
First case report of benign subcutaneous thyroid tissue implantation following transoral endoscopic thyroidectomy vestibular approach (TOETVA)
Highlight box
Key findings
• Thyroid tissue spillage while extracting thyroid specimen from vestibular incision could result in subcutaneous thyroid tissue implantation or seeding benign thyroid tumor.
What is known and what is new?
• Transoral endoscopic thyroidectomy vestibular approach (TOETVA) was approved for its safety equivalence to open traditional thyroidectomy.
• Intracorporeal thyroid tissue breakage and spillage should always be aware while performing TOETVA to prevent the thyroid tissue implantation.
What is the implication, and what should change now?
• Awareness of tissue damage and spillage is essential throughout the entire TOETVA procedure, including ensuring that the specimen remains securely within the retrieval bag during extraction. The risks of tissue rupture, potential misinterpretation, and the necessity of an additional incision, such as the axillary or submandibular incision, should be thoroughly discussed with patients presenting with large nodules.
Introduction
In 2014, the initial attempt to perform a transoral thyroid/parathyroidectomy used a sublingual approach, which was promptly forbidden due to complications and injury to the floor of the mouth (1-3). The following attempt which used a 2.5 cm single vestibular incision in the transoral video-assisted neck surgery (TOVANS) technique, was associated with a significant risk of mental nerve injury (4). Eventually, in 2016, the transoral endoscopic thyroidectomy vestibular approach (TOETVA) was developed without any major complications (5,6). Since then, TOETVA has been adopted globally, not only because of its safety equivalent to conventional open thyroidectomy but also because it overcame the limitations of earlier remote assessment modalities including shortened dissected surgical tracts, a more familiar surgical view, and patient satisfaction with the ideal aesthetic outcomes (5-12).
Aside from the potential complications in remote access thyroidectomy such as flap injury, vascular injury, hematoma, recurrent laryngeal nerve palsy or injury, trachea injury, and hypoparathyroidism, however, there were extremely rare late complication such as the subcutaneous thyroid tissue implantation (10,12).
Subcutaneous thyroid tissue implantation or seeding of benign thyroid tumor could be occurred from 1 year up to 26 years after thyroidectomy following conventional open surgery or remoted access approach (13-18). There have been 5 reports of subcutaneous implantation in remote access thyroid surgery occurring between 3 and 8 years after surgery while four of these were transaxillary approach and the other was transcervical endoscopic approach (14,15,19,20). However, the benign subcutaneous implantation has still never been reported in TOETVA technique. We present this article in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-24-15/rc).
Case presentation
A 28-year-old female had previously undergone right lobe TOETVA 4 years prior to her arrival [2018] due to a right thyroid nodule measuring 3.1 cm × 2.4 cm × 1.7 cm. The operation was successful without intraoperative complication. However, the retrieval bag was accidentally torn during extracting the specimen. We utilized a medical-grade polypropylene bag for retrieval. Upon discovering the tear, we carefully reinserted the specimen and proceeded with extraction using another retrieval bag. Following the extraction, we meticulously removed any remaining visible thyroid tissue and irrigated the surgical field with 1 liter of hypo-osmolar fluid to minimize the leftover tissue. However, there still remained a possibility of goiter cells seeding throughout the surgical field.
The pathological report was a nodular goiter with cystic degeneration, in which the capsule had been previously ruptured. After the surgical procedure had been performed, the patient had a regular follow-up for 6 months without further complications.
Two years after the surgery [2020], the patient started to feel small nodules on her left submandibular area. Eventually, 4 years after the initial surgery [2022], she decided to visit our surgical department after the nodule grew bigger and could be seen from the external surface. She had two moveable, round, firm-consistency nodules located in the left submandibular area, measuring 1 and 1.5 cm, and two small nodules, measuring 0.5 cm, located in the right submandibular area (Figures 1-3). The sonography showed multiple nodules up to 1.5 cm along the submandibular area (Figures 4,5), while the cytology reports were benign thyroidal tissues. Thyroid function tests showed euthyroid [free triiodothyronine (FT3), 2.610 pg/mL; free thyroxine (FT4), 0.91 ng/dL; thyroid stimulating hormone (TSH), 2.232 mIU/L].
