
Remarkable recovery following prolonged out-of-hospital cardiac arrest: hypoxic-ischemic encephalopathy (HIE) versus posterior reversible encephalopathy syndrome (PRES)—a case report
Highlight box
Key findings
• The study aims to highlight the significance of early cardiopulmonary resuscitation (CPR), emphasizing various factors contributing to enhanced outcomes post-cardiac arrest, including the initial rhythm’s predictive value for mortality and morbidity. Furthermore, it explores the role of imaging in conjunction with clinical assessment for diagnosing and anticipating outcomes.
What is known and what is new?
• Early resuscitation specifically in witnessed arrest would favor a better outcome.
• Initial rhythm is a key factor in predicting the prognosis after CPR.
• Despite the extensive data available in the literature, there may be exceptions to the rule. For instance, a complete recovery was observed in our patient despite all her poor prognostic factors.
• In managing such patients, it is crucial to integrate radiological findings and adopt a multidisciplinary approach. Relying solely on clinical assessment or radiological findings may not suffice; rather, they should complement each other seamlessly.
What is the implication, and what should change now?
• Increased focus on out-of-hospital cardiac arrests is essential, along with expanded campaigns to educate people on how to respond effectively in such emergencies. These efforts aim to reduce mortality rates stemming from cardiac arrests, addressing gaps in knowledge regarding resuscitation techniques.
• Emphasizing the significance of imaging, even in patients with poor prognoses, is vital for assessing the potential reversibility of brain damage caused by cardiac arrest.
Introduction
Out-of-hospital cardiac arrest (OHCA) is an increasingly prevalent medical emergency, posing significant challenges for healthcare providers and often leading to devastating outcomes for patients and their families. Globally, it stands as one of the primary causes of mortality. While the majority of OHCAs stem from cardiac-related issues, especially coronary artery disease (CAD) and acute coronary syndrome, various non-cardiac factors, such as trauma and respiratory complications, can also precipitate these events.
Cardiopulmonary resuscitation (CPR) aims to partially sustain cerebral blood flow, albeit at suboptimal levels, crucial for preserving cellular structure and metabolic function. However, research suggests that a substantial proportion of those who achieve return of spontaneous circulation (ROSC) after CPR ultimately succumb to their injuries. Factors such as the duration of CPR, the type of cardiac rhythm during the arrest, and the environment of the arrest can influence outcomes, often making the physician’s decisions during resuscitation especially challenging.
In addition to that, it was documented that following cardiac arrest cerebral physiological state is severely affected and expected to be worse with OHCA. The primary severe outcome for the brain is hypoxic-ischaemic brain injury (HIBI), which can result in significant levels of disability, a consistent vegetative condition, or even fatality (1).
Recent advances in medical imaging have provided invaluable insights into the neurological outcomes following OHCA. Timely and appropriate use of imaging modalities, coupled with expert interpretation, can significantly impact the diagnosis and potential prognosis of these patients. Particularly, understanding the interplay between conditions like posterior reversible encephalopathy syndrome (PRES) and hypoxic-ischemic encephalopathy (HIE)—both of which manifest distinct radiological features—can be pivotal in tailoring patient management.
PRES is an entity with clinical and radiological features with good prognosis usually. The association of PRES with cardiac arrest is rare and few case reports were found (2-4). We present this article in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-23-218/rc).
Case presentation
A 60-year-old female patient was brought to the emergency department after a sustained OHCA two times consecutively in the house and CPR was initiated by her son and continued by the national ambulance team upon their arrival achieved ROSC after 27 minutes. Furthermore, another cardiac arrest developed on the way in ambulance on pulseless electrical activity (PEA) rhythm and ROSC was achieved after 4 minutes, then arrested lastly in the emergency department for 4 minutes then again ROSC was achieved, CPR throughout was done following advanced cardiovascular life support (ACLS) protocol with a duration from collapse to ROSC of 35 minutes. In the ER, arterial blood gasses (ABGs) were withdrawn, and results are shown in Table 1.
