
Idiopathic myointimal hyperplasia of the mesenteric veins—a report of two cases
Highlight box
Key findings
• Idiopathic myointimal hyperplasia of the mesenteric veins (IMHMV) is a very rare condition.
What is known and what is new?
• The diagnosis of IMHMV is challenge.
• A multidisciplinary team approach will be vital for the appropriate treatment in future cases.
What is the implication, and what should change now?
• The multidisciplinary approach needs to be the gold standard of treatment.
Introduction
Idiopathic myointimal hyperplasia of the mesenteric veins (IMHMV) is a rare condition that poses a diagnostic challenge to surgeons and pathologists alike (1-7). Both clinically and pathologically, it is often misdiagnosed as inflammatory bowel disease or ischemic colitis. IMHMV is part of a trilogy of distinct but closely related pathologic entities; mesenteric inflammatory veno-occlusive disease (MIVOD) and idiopathic mesenteric phlebosclerosis (IMP) (8,9). MIVOD is a venogenic intestinal disease that shares the intimal hyperplasia of the mesenteric veins observed in IMHMV. In contrast with IMHMV, inflammatory infiltration and/or fibrinoid necrosis of the mesenteric veins is observed, to the date were described 124 patients with IMHMV (10). IMP is a rare form of chronic ischemic colitis characterized by calcification of mesenteric veins and concurrent thickening of the right hemicolon wall (11). IMHMV is described as an ischemic bowel disease without the presence of thrombus or venous occlusion. The ischemia is a result of the proliferation of smooth muscle in the venous intima. Predictably, definitive diagnosis is often only made after operative resection. The first reported cases of IMHMV were a series of 4 patients by Genta and Haggitt in 1991 (1). During the past 3 decades, only 66 subsequent cases have been reported; however, etiology and pathophysiology of the disorder remain unknown. Our aim is to describe two cases of IMHMV requiring operative intervention (12,13). We present both cases in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-23-59/rc).
Case presentation
Case 1
A 37-year-old male with no significant past medical history was evaluated for a two-month history of abdominal pain, constipation, diarrhea and recent bleeding per rectum. This patient had undergone workup by both his primary care physician and an outside institution with the differential diagnosis presumed to be inflammatory bowel disease or ischemic colitis. Workup for infectious colitis was negative. He was placed on a course of empiric IV antibiotics without improvement. On admission to our institution, laboratory results were significant for leukocytosis of 18,000/mm3 and hemoglobin of 11.3 g/dL. Computed tomography (CT) scan revealed abnormal wall thickening with surrounding inflammatory changes and mesenteric edema involving the descending and sigmoid colon as well as the rectum. All three mesenteric vessels were noted to be patent without aneurysmal or significant occlusive disease. Subsequent flexible sigmoidoscopy demonstrated diffuse inflammation of the rectum and distal sigmoid with a 5 mm diametric stricture noted at 20 cm from the anal verge (Figure 1).
Biopsy sites did not bleed, raising concern for ischemia. Given these findings, the patient was taken to the operating room where he underwent a laparoscopic-assisted extended left colectomy with end colostomy. On abdominal survey, there was a markedly thickened and rigid left colon (Figure 2) and rectum with a slightly dilated but normal transverse colon. Initial histopathologic assessment demonstrated significant mucosal ulceration, hemorrhagic necrosis, transmural necrotizing acute inflammation, congestion and edema extending to the distal margin of resection, with viable mucosa at the proximal margin. The patient did well postoperatively and was ultimately meeting all goals for discharge by postoperative day 9. His case was then presented at our institutional Inflammatory Bowel Disease Conference where the specimen was reviewed by multiple pathologists who identified typical morphologic findings consistent with idiopathic myointimal hyperplasia of mesenteric veins.

Case 2
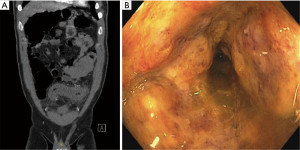
A 49-year-old male with a past medical history of hypertension, gastroesophageal reflux and recent coronavirus disease 2019 (COVID-19) infection was admitted to another hospital following several months of colitis of unknown etiology; unresponsive to antibiotics and steroids. He was ultimately transferred to our institution after developing saddle pulmonary embolism which was treated with thrombectomy and systemic anticoagulation. Although his respiratory status improved, he had worsening abdominal symptoms characterized by intractable pain, cramping, and bloody diarrhea. Laboratory results were significant for leukocytosis of 19,100/mm3, hemoglobin of 10.2 g/dL and an elevated C-reactive protein at 54.5 mg/L. Workup for infectious colitis was also unrevealing as in our first case. CT scan revealed concentric, severe mural thickening and intramural edema of the distal descending colon extending to the rectum consistent with proctocolitis. Flexible sigmoidoscopy demonstrated ischemic nonbleeding mucosa (Figure 3). On this premise, the patient was taken to the operating room where he underwent a laparoscopic-assisted low anterior resection with end colostomy with findings of an extremely indurated, thickened left colon and rectum (Figure 4). Histopathologic assessment revealed patchy ulceration, mucosal necrosis with pseudomembranes, edema and pericolonic inflammation with fat necrosis. Because of the clinical similarity to the above case, the histopathology was reviewed and found to be consistent with IMHMV (Figure 5).