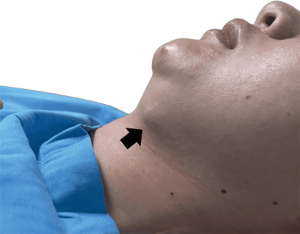

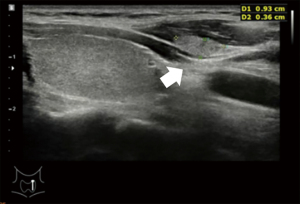

Therefore, the patient underwent an open excision of the bilateral cervical nodule under general anesthesia, with intraoperative ultrasonography performed to assess the existing remaining thyroid nodule. The intraoperative findings showed three left submandibular nodules sized 0.5, 1, and 1.5 cm beneath the platysma and two right submandibular nodules sized 0.5 and 0.5 cm beneath the right thyrohyoid muscle (Figure 6). The operation was performed without any complication, and the pathological results were shown as nodular hyperplasia. At the 6-month follow-up after surgery, ultrasonography revealed no nodule recurrence.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Based on previous literature, hypotheses for the recurrence of tumors along the surgical tract, whether benign or malignant, encompass various factors, including the potential rupture of a nodule during surgical manipulation, which could result in the implantation of tumor cells, the repeated minor trauma inflicted by rigid endoscopic instruments during surgery might prompt the exfoliation of cells from the tumor, and the “chimney effect”, where insufflation gas leaks through port sites, possibly carrying tumor cells along the surgical path (13,21-24).
However, in this scenario, the presence of implanted nodules is clarified as a result of tissue spillage that occurred while extracting the specimen through the vestibular incision. Consequently, fragments of the nodules were left in the vicinity of the port insertion sites, possibly remaining undetectable or inaccessible for removal during the procedure. Additionally, we attempt to rinse with hypo-osmolar fluid to facilitate the swelling and rupture of exfoliated cells in a hypo-osmolar environment before concluding the procedure (15).
Another major concern involves optimizing the nodule size criteria for performing TOETVA without interfering pathological interpretation. In our experience, patients with a smaller jaw and more prominent chin were associated with difficulty in tissue removal. According to our current protocol, we routinely extend the vestibular incision to 20–25 mm, which aligns with the consideration that mental foramens are located between the mandibular canine and the first molar. Extending the incision to this length may help with tissue extraction without causing mental nerve damage, particularly in patients with wider intercanine distances (25).
For benign nodules meeting specific criteria, such as oval shape, soft or spongy consistency, a diameter not exceeding 5 cm, extraction through this incision is feasible. Otherwise, the specimen would be extracted through a separate axillary incision. Additionally, we consider partially cutting the larger nodule within the retrieval bag for easier tissue extraction and repair the capsule before sending the specimen to the pathologist.
In cases of malignancy, we observed that the tissue tends to be notably firm and dense, making it challenging to extract the specimen through a smaller vestibular incision. Moreover, there is a concerning risk of tumor spillage below the jaw, potentially necessitating subsequent major surgery (23,26). To mitigate these risks, we adhered strictly to the findings of prior studies, which indicated that nodules smaller than 20 mm could be safely removed from a vestibular incision without causing mental nerve injury or specimen fracture, achieving a specificity rate of 100% (27). However, in instances where patients insist on undergoing TOETVA for cancerous nodules measuring 2–3 centimeters, we engage in thorough discussions regarding the associated risks including the potential for tumor rupture during specimen extraction, the challenge of accurately interpreting tumor margins, and the likelihood of requiring additional incisions for specimen extraction.
