
Breast cancer with cervix, lung and neck metastases: a case report and literature review
Highlight box
Key findings
• Breast cancer has the potential to metastasize to various sites; however, cases of metastasis to the cervix are rare. Here, we present clinical and pathological data from a rare case of primary breast cancer metastasis to the cervix, lung and neck.
What is known and what is new?
• Breast cancer metastases to other sites has been often seen like lungs, pleura, bones, liver, and brain.
• Breast cancer metastases to the cervix are rarely seen. We report a case of primary breast cancer metastases to the cervix, lung and neck.
What is the implication, and what should change now?
• Cervical metastasis is rare in patients with breast cancer, and most commonly presents as vaginal bleeding; however, there may also be no symptoms initially, and regular cervical cytology screening and/or gynecologic ultrasonography can assist in early detection of cervical lesions.
Introduction
Among malignant tumors, breast cancer has the highest incidence rate and results in the most mortality of women worldwide (1). In addition to axillary lymph nodes, tumor metastasis can also occur in non-axillary lymph nodes, lungs, pleura, bones, liver, and brain (2-4). Rare locations of metastasis include the stomach (5), rectum (6,7), pancreas (8), spleen, thyroid gland, adrenal glands (9), kidneys, heart, vagina (10), uterus, and ovaries; however, cases of metastasis to the cervix are particularly rare. Now we present clinical and pathological data from a rare case of primary breast cancer metastasis to the cervix, including imaging characteristics and clinical progression. We present this case in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-24-36/rc).
Case presentation
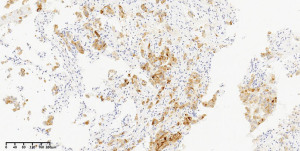
A 68-year-old female patient sought treatment at our hospital due to self-detected nodules in her right breast. B-ultrasound examination revealed multiple nodules in the right breast, classified as Breast Imaging Reporting and Data System (BI-RADS) 4c. There was no history of breast cancer in her family. Radical treatment for breast cancer was considered after ruling out contraindications. Histopathologic diagnosis revealed invasive ductal breast carcinoma of non-specific type, with intraductal carcinoma in the right breast (Figures 1,2). Of 15 axillary lymph nodes examined, 11 were positive for cancer cells, while 2 of 3 sentinel lymph nodes analyzed showed signs of metastasis. Immunohistochemical results indicated: androgen receptor (AR)-diffuse strong positive, estrogen receptor (ER)-negative, progesterone receptor (PR)-negative, human epidermal receptor-2 (HER2, c-erbB-2) overexpression, and Ki-67 60% (Figure 3). Additionally, the tumor was positive for GATA binding protein 3 (GATA-3) expression (Figure 4). Fluorescence in situ hybridization (FISH) analysis revealed HER2 gene amplification. Two weeks post-surgery, chemotherapy using the TCbH regimen (docetaxel, 135 mg; carboplatin, 650 mg; trastuzumab, 480 mg) was commenced. Chemotherapy was discontinued after completion of three cycles. After chemotherapy, the patient was listless, but conscious, without nausea and vomiting, abdominal pain and distension, and no fever. The blood routine examination items were within the norm. The patient refused further chemotherapy. Three years after stopping chemotherapy treatment, she experienced lower abdominal pain with cervical bleeding and underwent aspiration biopsy (Figure 5). An enhanced pelvic magnetic resonance scan revealed irregular thickening of the cervix, uneven reinforcement, limited diffusion. The cells were dispersed, not nested, and individual was adenoid. The tumor nuclei were large, hyperchromatic, irregular in shape, and eosinophilic in cytoplasm. Cervical site tumors, first consider whether gynecological primary, then consider whether breast cancer metastases. If the tumor is gynecological primary, it is paired box gene-8 (Pax-8)-positive; if breast cancer has metastasized to the cervix, GATA-3 and gross cystic disease fluid protein-15 (GCDFP-15) are positive. Immunohistochemical