
30 years later—a case report of late surgical clip migration after laparoscopic cholecystectomy
Highlight box
Key findings
• Surgical clip migration is a late complication of laparoscopic cholecystectomy. Endoscopic retrograde cholangiopancreatography is diagnostic and therapeutic after initial assessment with imaging like ultrasound and computed tomography scan.
What is known and what is new?
• Laparoscopic cholecystectomy comes with risk of early and late complications.
• Surgical clip migration can cause obstruction of common bile duct and mimic choledocholithiasis and it can occur as late complication.
What is the implication, and what should change now?
• Surgical clip migration is rare complication which can occur years after cholecystectomy and should be considered as deferential when patients present with concerning symptoms. Our case emphasizes the need for long-term monitoring of cholecystectomy patients to detect such uncommon complications. To address this, physicians and surgeons should be educated about the late and rare compaction and the importance of using fewer clips as possible. In addition to that, diagnostic evaluations for abdominal pain in post-cholecystectomy patient should include consideration of clip migration.
Introduction
Laparoscopic cholecystectomy is the gold standard treatment option for gallbladder disease, with around 750,000 procedures performed every year in the United States (1). Complication rates after laparoscopic cholecystectomy are approximately 3% only. Major post-operation complications include vascular injury, abscess formation, bowel injury, bile leak, and bile duct injury (2). Late complications, which can occur months to years after the surgery, include biliary fistula, recurrent bile duct stones, and bile duct strictures (3). Surgical clip migration has been reported in the literature as a late and uncommon complication (4). The first case was in 1979 following an open cholecystectomy, while the first clip migration complicating a laparoscopic cholecystectomy was in 1992 (5,6). The migrated clip can lead to serious complications such as cholangitis and pancreatitis, but there are no reported mortalities in the literature. In this case report, we describe a patient who presented with acute abdominal pain and was found to have a surgical clip migration 30 years after her laparoscopic cholecystectomy. We present this case in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-24-77/rc).
Case presentation
A 51-year-old female presented with acute upper abdominal pain and associated radiation to the back, worsening with food intake. Further symptoms included chronic burning epigastric pain responsive to antacids. She declined other symptoms, such as fever, nausea, or vomiting. She did not use acetaminophen or other pain medication. The past surgical history was significant for a laparoscopic cholecystectomy in 1992 and a hysterectomy in 2013.
Blood works showed aspartate transaminase (AST) 1,589 U/L, alanine transaminase (ALT) 1,159 U/L, alkaline phosphatase 248 U/L, and total bilirubin 1.8 g/dL with a direct bilirubin of 1.1 g/dL. The basic metabolic panel, complete blood count, and lipase level remained unremarkable. The patient tested negative for a viral hepatitis panel, Epstein-Barr virus, and cytomegalovirus.
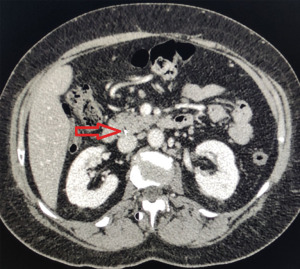
Imaging studies, including hepatic ultrasound and abdominal computed tomography (CT), indicated a dilated common bile duct (CBD) of 1.1 cm with a lodged metallic density within the CBD consistent with a surgical clip (Figures 1,2). Endoscopic retrograde cholangiopancreatography (ERCP) was subsequently performed, which showed a 1 cm free floating clip within the CBD. A 10 mm biliary sphincterotomy was performed, and as balloon extraction failed, a 2 cm × 4 cm basket was used to fragment the stone and retrieve the clip. The post-operative course was uneventful. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report. A copy of the written consent is available for review by the editorial office of this journal.

Discussion
Complications associated with laparoscopic cholecystectomy have been reported to be less than 5%. Late complications are biliary strictures and post-cholecystectomy surgical clip migration which might lead to include intestinal pneumatosis, pneumobilia, and CBD obstruction with stone formation. Despite the increasing number of cholecystectomies performed annually, surgical clip migration remains rare. Intestinal pneumatosis, characterized by gas buildup in the intestinal wall, is a particularly another rare complication after cholecystectomy. The exact pathophysiology of this condition is unclear, but one theory suggests that clips at the ileocecal valve might cause mechanical obstruction and impaired bowel motility, leading to stasis and distension. This environment could promote bacterial overgrowth and gas production, resulting in pneumatosis and pneumobilia (7-9).
This case illustrates an uncommon after cholecystectomy complication known as clip migration. The migration of the surgical clip is recognized as a late complication, occurring on average 26 months after laparoscopic cholecystectomy, with only very few reported cases that occurred after more than ten years (8). This complication is rarely seen, and the current literature illustrates around 100 cases (9,10). Most of the reported cases were in the nineties, following the introduction of laparoscopic cholecystectomy, which reflects the learning curve process (11). The higher the number of clips used, and the degree of cystic duct dissection performed, the higher the clip migration risk (12). If the clip migration occurred early in the postoperative course, it is more likely related to procedure-related factors, including short cystic duct stump, imprecise placement of clips, placement of more than four surgical clips, or local purulent inflammation (8,12).
