aggressive metastatic diagnosis with poor outcome.
• Symptoms of LM may be masked by the neo-chemotherapy adverse effects, and the results of magnetic resonance imaging and computed tomography may show negative results.
What is the implication, and what should change now?
• Lumbar puncture with cerebrospinal fluid should be done promptly if LM is highly suspected in clinical practice. Various treatment modalities including intrathecal thiotepa, oral temozolomide and whole-brain radiation therapy didn’t show significant benefit for survival. Early prevention, early detection and timely treatment are crucial.
Introduction
Breast cancer accounts for 5% of the population (male and female) who develop central nervous system (CNS) metastasis, which is only second to the lung cancer (1). The incidence of CNS metastasis differs by molecular subtype, which is hormone receptor (HR)+/human epidermal growth factor receptor 2 (HER2)− (45.3%), HR+/HER2+ (14.5%), HR−/HER2+ (14.9%) and triple-negative (25.4%) (2). Breast cancer metastasis to the brain including parenchymal brain metastasis (BM) and leptomeningeal metastasis (LM), while molecular and cellular mechanisms can’t explain the difference currently. LM is a rare but very aggressive metastatic diagnosis with poor outcome. A recent study from India reported the median time to develop LM from the time of diagnosis of breast cancer was 6 months and the median overall survival (OS) was 3 months (3). This case report reported a 38-year-old woman developed LM during neo-adjuvant chemotherapy. Various treatment modalities had been used in clinical practice, but none of them showed significant benefit for survival. We present this article in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-23-116/rc).
Case presentation
Patient history and presentation
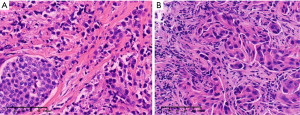
A 38-year-old Chinese female presented to the neurology department due to progressive headache for 1 month, accompanied with dizziness, nausea, vomiting and neck pain. During hospitalization, she experienced paroxysmal loss of consciousness twice, which were considered as symptomatic epilepsy. Five months prior to this visit, her first visit was diagnosed with breast cancer on the right side which is of triple-negative subtype and with homolateral axillary lymph node involvement by biopsy. She denied the existence of a family history of cancer, including breast or ovarian cancer, and there was no individual history of head trauma or craniotomy. After the clinician assessment she had received six cycles of TCb neo-adjuvant chemotherapy. During the period of neo-adjuvant chemotherapy, she did not report the presence of severe neurological symptoms. Twenty days ago, she underwent right breast-conserving surgery with homolateral axillary lymph node dissection in the breast surgery department of our hospital. The preoperative breast magnetic resonance imaging (MRI) suggested significant mass reduction. The surgery went well with complete removal of the mass (Figure 1A) and negative margin status. Postoperative evaluation of the patient’s breast cancer was ypT1N3M0 stage and Miller-Payne grade 2. The postoperative pathological results of all the 44 examined lymph nodes were positive (Figure 1B), which predicted a poor outcome for the patient. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Publication of this case report and accompanying images was waived from patient consent according to the ethics committee of the Second Affiliated Hospital, Zhejiang University School of Medicine (Approval No. 2023LSYD0864).
Diagnostic workup
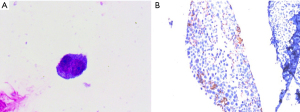
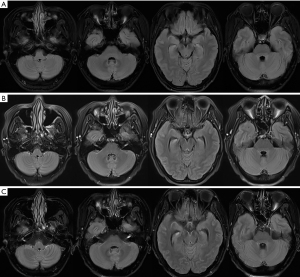
Neo-adjuvant chemotherapy reduced the tumor size (Figure 2) and enabled total tumor resection. Neurological examination showed a normal mental state, bilateral peripheral facial paralysis, left abducens nerve paralysis, a leftward horizontal nystagmus, neck rigidity and slight ataxia. Head computed tomography (CT) scans found no significant brain imaging changes. Further, the patient underwent three contrast-enhanced MRI scans of the head, but there was still no typical high signal intensity of meninges or brain parenchyma. Finally, lumbar puncture with cerebrospinal fluid (CSF) analysis showed the presence of malignant cells (Figure 3A). The expression of programmed cell death 1 ligand 1 (PD-L1) in the tumor sample was positive (Figure 3B). Given the patient’s clinical history and new neurologic symptoms, the diagnosis was LM from breast cancer.

