
Improved postural control in a patient having adult spinal deformity and previous thoraco-lumbar scoliosis surgery: a Chiropractic Biophysics® case report
Highlight box
Key findings
• Dynamic postural control and static posture correction is possible in patients with previous spinal surgery.
What is known and what is new?
• Patients with previous spinal fusion and deformity often have postural control impairment.
• This case demonstrates the improvement in postural control in an older patient who is contra-indicated for further spinal surgery.
What is the implication, and what should change now?
• Future research is needed to explore non-surgical approaches to improving balance control in older persons with spinal deformity as falling is a great risk for this population.
Introduction
Adult spinal deformity (ASD), technically defined as having scoliosis >20°, sagittal vertical axis (SVA) >5 cm, pelvic tilt >25°, and/or thoracic kyphosis >60°, is a significant source of the Global Burden of Disease (1). The complex condition involves progressive deformity and deterioration of the spine due to excessive and abnormal loads in the sagittal and/or coronal plane (2). ASD is a major factor in disability and pain and thus surgical intervention is frequently a treatment choice. Surgical complexity, however, becomes much greater when there are multiple spine deformities (3), and this complexity can lead to ineffective surgical intervention; that is, the spine surgery does not improve the spinal deformity. Thus, therapeutic spine rehabilitation is often necessary after surgical intervention, particularly if post-surgical symptoms and disability persist.
Patients with ASD show impairment in postural control; the maintenance of standing balance. Increased center of pressure (COP) amplitudes are indicative of unsteadiness (4-6). Ito et al., for example, found patients having a SVA >40 mm showed greater root mean square (RMS) displacement in the eyes closed (EC) condition vs. a young and healthy control group (4). Godzik et al. found that thoracic hyperkyphosis positively correlated with medial-lateral (ML) sway displacement in eyes open (EO) and EC conditions as well as total sway area in the EC condition vs. age-matched controls (5). Yagi et al. found those with SVA >50 mm and/or scoliosis >20° displayed greater sway area and left-to-right differences in ground reaction forces (6). There is a dearth of clinical evidence on the improvement in postural control for patients with ASD and previous surgical intervention.
Herein we present a case of a clinically significant improvement in postural control as measured by force plate after a multimodal treatment program of CBP posture rehabilitation as well as postural control rehabilitation in an elderly female with long-standing ASD including thoracic hyper-kyphosis and previous surgical intervention for thoracolumbar scoliosis. We present this article in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-23-183/rc).
Case presentation
In June, 2022, a 69-year-old female presented with gait and balance issues as well as back pains and headaches (2×/month). The patient underwent surgical stabilization for scoliosis at age 16 involving a single Harrington rod placed from T10 to L4. The pains were described to be in the mid and lower back, aggravated by walking and standing for too long and relieved by sitting or standing with her arms positioned behind her back. The pain started insidiously, approximately 3 years previous and were reported to range from 0 to 8/10 (0= no pain; 10= disabling pain) dependent on body position. She also reported having chronic digestive issues and headaches since age 4 years. Regarding her mobility, she reported feeling unsteady and lacked confidence to walk for extended periods due to balance issues which had been developing over the last 5 years. The patient did not report any previous falls and did not use a walking aid. The patient also reported having long standing stooped posture as well as diagnosed osteopenia. There was no familial scoliosis. The patient reported past physiotherapy that was directed at a previous hip flexor issue that only provided short-term relief.
Physical assessment showed significant rigidity throughout the thoracolumbar spine. Range of motion was limited for all lumbar spine movements. Palpation revealed tight and tender paraspinal muscle fibers throughout the middle and upper thoracic spine. The uppermost end of the Harrington rod could be palpated through the skin. Visual posture assessment identified a forward stooped posture with anterior head translation (AHT). Many orthopedic tests could not be performed due to the inability to move the spine and limbs due to inflexibility, and the straight leg raiser was limited bilaterally to 45° due to low back pain and hamstring tightness. Muscle strength testing revealed lower limb weakness (4/5) on all lower limb muscle tests. Reflexes were normal.
