
Two cases of sigmoid colon cancer with intussusception prolapsing through the anus in adults: consideration of preoperative reduction and surgical approaches: case reports
Highlight box
Key findings
• Gently reducing intussusception under general anesthesia rather than forcibly attempting reduction is crucial. Laparoscopic surgery is useful for treating sigmoid colon cancer with intussusception prolapsing through the anus.
What is known and what is new?
• Adult intussusception is a rare condition that is often associated with a high incidence of malignancy.
• The optimal management strategy remains controversial. Herein, we highlight the different surgical options available.
What is the implication, and what should change now?
• Accumulating knowledge about adult intussusception could contribute to standardizing the approach to managing this rare condition.
Introduction
Intussusception is relatively rare in adults and is associated with a high incidence of malignancy. Surgical resection is recommended, and less invasive management may be indicated. There are different opinions on whether bowel reduction should be performed before bowel resection because forcible bowel reduction may lead to the seeding of cancer cells or hematogenous metastasis, damage the intestinal tract, and increase the risk of suture failure (1,2). Herein, we report two cases of sigmoid colon cancer with intussusception that prolapsed through the anus. We present this article in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-24-1/rc).
Case presentation
Case 1
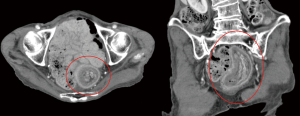
An 84-year-old woman was referred to our hospital for further management of a tumor prolapse through the anus. She was diagnosed with adenocarcinoma based on a biopsy of the tumor performed at a previous hospital. The patient experienced tenderness and poor defecation. In serum biochemistry tests, carcinoembryonic antigen (CEA) and carbohydrate antigen 19-9 (CA19-9) were within the normal range. Endoscopic reduction attempts were unsuccessful, and contrast enema did not visualize the oral intestinal tract. Abdominal contrast-enhanced computed tomography (CT) revealed ‘a target sign’ appearance confirming the diagnosis of intussusception due to proximal sigmoid colon cancer (Figure 1). There was no evidence of locally advanced or metastatic disease. The patient underwent urgent surgery due to a concern of ischemia resulting from the incarcerated prolapse. Under general anesthesia, the patient was placed in the modified lithotomy position. A midline incision was made from the umbilicus to the pubis. The peritoneum was opened; intussusception of the sigmoid colon was observed; and no serosal infiltration or adjacent organ invasion was noted (Figure 2). Attempts at manual reduction of the incarcerated bowel were unsuccessful. Furthermore, the assistant pushed the incarcerated bowel up from the anus. The intussusception was successfully released using the Hutchinson technique (Figure 3). The inferior mesenteric artery and veins were identified and ligated. The colon part proximal to the tumor was thick and edematous, making primary anastomosis difficult. The decision was made to resect the tumor with a temporary colostomy. The distal colon was resected at the level of the healthy colon on glass examination, which was located 15 cm above the peritoneal reflection. Histopathological examination led to a diagnosis of a mucinous adenocarcinoma in adenoma in the sigmoid colon sized 4.0 cm × 5.5 cm, which invaded the subserosa (pT3). The resection margins were free from carcinoma; no metastasis was noted in the 12 regional lymph nodes (pN0). Four days after surgery, movement of the intestine of the patient was recovered, and diet was initiated. There were no complications, but the patient lacked motivation and had difficulty getting out of bed and eating. She was discharged on postoperative day 24. The patient was doing well during the outpatient follow-up at 6 months, without recurrence.
Case 2
A 76-year-old woman was admitted to our hospital with a 2-day history of lower abdominal pain and blood-streaked stools. The mucosa of the prolapsed intestine showed tumor-like villous adenoma (Figure 4). Reduction of the prolapsed intestine through manual intervention was performed. However, prolapse of the intestine easily recurred. Abdominal CT scan showed intussusception and significant proximal fecal retention. There was no evidence of locally advanced or metastatic disease. Endoscopic reduction was unsuccessful. A biopsy revealed tubular adenocarcinoma in tubulovillous adenoma. In serum biochemistry tests, CEA and CA19-9 were within the normal range. Although the intestine showed no ischemia, emergency surgery was performed because of intussusception and persistent abdominal pain. Under general anesthesia, a midline incision was made from the umbilicus to the pubis. Intraoperatively, a sigmoid colon intussusception was observed. Attempts using the Hutchinson technique were unsuccessful. However, the intussusception was relieved by the transanal insertion of a circular sizer (Figure 5). The inferior mesenteric artery and vein were identified and ligated and oncological resection was performed. The distal colon was resected 15 cm above the peritoneal reflection. Due to the significantly edematous intestine, intestinal anastomosis was not performed, and a temporary colostomy was created. Histopathological examination revealed well differentiated tubular adenocarcinoma and tubule-villous adenoma in the sigmoid colon sized 5.3 cm × 3.0 cm which invaded the submucosa (pT1) and no metastasis in 12 regional lymph nodes was noted (pN0). Five days after surgery, movement of the intestine of the patient was recovered, and diet was initiated. The patient had diarrhea symptoms but recovered without other complications, and the patient was discharged on postoperative day 37. At present, 3 years after surgery, the patient is free of symptoms without recurrence.