Medical management and treatment
The patient was transferred to the radiotherapy department for further treatment. As the symptomatic treatment, mannitol, glycerol fructose and dexamethasone were used to lower the intracranial pressure. Antineoplastic drug therapy included intrathecal thiotepa 10 mg once for six times and concomitant oral temozolomide (TMZ). Whole-brain radiation therapy (WBRT) [6 MV X-ray, D95 planning target volume (PTV), 30 Gy/10 fractions] was used to treat LM. She was given antiepileptic treatment with levetiracetam and lacosamide. The patient had good adherence and tolerability of the treatment. However, all the treatment did not significantly release her neurological symptoms or prolong the survival. Her symptoms worsened rapidly after the diagnosis of LM, and the pain of head and neck was never relieved. She could walk normally after breast surgery at first, but after that she was confined to the wheelchair in a few weeks. The patient survived for only 5 months after being diagnosed with LM.
Discussion
The patient in this case was a 38-year-old young woman with aggressive triple-negative breast cancer (TNBC) of high risk. Although the patient had received neo-adjuvant chemotherapy, the LM still occurred and progressed rapidly. Doctors had tried the best to treat her, but the limited therapeutic options available make the prognosis abysmal. Her neurological symptoms ranged from brain parenchyma involvement, meningeal irritation syndromes, cranial nerve involvement, and progressive brain dysfunction. The patient’s clinical presentation accord with the diagnosis of LM. However, such a rapid progression made us wonder if it was true that patients’ LM metastasis progressed so aggressive and fast. Another possibility was that we had ignored some of the atypical symptoms that patients exhibited in the early stages of the disease. Actually, it was difficult to distinguish from the adverse effects of chemotherapy including headache, dizziness, nausea and vomiting, if patient not paying attention to these symptoms in the early stages. The diagnosis of LM is most commonly made by clinical evaluation, CSF cytology and brain imaging (4). MRI is the imaging modality of choice for BM and LM patients, because of its radiation-free, high-resolution soft-tissue imaging and high sensitivity. According to the current study, contrast-enhanced MRI is the technique of choice to evaluate patients with leptomeningeal diseases (5). Although CT has a significantly lower sensitivity than MRI, it remains valuable for patients who have contraindications to MRI. In cases where MRI is consistently negative while the clinical symptoms are very obvious, there are other auxiliary inspections besides CSF that can be used, such as positron emission tomography (PET)-CT and liquid biopsy. PET-CT allows the collection of anatomical and metabolic information, which is valuable in assessing systemic tumor load and can be used as a complement to MRI. Liquid biopsy including circulating tumor cells (CTCs) and cell-free DNA (cfDNA) has been used as an auxiliary inspection method for the diagnosis of breast cancer metastasis. However, its clinical application for the diagnosis of LM, needs further validation (6).
We really concerned the case of this patients and went through several multidisciplinary treatment (MDT) discussion for this case. It was found that much attention was paid on the patient’s MRI of the meninges and brain parenchyma (Figure 4), which presented no obvious imaging manifestation. With the help of the radiologist who was expert in nervous system imaging, enhancement was faintly visible in cerebellar sulcus, basal cistern level, internal auditory canal, brainstem and trigeminal nerve, at the time of third MRI on October 26 (Figure 4C). However, this enhancement was usually non-specific which can be observed not only in cancer but also in infectious diseases. Therefore, when interpreting the results of MRI, clinicians need to closely combine the patient’s clinical features to make the interpretation more consistent with the case.