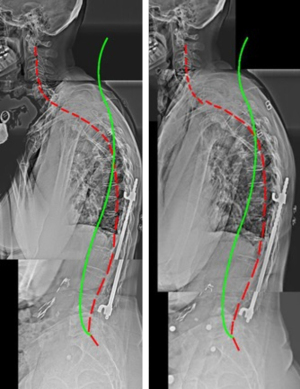
Sectional standing radiography images of the spine were taken and digitized using an advanced spine digitizing program (PostureCo Inc., Trinity, FL, USA) and stitched to create a full-spine profile. Alignment analysis was performed by the posterior tangent method which has excellent accuracy and reliability (7,8). The sagittal profile spinal alignment (Figure 1) shows a forward SVA from C2 to S1 (SVA: 118.4 mm), AHT (26.4 mm), and thoracic hyperkyphosis (64.7°). Also seen is the Harrington rod located between T10 and L4.
Standing balance testing was performed using the BTrackS balance plate (Balance Tracking Systems, San Diego, CA, USA) (9). This plate has established validity (10-12) and test re-test reliability (13). The modified clinical test of sensory integration and balance (mCTSIB) was performed to assess the different bodily systems that contribute to postural control (13). Figure 2 and Table 1 show the results of the testing. The patient demonstrated postural control impairment as the COP derived parameters for the ‘vestibular’ condition (EC; standing on foam) were high (14,15). Importantly, the patient scored a 165 cm COP total path length which placed her below the 10% percentile according to the normative data for females aged 60 years plus integrated into the proprietary BTrackS software (16).
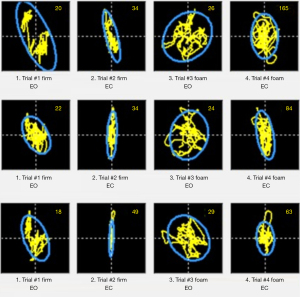
Table 1
| mCTSIB trial conditions | COP path length (cm) | 95% area (cm2) | Range ML (cm) |
Range AP (cm) |
Avg. velocity (cm/s) | RMS ML (cm) | RMS AP (cm) |
|---|---|---|---|---|---|---|---|
| (I) Standard (firm-EO) | |||||||
| Pre | 20.0 | 3.3 | 1.3 | 2.3 | 1.0 | 0.4 | 0.6 |
| Post1 | 22.0 | 1.0 | 0.9 | 1.5 | 1.1 | 0.2 | 0.3 |
| Post2 | 18.0 | 1.2 | 0.9 | 1.8 | 0.9 | 0.2 | 0.3 |
| (II) Proprioception (firm-EC) | |||||||
| Pre | 34.0 | 4.4 | 1.4 | 4.1 | 1.7 | 0.3 | 1.0 |
| Post1 | 34.0 | 2.9 | 0.9 | 4.6 | 1.7 | 0.2 | 0.9 |
| Post2 | 49.0 | 3.4 | 0.9 | 6.5 | 2.4 | 0.1 | 1.3 |
| (III) Visual (foam-EO) | |||||||
| Pre | 26.0 | 3.8 | 2.0 | 2.3 | 1.3 | 0.5 | 0.4 |
| Post1 | 24.0 | 2.8 | 1.8 | 2.1 | 1.2 | 0.3 | 0.4 |
| Post2 | 29.0 | 4.0 | 2.4 | 2.1 | 1.4 | 0.5 | 0.5 |
| (IV) Vestibular (foam-EC) | |||||||
| Pre | 165.0 | 53.3 | 6.6 | 12.1 | 8.2 | 1.3 | 2.1 |
| Post1 | 84.0 | 14.4 | 3.1 | 7.0 | 4.2 | 0.6 | 1.5 |
| Post2 | 63.0 | 14.0 | 3.0 | 7.5 | 3.1 | 0.6 | 1.2 |
mCTSIB, modified clinical test of sensory integration and balance; COP, center of pressure; ML, medial-lateral; AP, anterior-posterior; Avg., average; RMS, root mean square; EC, eyes closed; EO, eyes open.