Table 1
| Blood gas | Result |
|---|---|
| PH | 7.18 |
| PCO2, mmHg | 26 |
| PO2, mmHg | 173 |
| HCO3, mmol/L | 9.6 |
She had an initial rhythm of PEA and an initial electrocardiogram (ECG) rhythm of an old left bundle branch block (LBBB), the following ECG are on admission, follow up and on discharge respectively (Figures 1-3).
The patient after that was intubated and shifted to the intensive care unit (ICU) with high ventilatory support. The background of her medical history includes diabetes, hypertension, congestive heart failure, and hypothyroidism as her medical therapy she was on Entresto 50 mg bid, carvedilol 25 mg bid, ivabradine 5 mg bid, levothyroxine 100 mcg, gliclazide 60 mg, metformin 1,000 mg bid and dapagliflozin 10 mg.
The patient had undergone a coronary angiogram 3 years before the date of admission, which showed moderate left circumference (LCX) disease and mild proximal left anterior descending (LAD) disease. An echocardiogram was done 1 year before admission and showed an ejection fraction of 49%, mild global hypokinesis with abnormal jerky septal contraction, with features of dilated cardiomyopathy.
The cruciality of her situation led to the management by a multidisciplinary team to achieve the best outcome after the survival of sudden cardiac death.
Initially while in the emergency, computed tomography (CT) brain was done after ROSC and it showed dilatation of the ventricular system without shift of the midline structures, central and cortical involutional brain changes. A CT pulmonary embolism (PE) scan was done, and PE was excluded. The scan also showed mild cardiomegaly, mild bilateral effusion and bilateral extensive consolidation suggested to be due to heart failure (Figure 4).
Immediately after completion of imaging studies, she was admitted to the ICU on high vasopressor support, with norepinephrine and vasopressin. Glasgow Coma Scale (GCS) assessment revealed 3/15. She was put on maximum ventilatory support with fractional inspired oxygen of 100%, synchronized intermittent mandatory ventilation (SIMV) and positive end expiratory pressure (PEEP) of 10.
The provisional diagnosis was a mixed cardiogenic and septic shock. During her ICU stay, she developed an acute kidney injury (AKI) and CRRT was initiated. Cultures from sputum, blood and urine were collected and empirical antibiotics were started.
Echocardiography on admission, showed ejection fraction of 30–35%, hypokinesia of the apex, lateral and anterior walls, grade I diastolic dysfunction and mild mitral regurgitation. In view of extensive bilateral consolidations in initial CT PE and rising sepsis markers, infectious disease was consulted on the 2nd day of admission which suggested the possibility of aspiration pneumonitis during CPR and recommended to repeat CT chest high resolution (HR). Hence CT scans of brain and CT HR were repeated, in which brain CT showed normal result (Figure 5), and CT HR revealed minimal pleural effusion on the right with minimal basal lung collapse.
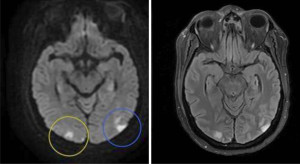
During the ICU stay, several other complications developed including disseminated intravascular coagulation (DIC) in which international normalized ratio (INR) was raised to 3 and platelets dropped to 83,000 per microliter, ischemic hepatitis in view of high liver enzymes and features suggestive of adult respiratory distress syndrome. On the fourth day of admission, the decision was to halt sedation to assess her neurological status, which showed gradual improvement in the following days. On the sixth day of admission, an electroencephalogram (EEG) followed, which revealed a picture of encephalopathy. On the eighth day of admission, a magnetic resonance imaging (MRI) study of the brain (Figure 6) using diffusion weighted imaging (DWI) series showed localized area of restricted diffusion with low apparent diffusion coefficient (ADC) map value in the cortical and subcortical areas of the posterior occipital regions of both cerebral hemispheres. The lesions correspond to an area of hyperintensity in the fluid attenuated inversion recovery (FLAIR) series. The susceptibility weighted imaging (SWI) series revealed no evidence of a haemorrhagic nature. Otherwise, normal features and signal intensities of both cerebral hemispheres along with normal age related involutional changes and prominence of the cerebral sulci and ventricular system are present.