Ethical consideration
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committees and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patients for publication of this case report and accompanying image. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Intussusception is a rare condition in adults, accounting for 5% of all cases (3,4). Adult intussusception is caused by an underlying disease, with benign tumors in the small intestine and malignant tumors in the colon (5). Various surgical options are available for managing rectal prolapse. Whether reduction of intussusception should be performed prior to colectomy remains controversial. Forcible bowel reduction may lead to seeding of cancer cells or hematogenous metastasis and damage the intestinal tract and increase the risk of suture failure (4,6-8), whereas resection should be performed after reduction of intussusception to evaluate the location and depth of tumor involvement (9).
In our country, there are numerous case reports. However, reports in English are rare. We searched for previous reports on sigmoid colon cancer with intussusception prolapsing through the anus in ICHUSHI using the keywords “sigmoid colon cancer”, “prolapsing through the anus” and reviewed 59 cases (10-16) (Table 1). The mean patient age was 77.1 years and percentage of female patients was 78%. Due to the high proportion of elderly patients, postoperative recovery was delayed, resulting in an average postoperative hospital stay of 25 days. Complications such as pneumonia, cystitis, and paralytic ileus were observed, but there were no complications specific to the present condition. Older women exhibited a tendency to be more susceptible to sigmoid colon cancer with intussusception prolapsing through the anus. The causes are thought to involve aging, relaxation of the pelvic floor muscles associated with childbirth, and weakening of the supporting tissues around the anal sphincter and surrounding area of the rectum. In 76% (45/59) of cases where preoperative reduction was attempted, reduction was unsuccessful in 69% (31/45). Most patients underwent open abdominal surgery. Tumor depth varied in different cases. These cases are considered typical examples.
Table 1
| Variables | Character/pathology/outcome | Cases (n=59) |
|---|---|---|
| Age, years | Mean: 77.1 (range, 33 to 95) | |
| Sex | Male | 13 |
| Female | 46 | |
| Tumor type | Type 0 | 11 |
| Type 1 | 14 | |
| Type 2 | 19 | |
| Type 3 | 2 | |
| Type 4 | 0 | |
| Type 5 | 1 | |
| Unknown | 12 | |
| Pathological diagnosis | Well differentiated adenocarcinoma | 29 |
| Moderately differentiated adenocarcinoma | 20 | |
| Mucinous adenocarcinoma | 3 | |
| Papillary carcinoma | 1 | |
| Unknown | 6 | |
| Tumor depth | Mucosa | 9 |
| Submucosa | 6 | |
| Tunica muscularis propria | 13 | |
| Subserosa | 19 | |
| Serosa | 3 | |
| Unknown | 9 | |
| Surgical treatment | Sigmoidectomy | 25 |
| Low anterior resection | 1 | |
| High anterior resection | 4 | |
| Transanal tumorectomy | 7 | |
| Hartmann’s operation | 14 | |
| Abdominoperineal resection | 1 | |
| Laparoscopic sigmoidectomy | 2 | |
| Laparoscopic Hartmann’s operation | 1 | |
| Open abdominal tumorectomy | 1 | |
| Unknown | 3 | |
| Reduction | Preoperative reduction | 14 |
| Postoperative reduction | 22 | |
| Impossible | 9 | |
| Undone | 6 | |
| Unknown | 8 |
In cases of intussusception associated with colorectal cancer, preoperative reduction should not be performed, as it may exacerbate perforation and disseminate tumor cells into the abdominal cavity, leading to potential seeding (4,6-8). However, in most cases, preoperative reduction has been attempted. Some researchers have reported that preoperative reduction was important to determine the appropriate extent of bowel resection and lymph node dissection before performing oncological resection. In addition, it could improve intestinal edema and increase the possibility of avoiding a colostomy (15). In our both cases, preoperative reduction was attempted but failed. Moreover, significant proximal fecal retention was observed, increasing the risk of intestinal ischemia or perforation. Consequently, emergency open abdominal surgery was performed. As a result, intraoperative reduction was successful followed by oncological resection, without observing any recurrence. Sufficient muscle relaxation was maintained under general anesthesia, and gentle reduction from both sides of the anal and abdominal approaches was important. Therefore, avoiding forcible reduction is crucial.
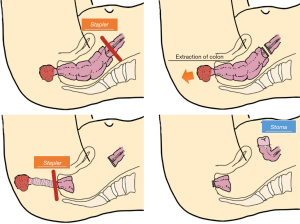
Laparoscopic surgery is widely used for the resection of benign and malignant gastrointestinal tumors. Laparoscopic procedures have also been reported for cases of intussusception associated with colorectal cancer. Considering that older women tended to have intussusception of colorectal cancer, laparoscopic surgery could be a suitable and advantageous option in terms of minimal invasiveness. However, in cases of intussusception, the laparoscopic approach presents challenges due to the limited working space. Kato et al. reported a combination of laparoscopic lymph node dissection, proximal bowel resection, and intestinal anastomosis, followed by transanal rectal-side bowel resection (14). In this case, the oral side of the sigmoid colon was resected, and the retrorectal space was mobilized to the levator muscle level. The intestine was subsequently pulled towards the anal side using a perineal approach. Furthermore, the distal rectum was transected using an automatic suture device outside the anus. The resected specimens were extracted (Figure 6). This is a good example of successful laparoscopic oncological resection without the need for reduction.