Treatment was prescribed for posture correction using CBP technique methods (17,18). Based on the measured abnormalities on the radiographs, a program was prescribed to extend the spine above the top of the Harrington rod using spine extension mirror image® traction (Figure 3). Due to her age, osteopenia, and her exaggerated hunched posture, progressing with the amount of weight added to the head with a head/forehead strap was slow but progressive to lessen any risk of exacerbation. The patient began traction with no weight and progressed to 12 pounds.

The patient also performed a series of five mirror image exercises. The first involved standing against a block placed at the mid thoracic spine at the location of the peak of the mid back curve abnormality. Standing with the back to the wall, the head and pelvis were retracted backwards towards the wall. This position was held for 5 seconds and repeated for 50 repetitions. The rest of the exercises were done on the PowerPlate® (Northbrook, IL, USA) whole-body vibration platform to increase their intensity (19). The second exercise was the “birddog”. On all fours, the opposite arm and leg were extended, held, and switched to the opposite side. The third exercise was the superman, laying on the stomach the legs and arms were raised and held. The fourth exercise were ‘W’s’, where the patient stood with the arms in the anatomical position, then bent the elbows to form a ‘W’, then straightened the arms overhead and repeated in the opposite sequence. The fifth exercise was horizontal arm extensions with resistance. These exercises were encouraged to do daily as well as in-office.
Two more exercises were performed for balance. Walking in place and standing squats were performed on the PowerPlate. All platform exercises were performed for 60 seconds. Initially, only one cycle of each exercise was performed, as treatment progressed, two cycles were performed. Later three cycles were performed for the balance training exercises. The patient also received paraspinal stimulation using a hand-held percussion device (Impac Inc., Salem, OR, USA) while in a seated position. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal. The patient tolerated the treatment well and there were no adverse events with treatment.
After 36 treatments (30 minutes/session) over the first 3 months (i.e., 3×/week), the patient reported improved balance and gait and stated she felt ‘better posture’. The back pain was reported to be largely relieved (ranging from 0 to 5/10 with long durations of standing) and the headaches were reported to be rare. Radiography showed improvement in the C1–S1 SVA (98.8 vs. 118.4 mm) (not shown). At this time, the patient continued on a three times per week schedule and started to add weight off the head to intensify the spine traction (Figure 3).
After 7 months (72 treatments) the patient reported to be doing well with her balance and gait, however, reported she still felt ‘compressed’ within the mid-torso area. A posturography exam on the force plate demonstrated improvements in COP parameters for the vestibular condition (EC; standing on foam). The COP total path length decreased by 81 cm (84 vs. 165 cm), the 95% ellipse area decreased by 38.9 cm2 (14.4 vs. 53.3 cm2), and the other parameters decreased by approximately half (Table 1). The patient’s percentile score for the vestibular condition changed from the 10th percentile to better than the 70th percentile. His time the patient had worked up to the traction weight of 7 pounds (Figure 3).
After 10 months (108 treatments) the patient reported to be doing well with balance and gait performance and felt stronger due to the exercise program. She reported that the compressed feeling in the mid torso area was still present but felt it was changing (i.e., improving). Radiography showed her posture was slightly improved in both reduced AHT (19.7 vs. 26.4 mm) and overall C1–S1 sagittal balance (92.3 vs. 118.4 mm). Posturography testing showed a further decrease in COP total path length (63 vs. 165 cm), the average velocity also decreased to 3.1 cm/s (vs. 8.2 cm/s). The patient had worked up to a traction weight of 12 pounds (Figure 3). The patient reported she ‘felt good’ in traction as it was pulling in the right areas.
Discussion
Key findings
This case illustrates a clinically significant improvement in standing balance following treatment consisting of CBP spinal rehabilitation as well as balance rehabilitation using whole-body vibration. All COP parameters measured had a significant decrease for the vestibular condition; the fourth trial of mCTSIB which demonstrates important measures of improved performance (14-16). Importantly, there was a 102 cm reduction in COP total path length, which is well beyond the minimal detectable change of 10.5 cm (20) and 19.4 cm (21) for young and older adults in the EC condition, respectively. As a result, the patient’s scores on the vestibular condition showed a change from scoring below the 10th percentile to scoring above the 90th percentile for a female older than 60 years (16).