Furthermore, not only intracorporeal tissue breakages could result in tissue spillage but also potentially compromising the pathological results in doubtful nodules, such as those classified as Bethesda III/IV, which reported up to 40% malignancy potential (28). Various methods for extracting larger nodules, such as separated transaxilla incision, retroauricular facelift approach, or submandibular incision, have been discussed and require thorough evaluation, especially in cases of Bethesda III/IV tumors (29).
Even though there were no absolute guidelines or contraindications for patient selection in TOETVA, an awareness of tissue breakage and spillage should always be taken into consideration. The optimal case selection for vestibular removal, which would reduce complications and misinterpretation of pathological outcomes, still required additional research.
Conclusions
Throughout the entire TOETVA procedure, meticulous dissection should be conducted to maintain awareness of tissue damage and spillage, while it is crucial to ensure that the specimen remains securely within the retrieval bag during the specimen extraction. The risks of tissue rupture, potential misinterpretation, and the necessity of an additional incision, such as the axillary or submandibular incision, should be thoroughly discussed with patients presenting with large nodules.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-24-15/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-24-15/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-24-15/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Karakas E, Steinfeldt T, Gockel A, et al. Transoral parathyroid surgery--a new alternative or nonsense? Langenbecks Arch Surg 2014;399:741-5. [Crossref] [PubMed]
- Karakas E, Steinfeldt T, Gockel A, et al. Transoral thyroid and parathyroid surgery--development of a new transoral technique. Surgery 2011;150:108-15. [Crossref] [PubMed]
- Wilhelm T, Metzig A. Endoscopic minimally invasive thyroidectomy (eMIT): a prospective proof-of-concept study in humans. World J Surg 2011;35:543-51. [Crossref] [PubMed]
- Nakajo A, Arima H, Hirata M, et al. Trans-Oral Video-Assisted Neck Surgery (TOVANS). A new transoral technique of endoscopic thyroidectomy with gasless premandible approach. Surg Endosc 2013;27:1105-10. [Crossref] [PubMed]
- Anuwong A, Ketwong K, Jitpratoom P, et al. Safety and Outcomes of the Transoral Endoscopic Thyroidectomy Vestibular Approach. JAMA Surg 2018;153:21-7. [Crossref] [PubMed]
- Anuwong A. Transoral Endoscopic Thyroidectomy Vestibular Approach: A Series of the First 60 Human Cases. World J Surg 2016;40:491-7. [Crossref] [PubMed]
- Zhang D, Park D, Sun H, et al. Indications, benefits and risks of transoral thyroidectomy. Best Pract Res Clin Endocrinol Metab 2019;33:101280. [Crossref] [PubMed]
- Anuwong A, Sasanakietkul T, Jitpratoom P, et al. Transoral endoscopic thyroidectomy vestibular approach (TOETVA): indications, techniques and results. Surg Endosc 2018;32:456-65. [Crossref] [PubMed]
- Bakkar S, Al Hyari M, Naghawi M, et al. Transoral thyroidectomy: a viable surgical option with unprecedented complications-a case series. J Endocrinol Invest 2018;41:809-13. [Crossref] [PubMed]
- Fernandez-Ranvier G, Meknat A, Guevara DE, et al. Transoral Endoscopic Thyroidectomy Vestibular Approach. JSLS 2019;23:e2019.00036.