results indicated that the tumor was AR-diffuse strong positive, ER-negative, PR-negative, c-erbB-2-negative, Ki-67 30%, Pax-8-negative, GATA-3-diffuse strong positive (Figure 6), and GCDFP-15-diffuse strong positive (Figure 7). Meanwhile, positron emission tomography-computed tomography (PET-CT) showed nodules in the lower lobe of the left lung, about 2.02 cm × 1.38 cm in size, with blurred boundaries and increased radioactive uptake. Therefore, she underwent lung puncture and biopsy (Figure 8), with immunohistochemical results as follows: ER-negative, PR-negative, c-erbB-2-positive, Ki-67 30%, GCDFP-15-diffuse positive and GATA-3-diffuse positive (Figure 9). No HER2 gene amplification was detected by FISH analysis. Based on morphological, immunohistochemical, and clinical findings, a diagnosis of metastasis of ductal breast carcinoma to the uterus and lung was made. She received eight cycles of a chemotherapy regimen comprising albumin paclitaxel (400 mg) + inetetamab (600 mg). Eight months later, she developed a neck mass, and underwent mass puncture and biopsy, which confirmed metastatic breast cancer (Figure 10). Immunohistochemical results were ER-negative, PR-negative, c-erbB-2-positive, Ki-67 30%, trichorhinophalangeal syndrome type 1 (TRPS1)-positive (Figure 11), and GATA-3-positive (Figure 12). The chemotherapy regimen was adjusted to inetetamab 390 mg + EC scheme (EC scheme) for six cycles. The primary tumor in this case was ER-negative and PR-negative, with HER2 amplification. Sometime later, the cervical, pulmonary, and neck mass metastases were ER-negative, PR-negative, and HER2-negative. This is a timeline of the patient’s entire illness (Figure 13). The patient remains alive. The last follow-up was on June 15, 2024, 54 months after radical treatment for breast cancer.






All procedures performed in this study were in accordance with the ethical standards of the research ethics board of The Second Affiliated Hospital of Zhejiang University School of Medicine (Zhejiang, China) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Key findings
Here, we present clinical and pathological data from a rare case of primary breast cancer metastasis to the cervix, lung and neck. In particular, metastasis of breast cancer to the cervix is extremely rare.
Strengths and limitations
Although now we have found a case of breast cancer metastasis to the cervix, how to prevent it is still unknown. It is recommended to do cervical liquid-based cytology and gynecological B-ultrasound every 6 months. Treat any abnormalities as soon as possible.
Comparison with similar researches
Metastasis of non-gynecological tumors to the cervix is a rare event, and metastasis from breast cancer is even more uncommon. To date, only a few cases have been reported; therefore, the true incidence of breast tumor metastasis to the cervix remains unknown (11-13). In 1984, Mazur et al. conducted a study of 325 women with metastatic tumors of the external genitalia and found that, except for cervical metastasis, only 52 were metastatic tumors of breast cancer (14). More recently, Cummings et al. reported that the risk of breast cancer metastases to gynecological sites is higher in young women than that for cervical cancer metastases (4). Lobular carcinoma, with lymph node metastasis and hormone receptor positivity, is prone to metastasis (15). Invasive lobular carcinoma (ILC) is usually negative for HER2, but rarely positive. The status of invasive ductal carcinoma (IDC) HER2 is variable. However, unlike previous reported cases, our patient was an older woman with IDC, negative for both estrogen and progesterone, and HER2-positive. Because the primary tumor is HER2-positive, the patient can receive anti-HER2 targeted therapy for life. Even if some metastases appear negative for HER2, this may be due to tumor heterogeneity (16). In addition, HER2 discordance between primary biopsy and second biopsy after neoadjuvant or adjuvant treatment was observed in 20.7%. This discordance was related only to the use of HER2-targeted treatment (17). In our case, HER2 changes occurred after HER2-targeted treatment also.