Strengths and limitations
There are limitations to this case. First, this is a single case and despite the improvement in postural control (balance), no causal inference can be made. Second, there is no long-term follow-up after the cessation of treatment to assess the stability of improved postural control. The last limitation is the use of multiple treatment modalities; namely, PowerPlate exercises, CBP spinal extension traction, paraspinal stimulation via mechanical instrument, and mirror image exercises. The specific modality leading to postural control improvement cannot be known conclusively. Larger, clinical trials are necessary to determine firm conclusions. It is speculated that both non-surgical posture improvement as well as whole-body vibration exposures have the potential to contribute to improved postural control and balance performance.
Comparison with similar research
It is known that patients with ASD have impaired postural control (4-6). Although some pre- and post-surgery trials have determined differences in some measures of postural control after spinal surgery for ASD (22), most studies fail to show significant differences following surgical re-alignment (23). Sakaguchi et al. (23) discovered that the order of recovery following spinal surgery for ASD was first in dynamic balance, second in gait, and finally, and lagging behind was static standing balance. In fact, in their study, static balance remained unchanged at the 12-month post-operative assessment. They suggested that poor adaptation to a new spine alignment may explain the lack of balance performance improvement at the 1-year post-surgical assessment (23). Thus, the current case demonstrating improved postural control after 10 months of rehabilitation warrants further research.
Explanation of findings
The mCTSIB is a unique balance test that systematically assesses the different sensory systems involved with achieving postural stability. Importantly, our measures found significant deficiency in the fourth trial condition; that is, the vestibular condition. Piątek-Krzywicka et al. determined that performing this test on adolescent idiopathic scoliosis (AIS) patients demonstrated that it was only on the vestibular trial that a significant difference showing impairment was observed as compared to age-matched controls (24). Further, Sim et al. determined that larger spinal deformity magnitudes demonstrated larger postural impairment, and increased energy rates (as determined by discrete wavelet transformation) were observed for vestibular input over both visual and somatosensory inputs (25). Others have also demonstrated deficiencies in postural control in the condition that isolates the vestibular system (26,27) demonstrating that vestibular impairment is a phenomenon occurring in patients with ASD. It seems ASD patients may maximally exert their compensatory muscles, so-called ‘postural reserves’ in the attempt to maintain their postural steadiness (5). This is seen, for example, in those with thoracic hyperkyphosis who have severe fatigue in the paravertebral spinal muscles (28).
Although clinically significant postural control improvements occurred in this patient, as all COP parameters decreased in the performance of the vestibular trial after 10-month of treatment, we cannot confirm why these changes occurred. Attributing this to the improved postural alignment is questionable as there was only a small improvement in the C1–S1 SVA. It should be noted however, unlike spinal surgery which forces a re-positioning of the spine by surgical hardware, postural improvements by non-invasive methods occur over a longer time frame and involve exercising the muscles that support and move the spine as part of the treatment and may show promise in improving balance control. Alternatively, whole-body vibration has been shown to contribute to a triggering towards recalibration of the sensorimotor systems. Rigoni et al. found that when exposed to whole-body vibration, although the challenge destabilizes balance initially, the stimulation increases the recruitment of more muscular effort (29). It is postulated that this process shifts the muscle modulation towards a supraspinal control and recalibration of muscle recruitment (29).
Implications and actions needed
Improved balance has been associated with reduced fall risk (30,31). Fall reduction in elderly patients may be preventive for many untoward consequences; note that the patient of this report also had a comorbidity of osteopenia. Further research is needed to elucidate which treatment approaches are efficacious at improving postural balance control in those with spinal deformity.
Conclusions
A non-surgical rehabilitation program demonstrated dramatically improved balance performance in an elderly female diagnosed with osteopenia, ASD, and previous spine deformity surgery. This approach to improving postural stability is important and further investigations should be undertaken.