- Russell JO, Razavi CR, Shaear M, et al. Transoral Vestibular Thyroidectomy: Current State of Affairs and Considerations for the Future. J Clin Endocrinol Metab 2019;104:3779-84. [Crossref] [PubMed]
- Akritidou E, Douridas G, Spartalis E, et al. Complications of Trans-oral Endoscopic Thyroidectomy Vestibular Approach: A Systematic Review. In Vivo 2022;36:1-12. [Crossref] [PubMed]
- Lee YS, Yun JS, Jeong JJ, et al. Soft tissue implantation of thyroid adenomatous hyperplasia after endoscopic thyroid surgery. Thyroid 2008;18:483-4. [Crossref] [PubMed]
- Kim HS, Kim SH, Kim JH, et al. Multifocal hot spots demonstrated by whole-body 131I scintigraphy and SPECT/CT after transaxillary endoscopic thyroidectomy. Clin Nucl Med 2015;40:260-2. [Crossref] [PubMed]
- Fregoli L, Bakkar S, Papini P, et al. First report of benign track seeding after robot-assisted transaxillary thyroid surgery. Am J Otolaryngol 2021;42:102811. [Crossref] [PubMed]
- Liu Y, Li ZY. DU YP. Subcutaneous implantation of benign thyroid tissue: a rare complication after thyroidectomy. Chin Med J (Engl) 2011;124:1111-3. [PubMed]
- Takei I, Ito T, Mori T, et al. Subcutaneous Thyroid Tissue Implantation after Thyroidectomy: A Mimic of Benign Cutaneous Tumours. Acta Derm Venereol 2023;103:adv00842. [Crossref] [PubMed]
- Harach HR, Cabrera JA, Williams ED. Thyroid implants after surgery and blunt trauma. Ann Diagn Pathol 2004;8:61-8. [Crossref] [PubMed]
- Rossi L, Buoni V, Fregoli L, et al. Postsurgical complications after robot-assisted transaxillary thyroidectomy: critical analysis of a large cohort of European patients. Updates Surg 2022;74:511-7. [Crossref] [PubMed]
- Espiard S, Petyt G, Lion G, et al. Ectopic Subcutaneous Implantation of Thyroid Tissue After Gasless Transaxillary Robotic Thyroidectomy for Papillary Thyroid Cancer. Thyroid 2015;25:1381-2. [Crossref] [PubMed]
- Koh KW, Lee TH, Cho SY, et al. Subcutaneous implantation of adenomatous goiter: an unpredicted complication of endoscopic thyroid surgery. Thyroid 2010;20:441-3. [Crossref] [PubMed]
- Hubens G, Pauwels M, Hubens A, et al. The influence of a pneumoperitoneum on the peritoneal implantation of free intraperitoneal colon cancer cells. Surg Endosc 1996;10:809-12. [Crossref] [PubMed]
- Oh MY, Oh SW, Kim YA, et al. Seeding recurrence of follicular thyroid carcinoma after transoral endoscopic thyroidectomy vestibular approach: a case report. Gland Surg 2024;13:265-73. [Crossref] [PubMed]
- Soengas MS, Mateo CR, Salas M, et al. Structural features of phi29 single-stranded DNA-binding protein. I. Environment of tyrosines in terms of complex formation with DNA. J Biol Chem 1997;272:295-302. [Crossref] [PubMed]
- Greenstein G, Tarnow D. The mental foramen and nerve: clinical and anatomical factors related to dental implant placement: a literature review. J Periodontol 2006;77:1933-43. [Crossref] [PubMed]
- Kim Y, Lee JS, Yun HJ, et al. Tract Site Seeding of Papillary Thyroid Cancer After Transoral Endoscopic Thyroidectomy: A Case Report. Journal of Endocrine Surgery 2023;23:127-32. [Crossref]
- Wu YJ, Chi SY, Elsarawy A, et al. What is the Appropriate Nodular Diameter in Thyroid Cancer for Extraction by Transoral Endoscopic Thyroidectomy Vestibular Approach Without Breaking the Specimens? A Surgicopathologic Study. Surg Laparosc Endosc Percutan Tech 2018;28:390-3. [Crossref] [PubMed]
- Cibas ES, Ali SZ. The 2017 Bethesda System for Reporting Thyroid Cytopathology. Thyroid 2017;27:1341-6. [Crossref] [PubMed]
- Karakas E, Klein G, Schopf S. Transoral thyroid surgery vestibular approach: does size matter anymore? J Endocrinol Invest 2020;43:615-22. [Crossref] [PubMed]
Cite this article as: Laohathai S, Jamikorn T, Anuwong A. First case report of benign subcutaneous thyroid tissue implantation following transoral endoscopic thyroidectomy vestibular approach (TOETVA). AME Case Rep 2024;8:73.