The postoperative course was significant for prolonged hospital stay complicated by loculated pleural/intra-abdominal fluid collections requiring intravenous antibiotics and a CT-guided drainage. While the patient’s abdominal status improved, he developed an empyema requiring decortication. The patient recovered from these additional interventions and was discharged home in stable condition on postoperative day 32.
Ethical consideration
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committees and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
IMHMV is a rare disease characterized by myointimal proliferative changes that narrow the lumen of mesenteric veins resulting in a non-thrombotic ischemic injury of the intestinal tract. Most cases in the literature are that of healthy middle-aged men. The clinical presentation typically includes recurrent, progressive abdominal discomfort, accompanied by hematochezia, tenesmus, and diarrhea. The clinical course is often chronic and quite frequently refractory to antibiotics and systemic steroids. CT of the abdomen will often reveal both the localization of the disease involvement as well as the typical features of ischemic colitis. Commonly encountered findings of IMHMV on CT include segmental circumferential colonic wall thickening with poor mural enhancement, pericolic fat stranding and submucosal edema (14). One study investigating the angiographic features of IMHMV reported complete occlusion of the distal inferior mesenteric vein. This finding is posited as a way to differentiate IMHMV from other inflammatory bowel diseases that otherwise share the same CT findings—for example, ulcerative colitis was found to consistently have a patent inferior mesenteric vein (14). A recent review of published cases in the literature found the most encountered endoscopic features to be ulceration, mucosal congestion, friability, and stricture. Diffuse mucosal erythema and friability affected the rectosigmoid in all patients reviewed (15). In our two cases, in addition to these findings, non-bleeding tissue on biopsy was also noted.
Complete appreciation of the etiology of this disease remains unclear. Some studies have observed that the myointimal hyperplasia seen in the mesenteric veins is comparable to pathologic changes noted in failed saphenous vein grafts used in coronary bypass grafts (2). The basis of this alteration is 2-fold: adaptation of the graft secondary to arterial pressures and mechanical trauma to the endothelium causing fibrin extravasation. This informs one theory on the etiology of IMHMV. Some propose that the presence of an arteriovenous fistula increases venous blood flood flow—like saphenous vein grafts in coronary artery bypass grafts or arteriovenous fistulas for hemodialysis. Genta and Haggit proposed that the mesentery of the hypermobile sigmoid colon intermittently torses, causing stretching injury and subsequent arteriovenous fistula (1). At this juncture, however, no arteriovenous malformations have been noted on review of the literature or in our two cases. Additionally, this fails to account for the cases seen in other segments of the colon or small intestine.
To secure a diagnosis in a timely manner, we are left to wrestle with the task of identifying patterns in clinical presentation and imaging findings. Surgical resection has classically been considered the primary method of diagnosis. Gross specimens with IMHMV are most frequently described in the rectosigmoid colon, however, there have been instances of more proximal disease involving the descending colon, pancolonic involvement, (7) and even small bowel disease (5). Interestingly, intraoperative evaluation in both our cases demonstrated a more distal distribution of disease extending to the distal rectum. While histopathologic features have not been definitively identified for IMHMV, several reports have suggested features that can prompt the consideration of this pathology in appropriate patient populations. In one case report, IMHMV was diagnosed preoperatively based on nonspecific ischemic changes coupled with abnormal thickening of the slightly tortuous lamina propria veins with smudged eosinophilic staining (3). Another study further confirmed the presence of dilated, “arteriolized” capillaries lined by plump endothelial cells and fibrin deposits in the endothelium (4). These consistencies give credence to the eventual possibility of a timelier preoperative diagnosis.
While medical treatment has not yet been optimized, operative resection has been found to be curative, and thus, avoids complications inherent to progressive ischemia, malnutrition, and prolonged antibiotic/corticosteroid use. This case series looks to highlight the value of including IMHMV to the clinician’s diagnostic toolbox. At this juncture, our experience, as well as review of the literature, suggests that operative intervention with resection and not medical management, can be curative. Questions certainly remain for the postoperative period. In both of our cases, the remaining rectum was stapled and oversewn. The tentative plan will be to perform a follow-up proctoscopy to re-evaluate the rectum. While there have been no published reports of disease recurrence, the safety of possible reversal is difficult to establish, even in the setting of normal rectal mucosa.