Acknowledgments
Funding: This work was funded by
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-23-183/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-23-183/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-23-183/coif). All authors report that this study has received funding support from CBP NonProfit Inc. P.A.O. is a compensated consultant for CBP NonProfit, Inc. J.W.H. is compensated researcher for CBP NonProfit Inc. D.E.H. is the CEO of Chiropractic Biophysics (CBP) and provides post-graduate education to health care providers/physicians. Spine rehabilitation devices are distributed through his company. D.E.H. is the president of CBP NonProfit, Inc.—a not-for-profit spine research foundation. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Diebo BG, Shah NV, Boachie-Adjei O, et al. Adult spinal deformity. Lancet 2019;394:160-72. [Crossref] [PubMed]
- Iyer S, Sheha E, Fu MC, et al. Sagittal Spinal Alignment in Adult Spinal Deformity: An Overview of Current Concepts and a Critical Analysis Review. JBJS Rev 2018;6:e2. [Crossref] [PubMed]
- Laverdière C, Georgiopoulos M, Ames CP, et al. Adult Spinal Deformity Surgery and Frailty: A Systematic Review. Global Spine J 2022;12:689-99. [Crossref] [PubMed]
- Ito T, Sakai Y, Yamazaki K, et al. Postural Sway in Older Patients with Sagittal Imbalance and Young Adults during Local Vibratory Proprioceptive Stimulation. Healthcare (Basel) 2021;9:210. [Crossref] [PubMed]
- Godzik J, Frames CW, Smith Hussain V, et al. Postural Stability and Dynamic Balance in Adult Spinal Deformity: Prospective Pilot Study. World Neurosurg 2020;141:e783-91. [Crossref] [PubMed]
- Yagi M, Kaneko S, Yato Y, et al. Standing Balance and Compensatory Mechanisms in Patients With Adult Spinal Deformity. Spine (Phila Pa 1976) 2017;42:E584-91. [Crossref] [PubMed]
- Fedorchuk C, Comer RD, McRae C, et al. Validity of Radiographic Analyses Between Hand-Drawn and Computer- Aided Measurements: A Double-Blinded Test-Retest Trial. Curr Med Imaging 2023;19:1071-8. [Crossref] [PubMed]
- Harrison DE, Holland B, Harrison DD, et al. Further reliability analysis of the Harrison radiographic line-drawing methods: crossed ICCs for lateral posterior tangents and modified Risser-Ferguson method on AP views. J Manipulative Physiol Ther 2002;25:93-8. [Crossref] [PubMed]
- Goble DJ, Baweja N, Baweja HS. BTrackS: A Low-Cost, Portable Force Plate for Objectively Measuring Balance Deficits and Fall Risk. Home Healthc Now 2019;37:355-6. [Crossref] [PubMed]
- Richmond SB, Dames KD, Goble DJ, et al. Leveling the playing field: Evaluation of a portable instrument for quantifying balance performance. J Biomech 2018;75:102-7. [Crossref] [PubMed]
- Goble DJ, Khan E, Baweja HS, et al. A point of application study to determine the accuracy, precision and reliability of a low-cost balance plate for center of pressure measurement. J Biomech 2018;71:277-80. [Crossref] [PubMed]
- O'Connor SM, Baweja HS, Goble DJ. Validating the BTrackS Balance Plate as a low cost alternative for the measurement of sway-induced center of pressure. J Biomech 2016;49:4142-5. [Crossref] [PubMed]
- Goble DJ, Conner NO, Nolff MR, et al. Test-Retest Reliability of the Balance Tracking System Modified Clinical Test of Sensory Integration and Balance Protocol Across Multiple Time Durations. Med Devices (Auckl) 2021;14:355-61. [Crossref] [PubMed]
- Prieto TE, Myklebust JB, Hoffmann RG, et al. Measures of postural steadiness: differences between healthy young and elderly adults. IEEE Trans Biomed Eng 1996;43:956-66. [Crossref] [PubMed]
- Quijoux F, Nicolaï A, Chairi I, et al. A review of center of pressure (COP) variables to quantify standing balance in elderly people: Algorithms and open-access code. Physiol Rep 2021;9:e15067. [Crossref] [PubMed]
- BTrackS™. mCTSIB Normative Data. Accessed August 29, 2023. Available online: https://balancetrackingsystems.com/wp-content/uploads/2020/06/BTS-Normative-CTSIB-Data-2020.pdf
- Harrison DD, Janik TJ, Harrison GR, et al. Chiropractic biophysics technique: a linear algebra approach to posture in chiropractic. J Manipulative Physiol Ther 1996;19:525-35. [PubMed]
- Harrison DE, Oakley PA. An introduction to Chiropractic BioPhysics®(CBP®) technique: A full spine rehabilitation approach to reducing spine deformities. In: Bernardo-Filho M, Taiar R, de Sá-Caputo DC, et al. editors. Complementary Therapies. London: IntechOpen Publishers; 2022.