On the 11th day of discontinuation of sedation (15th day post admission), the patient was extubated successfully. She was conscious and obeying commands. Nonetheless, she developed features of critical illness myopathy and evidence of oropharyngeal dysphagia following extubation. Interestingly all these complications were managed with the concerned specialties involving intense physiotherapy sessions.
She was then discharged out of the ICU after 24 days and a repeated echo showed improved systolic function and ejection fraction of 50%. However, she needed readmission to the ICU 2 days after ICU discharge due to acute pulmonary edema and intubation took place on the scene and was shifted back to the ICU. Angiography was done on the same day as an emergency (no new changes in the ECG with previously detected LBBB) and revealed normal study.
A multidisciplinary team following the case daily included neurologists, cardiologists, intensivists, respiratory therapists, and electrophysiology study (EPS) team. On the 23rd day, an implantable cardioverter-defibrillator (ICD), single chamber ICD implantation was done after coronary angiography. Followed by a discharge from the ICU 2 days later to the medical ward and a discharge from the hospital after 37 days. She was conscious and alert, requiring physiotherapy and regular follow up with cardiology and the EPS team.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committees and with the Helsinki Declaration (as revised in 2013). Informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
OHCA is a major health problem worldwide and has grabbed attention recently due to its unpredictability, low survival rates, and an increase in cases globally (5,6). Numerous studies in the United Arab Emirates (UAE) demonstrated similar results, especially after the establishment of the National Ambulance of the U.A.E which in return is a contributing member to the Pan-Asian Resuscitation Outcomes Study (PAROS), an international cardiac arrest registry study concerned with OHCA (7). As of 2023, according to data from the World Health Organization (WHO), non-communicable diseases (NCDs) are responsible for 77% of all fatalities in the UAE, with cardiovascular diseases (CVDs) contributing to 40% of these cases. Previous studies conducted in the UAE have demonstrated low ROSC rates, bystander CPR in more than half of the cases and an overall low survival rate as seen in international studies (8-10).
CPR duration varies significantly among different patient characteristics. Multiple efforts have been attempted to determine the upper limit of CPR duration beyond which it would be futile (11-13). As per the emergency medical service in the United States and Western countries, the rule to terminate CPR efforts and to declare a patient’s death vary from 20 to 30 minutes (14-16). In a study including approximately 420,000 OHCA patients without achieving ROSC, it was found that extending CPR by more than 26 minutes is futile. Moreover, OHCA patients with an initial shockable rhythm, witnessed arrest, and <75 years of age had better neurological outcomes with shorter durations of CPR, and the longer the duration the worse the outcome (11). Interestingly, as in our case of OHCA with a CPR duration of 44 minutes and a witnessed arrest along with a non-shockable rhythm with immediate bystander CPR, some of OHCA patients in another study who had a witnessed arrest, and an initial non-shockable rhythm had a favorable neurological outcome after similar CPR duration (17). Although termination of resuscitation is considered applicable if the efforts made were futile, there are no clear cutoff points to decide when to determine the end of the process and a lot of factors must be considered.
The detrimental effect of cardiac arrest on the nervous system is one of the leading causes of mortality in cardiac arrest patients (18). Around ten percent of the patients tend to have favorable neurological outcomes (19). The MIRACLE2 score is a tool used as an early predictor of neurological outcomes in OHCA patients. A score of ≥5 predicts poor neurological outcome with a specificity of 92.3%. Our patient had a risk score of 6. Although her arrest was witnessed but it was characterized by extended CPR time, her initial rhythm was non shockable, her pupils were dilated and non-reactive at ROSC, age of 60 years old and was comorbid, she was acidotic with a pH was 7.18, and she was administered epinephrine.