For most patients, the goal of therapy of breast cancer metastasis to the brain is to prevent or delay neurological deterioration and to improve the quality of life. European Association of Neuro-Oncology (EANO)-European Society for Medical Oncology (ESMO) guidelines recommend local (surgery and radiotherapy) and systemic treatment as the main treatment strategy, and the main contents include: (I) WBRT and stereotactic radiotherapy (SRT) are the most used radiotherapy methods. (II) WBRT is used in patients with extensive linear lesions, and intrathecal injection therapy is used in patients with pathological confirmed CSF cancer cells. (III) Systemic medical treatment, including capecitabine and TMZ, is also an optional treatment in combination with radiotherapy. (IV) HER2+ patients with BM were particularly likely to benefit from HER2 targeted therapy (7). However, there is no standard treatment for LM patients. The main challenge of brain disease therapy is the blood-brain barrier, radiation therapy can disrupt the blood-brain barrier to increase drug permeation into brain. It was reported that OS of patients with LM could be improved by concomitant systemic therapy (except TNBC) and the use of intrathecal methotrexate (rather than cytarabine or thiotepa) (8). In this case, the neuro symptoms were stable for a month after radiotherapy and intrathecal injection therapy, but soon deteriorated. Any subsequent treatment with medication was ineffective. TMZ is first-line treatment for recurrent BM. Melisko et al. found the combination of irinotecan and TMZ had modest clinical activity and was well tolerated in patients with breast cancer and progressing CNS disease (9). TMZ in combination with T-DM1 shows low-grade toxicity and potential activity in secondary prevention of HER2+ patients’ BM (10). TNBC lacks a standardized treatment approach. As the current therapies for TNBC lack the effectiveness to improve patients’ survival, it is crucial to develop novel treatments (11). Personalized immunotherapy could also be considered for the TNBC patients with LM, but the effectiveness needs to be supported by more study in the future (12). Although the patient’s expression of PD-L1 was positive, she didn’t receive immunotherapy, probably due to financial consideration.
A meta-analysis showed that the incidence of metastasis to the brain among patients with HER2+ and triple-negative disease was higher than HR+/HER2− (13). It was reported that OS was independently associated with subtypes: median OS was 18.9 months for HR+/HER2+, 13.1 months for HR−/HER2+, 7.1 months for HR+/HER2− and 4.4 months for triple-negative patients (2). In patients with ER+/HER2− advanced breast cancer, those in the LM group were more likely to die from worsening CNS lesions and had worse prognosis than BM (14). TNBC strongly associated with poorer outcome (8), especially in patients who developed LM. Breast cancer metastasis to the brain in TNBC is extremely faster compared to other subtypes, and clinicians should focus on the progression of symptoms. As CT and MRI results are usually negative in the early stage of LM, abnormal nervous system manifestations are sometimes more suggestive than imaging findings. Cranial nerve damage is a symptom highly suggestive of meningeal carcinomatosis, which is unlikely to occur due to intraparenchymal metastasis. The interactions between metastatic cancer cells and their microenvironment activate some signaling pathways such as PI3K-Akt, STAT3 and HER2-HER3 (12). Genetic test of the patient showed that the TP53 gene had mutations, which lead to the inactivation of tumor suppressor TP53 gene. She also had mutations in the JAK3 gene, which might contribute to the activation of the JAK-STAT pathway. Although there is still a lack of a reliable prediction model that can accurately screen the high-risk patients who may develop LM, prevention of LM from the primary tumors is a trend in the future.
Conclusions
In brief, this case report shows that: (I) breast cancer metastasis to the brain, especially LM, should be given sufficient vigilance and attention at the beginning of the diagnosis and treatment, particularly in TNBC patients who are at high risk. (II) Symptoms of LM may be masked by the chemotherapy adverse effects that include headache, dizziness, nausea and vomiting. (III) The results of MRI and CT may show negative results, and lumbar puncture with CSF should be done promptly if LM is highly suspected in clinical practice. (IV) The prognosis for TNBC patients who develop LM is poor, so early prevention, early detection and timely treatment are crucial.