- Lee DY. Analysis of muscle activation in each body segment in response to the stimulation intensity of whole-body vibration. J Phys Ther Sci 2017;29:270-3. [Crossref] [PubMed]
- Morrison R, Petit KM, Kuenze C, et al. Preseason to Postseason Changes on the BTrackS Force Plate in a Sample of College Athletes. J Sport Rehabil 2020;29:134-6. [Crossref] [PubMed]
- Levy SS, Thralls KJ, Kviatkovsky SA. Validity and Reliability of a Portable Balance Tracking System, BTrackS, in Older Adults. J Geriatr Phys Ther 2018;41:102-7. [Crossref] [PubMed]
- Yagi M, Ohne H, Kaneko S, et al. Does corrective spine surgery improve the standing balance in patients with adult spinal deformity? Spine J 2018;18:36-43. [Crossref] [PubMed]
- Sakaguchi T, Tanaka M, Suthar H, et al. Chronological evaluation of gait ability and posture balance after adult spinal deformity surgery. Appl Sci 2022;12:4285. [Crossref]
- Piątek-Krzywicka E, Borzucka D, Kuczyński M. Postural control through force plate measurements in female AIS patients compared to their able-bodied peers. Sci Rep 2022;12:13170. [Crossref] [PubMed]
- Sim T, Yoo H, Lee D, et al. Analysis of sensory system aspects of postural stability during quiet standing in adolescent idiopathic scoliosis patients. J Neuroeng Rehabil 2018;15:54. [Crossref] [PubMed]
- Sinaki M, Brey RH, Hughes CA, et al. Balance disorder and increased risk of falls in osteoporosis and kyphosis: significance of kyphotic posture and muscle strength. Osteoporos Int 2005;16:1004-10. [Crossref] [PubMed]
- Lynn SG, Sinaki M, Westerlind KC. Balance characteristics of persons with osteoporosis. Arch Phys Med Rehabil 1997;78:273-7. [Crossref] [PubMed]
- Ghamkhar L, Kahlaee AH. The effect of trunk muscle fatigue on postural control of upright stance: A systematic review. Gait Posture 2019;72:167-74. [Crossref] [PubMed]
- Rigoni I, Degano G, Hassan M, et al. Sensorimotor recalibration of postural control strategies occurs after whole body vibration. Sci Rep 2023;13:522. [Crossref] [PubMed]
- El-Khoury F, Cassou B, Charles MA, et al. The effect of fall prevention exercise programmes on fall induced injuries in community dwelling older adults: systematic review and meta-analysis of randomised controlled trials. BMJ 2013;347:f6234. [PubMed]
- Sherrington C, Michaleff ZA, Fairhall N, et al. Exercise to prevent falls in older adults: an updated systematic review and meta-analysis. Br J Sports Med 2017;51:1750-8. [Crossref] [PubMed]
Cite this article as: Oakley PA, Haas JW, Harrison DE. Improved postural control in a patient having adult spinal deformity and previous thoraco-lumbar scoliosis surgery: a Chiropractic Biophysics® case report. AME Case Rep 2024;8:58.