Conclusions
Regarding the choice of surgical approach, in cases in which reduction can be easily achieved, routine preoperative examinations should be performed after reduction and proceed with elective surgery. In such cases, intestinal injury, cancer cell seeding, or hematogenous metastasis would unlikely occur. On the other hand, in cases such as ours, gently reducing intussusception under general anesthesia, rather than forcibly attempting reduction is crucial. Additionally, laparoscopic surgery could be useful for treating sigmoid colon cancer with intussusception prolapsing through the anus. The choice of the surgical approach and preoperative reduction depends on patient’s clinical condition. Further studies could contribute to standardizing the approach to managing this rare condition.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-24-1/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-24-1/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-24-1/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patients for publication of this case report and accompanying image. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Toshio S, Tetsuro T, Takashi N, et al. A case of adult rectal intussusception caused by sigmoid colon cancer resected after reduction by combined transanal and laparoscopic approach. Nihon Naishikyo Geka Gakkai Zasshi 2018;23:379-84.
- Takeshi S, Mizuyuki K, Masaichi O, et al. A case of intussusception caused by rectal cancer in an adult. Nihon Rinsho Geka Gakkai Zasshi 2004;65:459-63. [Crossref]
- Kimiyoshi Y, Masahiko O, Kiyohiko Y, et al. Clinicopathological study on classification of intussusception. Jap J Gastroenterological Surg 1994;27:1940-8. [Crossref]
- Azar T, Berger DL. Adult intussusception. Ann Surg 1997;226:134-8. [Crossref] [PubMed]
- Weilbaecher D, Bolin JA, Hearn D, et al. Intussusception in adults. Review of 160 cases. Am J Surg 1971;121:531-5. [Crossref] [PubMed]
- Finlayson E, Nelson H. Laparoscopic colectomy for cancer. Am J Clin Oncol 2005;28:521-5. [Crossref] [PubMed]
- Zerey M, Burns JM, Kercher KW, et al. Minimally invasive management of colon cancer. Surg Innov 2006;13:5-15. [Crossref] [PubMed]
- Nagorney DM, Sarr MG, McIlrath DC. Surgical management of intussusception in the adult. Ann Surg 1981;193:230-6. [Crossref] [PubMed]
- Kiyoshi I, Masaji Y, Hiroshi A, et al. Two cases of cancer of the sigmoid colon with intussusception prolapsing through the anus. Nihon Rinsho Geka Gakkai Zasshi 1998;59:753-8. [Crossref]
- Kazuyuki O, Akihito K, Kento K, et al. A Case of Sigmoid Colon Cancer with Intussusception Prolapsing through the Anus. Nihon Fukubukyukyu Igakkai Zasshi 2013;33:111-6.
- Toyoda S, Horii K, Okumura S, et al. Sigmoid colon cancer with intussusception prolapsing through the anus treated by elective laparoscopic radical surgery. Nihon Shokakibyo Gakkai Zasshi 2018;115:87-93. [PubMed]
- Akyuz M, Topal U, Gok M, et al. Sigmoid colon cancer presenting as complete prolapse. Ann Ital Chir 2019;8:345-8. [PubMed]
- Arimoto A, Sakamoto H, Asakura Y, et al. A Case of Sigmoid Colon Cancer with Intussusception Prolapsing through the Anus. Gan To Kagaku Ryoho 2022;49:1717-9. [PubMed]
- Kato Y, Yamamoto S, Yoshikawa Y, et al. A Case of Sigmoid Colon Cancer with Intussusception Treated by Laparoscopic Surgery and Removed Transanally. Nihon Shokaki Geka Gakkai Zasshi 2021;54:424-9. [Crossref]
- Kuniyasu M, Yoshida M, Mizumoto T, et al. A case of intussusception prolapsing through the anus caused by sigmoid colon cancer diagnosed by intraoperative colonoscopy. Nihon Rinsho Geka Gakkai Zasshi 2021;82:1401-6. [Crossref]
- Nonogaki I, Sunagawa Y, Nakagawa N, et al. Two Cases of Colorectal Cancer with Intussusception. Nihon Noson Geka Igakkai Zasshi 2019;68:71-6.
Cite this article as: Doita S, Taniguchi F, Ogawa T, Watanabe M, Tanakaya K, Aoki H. Two cases of sigmoid colon cancer with intussusception prolapsing through the anus in adults: consideration of preoperative reduction and surgical approaches: case reports. AME Case Rep 2024;8:61.