In one study, delayed recovery was related to the duration of sedation as using long- acting sedatives, hemodynamic shock, poor kidney function and old age. Compared to sedation cessation for a period of 4 days in our case, patients recovering after 4 days, or more were found to be subjected to severe neurological disability (20,21).
Neurological outcomes post prolonged cardiac arrest are influenced significantly by the initial rhythm and arrest time. Multiple studies have demonstrated better outcomes with time from collapse to ROSC <20 minutes and initial rhythm of ventricular fibrillation (VF) or ventricular tachycardia (VT). However, our patient had an almost normal return to function with a duration to ROSC of >20 minutes and an initial rhythm with a PEA which does not coincide with other articles (22-24). The patient, despite prolonged low-flow time and non-shockable rhythm, exhibited remarkable survival and neurological recovery, challenging some established notions.
Although it is often noted that patients who experience OHCA and receive extended CPR followed by hypoxic or anoxic brain injury typically do not achieve favorable outcomes, our situation witnessed a remarkable neurological recuperation (25).
As per radiological findings, there were two different etiologies, which were PRES and HIE. These findings were discussed with the neurology team following up with the patient since her admission. PRES is an acute mostly reversible clinical radiological diagnosis whose pathophysiology remains unclear but is multifactorial in nature, triggered by various conditions, including hypertensive encephalopathy, eclampsia, certain medications, renal disease, autoimmune diseases, sepsis, and transplant rejection. It is more prevalent in females, which can be explained by its potential link to autoimmune diseases. High suspicion must be granted in hypertensive patients with neurological sequelae. The diagnosis is established by evaluating clinical and radiographic evidence with a focus on symptoms such as headache, changes in mental status, seizures, and the presence of restricted diffusion on DWI scans. In contrast to our case, the diagnosis was hindered inapplicable due to the patient’s circumstances as she was sedated, intubated and mechanically ventilated. We acknowledge the complexity in diagnosing PRES, particularly when CT scans may appear normal. Our decision to proceed with an MRI was based on a combination of factors including the EEG findings indicating encephalopathy and the patient’s clinical scenario suggesting a differential diagnosis that included PRES. This choice is supported by MRI’s superior sensitivity in detecting the radiologic hallmarks of PRES, which are not as readily apparent on CT scans. The case study places significant emphasis on the recognition of PRES in its early stages, as this has been shown to yield more favorable outcomes. The treatment of PRES involves managing the underlying cause and supportive care, including blood pressure control, fluid resuscitation, vasopressor support, anticonvulsants, sedatives, and possibly intubation and mechanical ventilation. The patient’s recovery in the case study is attributed to the team-based care approach, involving multidisciplinary coordination, which led to a favorable prognosis despite the complexity of the case.
HIE may be differentiated by its gyriform restricted diffusion and unfavorable resolution on follow up imaging. However, we find it important to note that some studies have emphasized the difficulty in distinguishing PRES from HIE (26,27).
Our patient had a pre-arrest cardiac disease that might explain her positive outcome which is seen in patients in other studies, and this could be explained by better interventions and treatment options. However, our patient had a non-VF/VT initial rhythm; this is inconsistent with other articles where VF/VT initial rhythms had lower mortality rates than the former (28,29).
We strongly believe awareness among intensive care physicians towards PRES shall increase especially with the existing neuroimaging modalities, especially that with early recognition and prompt management, it is not uncommon to have good outcomes.
It was declared that there is a generalized lack of knowledge in detecting OHCA, inconfidence in performing CPR and the element of cultural barriers which contributed significantly to the poor performance of CPR. Additionally, there is a limited number of public access to automated external defibrillators (AED) which we can target to highlight the importance of identifying the reasons.
Conclusions
OHCA is not uncommon around the world and in the UAE, hence stressing the importance of resuscitation for a better outcome is pivotal for survival. However, it is related to other factors including time of resuscitation, witnessed or not, and the initial rhythm that led to arrest.