Explanations of findings
ILC is the most malignant breast tumor after IDC common. If the ILC is not high grade and is ER-positive at diagnosis, patient prognosis is excellent (18,19); however, compared with IDC, ILC is more likely to metastasize to the female reproductive organs (20). More than 80% of breast cancers that metastasize to the female genital organs are ILC (21), which is more likely to metastasize to the endometrium than IDC, based on data from 13 patients with endometrial metastasis reported from 1984 to 2015 (22).
Cervical metastasis is rare in women with breast cancer, with only 3.7% of patients experiencing metastatic lesions in the reproductive system (23). The cervix is a small organ, primarily composed of dense fibrous muscle, with limited blood supply, and only incoming lymph nodes, making it a disadvantageous location for malignant tumors outside the genital area (24), likely accounting for the rarity of cervical metastasis of breast cancer.
Age is an important factor in breast cancer behavior, with younger patients more prone to liver and gynecological metastasis (4). Further, ILC is hormone sensitive and prone to spreading to the uterus (19).
The most common presentation of uterine metastasis from breast cancer is abnormal uterine metrorrhagia (25), and our case also presented with cervical bleeding. Moreover, numerous studies have demonstrated that the presence of uterine tumor metastasis remains heterogeneous, due to lack of effective diagnostic and therapeutic modalities (22,25). Given its pivotal role in malignant tumors, uterine metastasis significantly contributes to the poor prognosis of patients.
Implications and actions needed
The main treatment for cervical metastasis is surgery, and patients with large lesion circumference are treated using radiotherapy and chemotherapy before operation, to create favorable conditions for surgery. Platinum-containing chemotherapeutic agents can be administered between radiotherapy doses, and supplemented with taxane chemotherapeutic agents after surgery. Endocrine therapy is recommended for patients with ER- and PR-positive tumors. More clinical data from patients with cervical metastasis of breast cancer are required to inform treatment options.
Conclusions
In summary, cervical metastasis is rare in patients with breast cancer, and most commonly presents as vaginal bleeding; however, there may also be no symptoms initially, and regular cervical cytology screening and/or gynecologic ultrasonography can assist in early detection of cervical lesions. Cervical biopsy and pathological examination are the main methods of diagnosis, and immunohistochemistry is also helpful for differential diagnosis.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-24-36/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-24-36/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-24-36/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the research ethics board of The Second Affiliated Hospital of Zhejiang University School of Medicine (Zhejiang, China) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sharma GN, Dave R, Sanadya J, et al. Various types and management of breast cancer: an overview. J Adv Pharm Technol Res 2010;1:109-26. [Crossref] [PubMed]
- Sobinsky JD, Willson TD, Podbielski FJ, et al. Unusual metastatic patterns of invasive lobular carcinoma of the breast. Case Rep Oncol Med 2013;2013:986517. [Crossref] [PubMed]
- Jones GE, Strauss DC, Forshaw MJ, et al. Breast cancer metastasis to the stomach may mimic primary gastric cancer: report of two cases and review of literature. World J Surg Oncol 2007;5:75. [Crossref] [PubMed]
- Cummings MC, Simpson PT, Reid LE, et al. Metastatic progression of breast cancer: insights from 50 years of autopsies. J Pathol 2014;232:23-31. [Crossref] [PubMed]