Conclusions
The challenge going forward is accurately and systematically identifying factors from both a pathologic and clinical perspective that guide timely diagnosis and avoid unnecessary treatment. Clinicians should have a high index of suspicion when encountering patients with colitis refractory to treatment, CT angiography negative for arterial occlusion and biopsy demonstrating changes consistent with ischemia in the absence of other biopsy findings specific to inflammatory bowel disease. Undoubtedly, a multidisciplinary team approach to this condition will be vital to administering the appropriate treatment modalities for future cases of IMHMV.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-23-59/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-23-59/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-23-59/coif). L.B.L. serves as an unpaid editorial board member from May 2023 to April 2025. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committees and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Genta RM, Haggitt RC. Idiopathic myointimal hyperplasia of mesenteric veins. Gastroenterology 1991;101:533-9. [Crossref] [PubMed]
- Abu-Alfa AK, Ayer U, West AB. Mucosal biopsy findings and venous abnormalities in idiopathic myointimal hyperplasia of the mesenteric veins. Am J Surg Pathol 1996;20:1271-8. [Crossref] [PubMed]
- Wangensteen KJ, Fogt F, Kann BR, et al. Idiopathic Myointimal Hyperplasia of the Mesenteric Veins Diagnosed Preoperatively. J Clin Gastroenterol 2015;49:491-4. [Crossref] [PubMed]
- Li H, Shu H, Zhang H, et al. Idiopathic Myointimal Hyperplasia of the Mesenteric Veins: A Case Report and Scoping Review of Previously Reported Cases From Clinical Features to Treatment. Front Med (Lausanne) 2022;9:855335. [Crossref] [PubMed]
- Song SJ, Shroff SG. Idiopathic Myointimal Hyperplasia of Mesenteric Veins of the Ileum and Colon in a Patient with Crohn's Disease: A Case Report and Brief Review of the Literature. Case Rep Pathol 2017;2017:6793031. [Crossref] [PubMed]
- Almumtin A, Al Sulais E, Elhag MA. Idiopathic Myointimal Hyperplasia of Mesenteric Veins (IMHMV) with two spontaneous bowel perforations: A case report and literature review. Int J Surg Case Rep 2021;83:106022. [Crossref] [PubMed]
- Korenblit J, Burkart A, Frankel R, et al. Refractory pancolitis: a novel presentation of idiopathic myointimal hyperplasia of mesenteric veins. Gastroenterol Hepatol (N Y) 2012;8:696-700. [PubMed]
- Al Ansari A, Ahmed S, Mansour E, et al. Idiopathic myointimal hyperplasia of the mesenteric veins. J Surg Case Rep 2021;2021:rjaa453. [Crossref] [PubMed]
- Yamada K, Hiraki M, Tanaka T, et al. A case of idiopathic myointimal hyperplasia of the mesenteric veins presenting with small bowel obstruction. Surg Case Rep 2021;7:17. [Crossref] [PubMed]
- Rozner R, Gisriel S, Damianos J, et al. Idiopathic myointimal hyperplasia of the mesenteric veins: A systematic review and individual patient data regression analysis. J Gastroenterol Hepatol 2023;38:1040-6. [Crossref] [PubMed]
- Wen Y, Chen YW, Meng AH, et al. Idiopathic mesenteric phlebosclerosis associated with long-term oral intake of geniposide. World J Gastroenterol 2021;27:3097-108. [Crossref] [PubMed]
- Ayres LRO, Scott M, Shepherd N, et al. An unusual case of mesenteric ischaemia. Frontline Gastroenterol 2014;5:36-9. [Crossref] [PubMed]
- Fang C, Liao X, Lu X. An Acute Progressive Ischemic Enteritis in a Young Patient. Gastroenterology 2021;161:e11-3. [Crossref] [PubMed]
- Yun SJ, Nam DH, Kim J, et al. The radiologic diagnosis of idiopathic myointimal hyperplasia of mesenteric veins with a novel presentation: case report and literature review. Clin Imaging 2016;40:870-4. [Crossref] [PubMed]
- Yantiss RK, Cui I, Panarelli NC, et al. Idiopathic Myointimal Hyperplasia of Mesenteric Veins: An Uncommon Cause of Ischemic Colitis With Distinct Mucosal Features. Am J Surg Pathol 2017;41:1657-65. [Crossref] [PubMed]
Cite this article as: Uwah M, Bustamante-Lopez L, Devane L, Hoff J, Garcia-Henriquez N, Kline B, Monson JRT, Albert M. Idiopathic myointimal hyperplasia of the mesenteric veins—a report of two cases. AME Case Rep 2024;8:84.