This case study provides valuable insights into the complexities of managing cardiac arrest patients, the factors influencing recovery, and the importance of early diagnosis and treatment of conditions like PRES to prevent permanent neurological damage.
There is a generalized increase in cardiac arrest research, and we aim to contribute to the database and reinforce the efforts of the community and raise awareness to enhance the chain of survival.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-23-218/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-23-218/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-23-218/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committees and with the Helsinki Declaration (as revised in 2013). Informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sandroni C, D'Arrigo S, Nolan JP. Prognostication after cardiac arrest. Crit Care 2018;22:150. [Crossref] [PubMed]
- Kargl S, Hornath F, Rossegg U, et al. Status epilepticus, cardiac resuscitation, and posterior reversible encephalopathy syndrome after ingestion of viscous lidocaine: a plea for more childproof packaging of pharmaceuticals. Pediatr Emerg Care 2014;30:185-7. [Crossref] [PubMed]
- Ohashi E, Hayakawa I, Tsutsumi Y, et al. Central-variant posterior reversible encephalopathy syndrome in an infant with mid-aortic syndrome: A rare case of symmetric basal ganglia lesions. Radiol Case Rep 2022;17:3475-80. [Crossref] [PubMed]
- Fantini S, Sassaroli A, Tgavalekos KT, et al. Cerebral blood flow and autoregulation: current measurement techniques and prospects for noninvasive optical methods. Neurophotonics 2016;3:031411. [Crossref] [PubMed]
- Nadolny K, Zyśko D, Obremska M, et al. Analysis of out-of-hospital cardiac arrest in Poland in a 1-year period: data from the POL-OHCA registry. Kardiol Pol 2020;78:404-11. [Crossref] [PubMed]
- Sandroni C, Cronberg T, Sekhon M. Brain injury after cardiac arrest: pathophysiology, treatment, and prognosis. Intensive Care Med 2021;47:1393-414. [Crossref] [PubMed]
- Doctor NE, Ahmad NS, Pek PP, et al. The Pan-Asian Resuscitation Outcomes Study (PAROS) clinical research network: what, where, why and how. Singapore Med J 2017;58:456-8. [Crossref] [PubMed]
- Batt AM, Al-Hajeri AS, Cummins FH. A profile of out-of-hospital cardiac arrests in Northern Emirates, United Arab Emirates. Saudi Med J 2016;37:1206-13. [Crossref] [PubMed]
- Blewer AL, Leary M, Decker CS, et al. Cardiopulmonary resuscitation training of family members before hospital discharge using video self-instruction: a feasibility trial. J Hosp Med 2011;6:428-32. [Crossref] [PubMed]
- Bürger A, Wnent J, Bohn A, et al. The Effect of Ambulance Response Time on Survival Following Out-of-Hospital Cardiac Arrest. Dtsch Arztebl Int 2018;115:541-8. [Crossref] [PubMed]
- Funada A, Goto Y, Tada H, et al. Duration of cardiopulmonary resuscitation in patients without prehospital return of spontaneous circulation after out-of-hospital cardiac arrest: Results from a severity stratification analysis. Resuscitation 2018;124:69-75. [Crossref] [PubMed]
- Reynolds JC, Frisch A, Rittenberger JC, et al. Duration of resuscitation efforts and functional outcome after out-of-hospital cardiac arrest: when should we change to novel therapies? Circulation 2013;128:2488-94. [Crossref] [PubMed]
- Grunau B, Reynolds JC, Scheuermeyer FX, et al. Comparing the prognosis of those with initial shockable and non-shockable rhythms with increasing durations of CPR: Informing minimum durations of resuscitation. Resuscitation 2016;101:50-6. [Crossref] [PubMed]