- Yamada K, Kaneko J, Watahiki M, et al. Endoscopic ultrasound-guided fine-needle biopsy for the diagnosis of gastric metastasis from breast cancer mimicking primary linitis plastica: A case report. DEN Open 2022;2:e115. [Crossref] [PubMed]
- Guzmán-Calderón E. Rectal Metastases from Breast Cancer. A Case Report. J Gastrointest Cancer 2017;48:205-7. [Crossref] [PubMed]
- Algethami NE, Althagafi AA, Aloufi RA, et al. Invasive Lobular Carcinoma of the Breast With Rectal Metastasis: A Rare Case Report. Cureus 2022;14:e23666. [Crossref] [PubMed]
- Bonapasta SA, Gregori M, Lanza R, et al. Metastasis to the Pancreas from Breast Cancer: Difficulties in Diagnosis and Controversies in Treatment. Breast Care (Basel) 2010;5:170-3. [Crossref] [PubMed]
- Banasiewicz T, Krokowicz L, Biczysko M, et al. A case of late breast cancer metastases to both suprarenal glands 28 years after mastectomy. Clin Breast Cancer 2012;12:68-70. [Crossref] [PubMed]
- Pineda A, Sall S. Metastasis to the vagina from carcinoma of the breast. J Reprod Med 1978;20:243-5. [PubMed]
- CRUZ PT. Mammary carcinoma with metastasis to the cervix uteri. Del State Med J 1954;26:304-5. [PubMed]
- Muñoz-Iglesias J, Uña-Gorospe J, Allende-Riera A, et al. Unsuspected uterine metastasis of breast carcinoma diagnosed by 18F-FDG PET/CT. Clin Nucl Med 2013;38:e441-2. [Crossref] [PubMed]
- Benkerroum Z, Babahabib A, Kouach J, et al. Metrorrhagia disclosing a synchronous bilateral breast cancer: report of a case. Gynecol Obstet Fertil 2014;42:360-4. [Crossref] [PubMed]
- Mazur MT, Hsueh S, Gersell DJ. Metastases to the female genital tract. Analysis of 325 cases. Cancer 1984;53:1978-84. [Crossref] [PubMed]
- Bouvier AS, Panchbhaya N, Brochard C, et al. Uterine metastasis from invasive ductal breast carcinoma: A case report with literature review. J Gynecol Obstet Hum Reprod 2021;50:101993. [Crossref] [PubMed]
- Kunte S, Abraham J, Montero AJ. Novel HER2-targeted therapies for HER2-positive metastatic breast cancer. Cancer 2020;126:4278-88. [Crossref] [PubMed]
- Ignatov T, Gorbunow F, Eggemann H, et al. Loss of HER2 after HER2-targeted treatment. Breast Cancer Res Treat 2019;175:401-8. [Crossref] [PubMed]
- Arpino G, Bardou VJ, Clark GM, et al. Infiltrating lobular carcinoma of the breast: tumor characteristics and clinical outcome. Breast Cancer Res 2004;6:R149-56. [Crossref] [PubMed]
- Rakha EA, El-Sayed ME, Powe DG, et al. Invasive lobular carcinoma of the breast: response to hormonal therapy and outcomes. Eur J Cancer 2008;44:73-83. [Crossref] [PubMed]
- Toyoshima M, Iwahashi H, Shima T, et al. Solitary uterine metastasis of invasive lobular carcinoma after adjuvant endocrine therapy: a case report. J Med Case Rep 2015;9:47. [Crossref] [PubMed]
- Ustaalioglu BB, Bilici A, Seker M, et al. Metastasis of lobular breast carcinoma to the uterus in a patient under anastrozole therapy. Onkologie 2009;32:424-6. [Crossref] [PubMed]
- Huo Z, Gao Y, Zuo W, et al. Metastases of basal-like breast invasive ductal carcinoma to the endometrium: A case report and review of the literature. Thorac Cancer 2015;6:548-52. [Crossref] [PubMed]
- Lokadasan R, Ratheesan K, Sukumaran R, et al. Metastatic lobular carcinoma of breast mimics primary cervix carcinoma: two case reports and a review of the literature. Ecancermedicalscience 2015;9:571. [Crossref] [PubMed]
- Bryson CA, de Courcy-Wheeler RH, Wallace RJ. Breast cancer metastasising to the uterine cervix. Ulster Med J 1999;68:30-2. [PubMed]
- Akhtar A, Ratra A, Puckett Y, et al. Synchronous Uterine Metastases from Breast Cancer: Case Study and Literature Review. Cureus 2017;9:e1840. [Crossref] [PubMed]
Cite this article as: Wang X, Wei S. Breast cancer with cervix, lung and neck metastases: a case report and literature review. AME Case Rep 2024;8:102.