Acknowledgments
We gratefully thank Dr. Fei Dong and his clinical team from Department of Radiology, the Second Affiliated Hospital, Zhejiang University School of Medicine, for their valuable advice in brain MRI analysis.
Funding: This work was supported by grants from
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-23-116/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-23-116/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-23-116/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Publication of this case report and accompanying images was waived from patient consent according to the ethics committee of Second Affiliated Hospital, Zhejiang University School of Medicine (Approval No. 2023LSYD0864).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gould J. Breaking down the epidemiology of brain cancer. Nature 2018;561:S40-1. [Crossref] [PubMed]
- Darlix A, Louvel G, Fraisse J, et al. Impact of breast cancer molecular subtypes on the incidence, kinetics and prognosis of central nervous system metastases in a large multicentre real-life cohort. Br J Cancer 2019;121:991-1000. [Crossref] [PubMed]
- Abraham AA. Clinical Outcome of Neoplastic Meningitis Associated with Breast Cancer. J Neurosci Rural Pract 2022;13:108-13. [Crossref] [PubMed]
- Le Rhun E, Preusser M, van den Bent M, et al. How we treat patients with leptomeningeal metastases. ESMO Open 2019;4:e000507. [Crossref] [PubMed]
- Chamberlain MC. Neoplastic meningitis. Oncologist 2008;13:967-77. [Crossref] [PubMed]
- Rossi G, Mu Z, Rademaker AW, et al. Cell-Free DNA and Circulating Tumor Cells: Comprehensive Liquid Biopsy Analysis in Advanced Breast Cancer. Clin Cancer Res 2018;24:560-8. [Crossref] [PubMed]
- Le Rhun E, Guckenberger M, Smits M, et al. EANO-ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up of patients with brain metastasis from solid tumours. Ann Oncol 2021;32:1332-47. [Crossref] [PubMed]
- Carausu M, Carton M, Darlix A, et al. Breast cancer patients treated with intrathecal therapy for leptomeningeal metastases in a large real-life database. ESMO Open 2021;6:100150. [Crossref] [PubMed]
- Melisko ME, Assefa M, Hwang J, et al. Phase II study of irinotecan and temozolomide in breast cancer patients with progressing central nervous system disease. Breast Cancer Res Treat 2019;177:401-8. [Crossref] [PubMed]
- Jenkins S, Zhang W, Steinberg SM, et al. Phase I Study and Cell-Free DNA Analysis of T-DM1 and Metronomic Temozolomide for Secondary Prevention of HER2-Positive Breast Cancer Brain Metastases. Clin Cancer Res 2023;29:1450-9. [Crossref] [PubMed]
- Klaas E, Sung E, Azizi E, et al. Advanced breast cancer metastasized in the brain: treatment standards and innovations. J Cancer Metastasis Treat 2023;9:23. [Crossref]
- Hosonaga M, Saya H, Arima Y. Molecular and cellular mechanisms underlying brain metastasis of breast cancer. Cancer Metastasis Rev 2020;39:711-20. [Crossref] [PubMed]
- Kuksis M, Gao Y, Tran W, et al. The incidence of brain metastases among patients with metastatic breast cancer: a systematic review and meta-analysis. Neuro Oncol 2021;23:894-904. [Crossref] [PubMed]
- Watanabe J, Mitsuya K, Nakamoto S, et al. Leptomeningeal Metastasis in ER + HER2- Advanced Breast Cancer Patients: A Review of the Cases in a Single Institute Over a 15-year Period. Breast Cancer Res Treat 2021;189:225-36. [Crossref] [PubMed]
Cite this article as: Jin Y, Lu J, Zhang T, Yan S, Chen H, Zhang K, Chen Y, Zhou J. Leptomeningeal metastasis of breast cancer during neo-adjuvant chemotherapy in a 38-year-old woman: a case report. AME Case Rep 2024;8:37.