- Richmond S, Wyllie J. European Resuscitation Council Guidelines for Resuscitation 2010 Section 7. Resuscitation of babies at birth. Resuscitation 2010;81:1389-99. [Crossref] [PubMed]
- National Association of EMS Physicians and American College of Surgeons Committee on Trauma. Termination of resuscitation for adult traumatic cardiopulmonary arrest. Prehosp Emerg Care 2012;16:571. [Crossref] [PubMed]
- Millin MG, Khandker SR, Malki A. Termination of resuscitation of nontraumatic cardiopulmonary arrest: resource document for the National Association of EMS Physicians position statement. Prehosp Emerg Care 2011;15:547-54. [Crossref] [PubMed]
- Matsuyama T, Kitamura T, Kiyohara K, et al. Impact of cardiopulmonary resuscitation duration on neurologically favourable outcome after out-of-hospital cardiac arrest: A population-based study in Japan. Resuscitation 2017;113:1-7. [Crossref] [PubMed]
- Taccone FS, Picetti E, Vincent JL. High Quality Targeted Temperature Management (TTM) After Cardiac Arrest. Crit Care 2020;24:6. [Crossref] [PubMed]
- Dyson K, Brown SP, May S, et al. International variation in survival after out-of-hospital cardiac arrest: A validation study of the Utstein template. Resuscitation 2019;138:168-81. [Crossref] [PubMed]
- Rey A, Rossetti AO, Miroz JP, et al. Late Awakening in Survivors of Postanoxic Coma: Early Neurophysiologic Predictors and Association With ICU and Long-Term Neurologic Recovery. Crit Care Med 2019;47:85-92. [Crossref] [PubMed]
- Lybeck A, Cronberg T, Aneman A, et al. Time to awakening after cardiac arrest and the association with target temperature management. Resuscitation 2018;126:166-71. [Crossref] [PubMed]
- Aguila A, Funderburk M, Guler A, et al. Clinical predictors of survival in patients treated with therapeutic hypothermia following cardiac arrest. Resuscitation 2010;81:1621-6. [Crossref] [PubMed]
- Belliard G, Catez E, Charron C, et al. Efficacy of therapeutic hypothermia after out-of-hospital cardiac arrest due to ventricular fibrillation. Resuscitation 2007;75:252-9. [Crossref] [PubMed]
- Oddo M, Ribordy V, Feihl F, et al. Early predictors of outcome in comatose survivors of ventricular fibrillation and non-ventricular fibrillation cardiac arrest treated with hypothermia: a prospective study. Crit Care Med 2008;36:2296-301. [Crossref] [PubMed]
- Myat A, Song KJ, Rea T. Out-of-hospital cardiac arrest: current concepts. Lancet 2018;391:970-9. [Crossref] [PubMed]
- Hinduja A. Posterior Reversible Encephalopathy Syndrome: Clinical Features and Outcome. Front Neurol 2020;11:71. [Crossref] [PubMed]
- McKinney AM, Short J, Truwit CL, et al. Posterior reversible encephalopathy syndrome: incidence of atypical regions of involvement and imaging findings. AJR Am J Roentgenol 2007;189:904-12. [Crossref] [PubMed]
- Herlitz J, Engdahl J, Svensson L, et al. Factors associated with an increased chance of survival among patients suffering from an out-of-hospital cardiac arrest in a national perspective in Sweden. Am Heart J 2005;149:61-6. [Crossref] [PubMed]
- Martinell L, Larsson M, Bång A, et al. Survival in out-of-hospital cardiac arrest before and after use of advanced postresuscitation care: a survey focusing on incidence, patient characteristics, survival, and estimated cerebral function after postresuscitation care. Am J Emerg Med 2010;28:543-51. [Crossref] [PubMed]
Cite this article as: Singer N, Abdelbagi M, Alzuabi A, Elsayed MAM. Remarkable recovery following prolonged out-of-hospital cardiac arrest: hypoxic-ischemic encephalopathy (HIE) versus posterior reversible encephalopathy syndrome (PRES)—a case report. AME Case Rep 2024;8:89.