The underlying mechanism behind the late clip migration remains unclear, with a clip-induced chronic inflammatory process facilitating migration being one potential theory (13). Other possible contributing factors include local necrosis, increased intra-abdominal pressure from any cause, and stone formation over the exposed clip (14). Symptoms commonly encountered with this condition are similar to those of choledocholithiasis, as surgical clip migration is often accompanied by stone formation and subsequent choledocholithiasis (9,12). Furthermore, a migrated metallic clip can lead to recurrent abdominal pain, fever, and sepsis due to acute cholangitis, acute pancreatitis, clip embolism, duodenal ulcer, and obstructive jaundice (15).
The diagnosis of clip margination can be made with different imaging modalities, such as ultrasound, CT scan, or magnetic resonance cholangiopancreatography (MRCP) (16). The condition is usually treated with the use of ERCP to extract of the clip along with sphincterotomy which has a success rate of 85% (8). The presence of certain conditions, like a biliary stricture, fistula, or large stones, may reduce the odds of a successful ERCP intervention and warrant a surgical exploration (8).
Conclusions
Surgical clip migration is a late and rare complication following laparoscopic cholecystectomy. It should be considered as one of the differential diagnoses entertained in patients with a clinical presentation suggestive of choledocholithiasis who have a remote history of cholecystectomy.
Acknowledgments
This case was presented in abstract form at the 2023 American College of Gastroenterology Annual Meeting, 20–25 October 2023, Vancouver, British Columbia, Canada.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-24-77/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-24-77/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-24-77/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Vollmer CM Jr, Callery MP. Biliary injury following laparoscopic cholecystectomy: why still a problem? Gastroenterology 2007;133:1039-41. [Crossref] [PubMed]
- Thurley PD, Dhingsa R. Laparoscopic cholecystectomy: postoperative imaging. AJR Am J Roentgenol 2008;191:794-801. [Crossref] [PubMed]
- Jaunoo SS, Mohandas S, Almond LM. Postcholecystectomy syndrome (PCS). Int J Surg 2010;8:15-7. [Crossref] [PubMed]
- Raoul JL, Bretagne JF, Siproudhis L, et al. Cystic duct clip migration into the common bile duct: a complication of laparoscopic cholecystectomy treated by endoscopic biliary sphincterotomy. Gastrointest Endosc 1992;38:608-11. [Crossref] [PubMed]
- Walker WE, Avant GR, Reynolds VH. Cholangitis with a silver lining. Arch Surg 1979;114:214-5. [Crossref] [PubMed]
- Onghena T, Vereecken L, Van den Dwey K, et al. Common bile duct foreign body: an unusual case. Surg Laparosc Endosc 1992;2:8-10. [PubMed]
- Russo A, Patanè V, Zaccaria C, et al. Imaging diagnosis of a rare case of intermittent intestinal pneumatosis: A consequence of ileocecal valve clip dysfunction? Radiol Case Rep 2024;19:780-4. [Crossref] [PubMed]
- Hamid HKS, Fullard A, Sabahi J, et al. Late biliary endoclip migration after laparoscopic cholecystectomy: Case report and literature review. Int J Surg Case Rep 2020;74:205-8. [Crossref] [PubMed]
- Chong VH, Chong CF. Biliary complications secondary to post-cholecystectomy clip migration: a review of 69 cases. J Gastrointest Surg 2010;14:688-96. [Crossref] [PubMed]
- Aaron E, Palamuthusingam P. Post-cholecystectomy clip migration—a unique method of retrieval. Journal of Surgical Case Reports 2022;2022:rjab640. [Crossref] [PubMed]
- Ghavidel A. Migration of clips after laparoscopic cholecystectomy; a case report and literature review. Middle East J Dig Dis 2015;7:45-9. [PubMed]
- Cetta F, Baldi C, Lombardo F, et al. Migration of metallic clips used during laparoscopic cholecystectomy and formation of gallstones around them: surgical implications from a prospective study. J Laparoendosc Adv Surg Tech A 1997;7:37-46. [Crossref] [PubMed]
- Mateo R, Tsai S, Stapfer MV, et al. Ischemic mass effect from biliary surgical clips. J Laparoendosc Adv Surg Tech A 2008;18:84-7. [Crossref] [PubMed]
- Chong VH, Yim HB, Lim CC. Clip-induced biliary stone. Singapore Med J 2004;45:533-5. [PubMed]
- Ray S, Bhattacharya SP. Endoclip migration into the common bile duct with stone formation: a rare complication after laparoscopic cholecystectomy. JSLS 2013;17:330-2. [Crossref] [PubMed]
- Pang L, Yuan J, Zhang Y, et al. Clip-stone and T clip-sinus: A clinical analysis of six cases on migration of clips and literature review from 1997 to 2017. J Minim Access Surg 2019;15:192-7. [Crossref] [PubMed]
Cite this article as: Najim M, Kusnik A, Rozi W, Devgun S. 30 years later—a case report of late surgical clip migration after laparoscopic cholecystectomy. AME Case Rep 2025;9:5.


